Cardiovascular Problems in Bipolar Disorder May Begin in Adolescence
Adults with bipolar disorder have higher rates of cardiovascular disease and premature death from cardiovascular illness than the general population. At the 2012 meeting of the American Academy of Child and Adolescent Psychiatry, Benjamin Goldstein presented a poster in which he showed that youth with bipolar disorder may also have abnormal cardiovascular function.
When a tourniquet is applied, blood vessels normally expand to make up for the period of oxygen deprivation. This does not happen as readily in patients with mood disorders. This lack of flexibility and compensatory response could be one of the reasons for increased cardiovascular difficulties in those with mood disorders.
In Goldstein’s study, noninvasive ultrasound imaging was used to measure the thickness of the walls of the carotid artery and flow mediated dilation of the artery in adolescents with bipolar disorder and those without the illness. The data was collected by a certified ultrasound technologist who remained blind to the patients’ diagnostic and symptom status.
Goldstein found highly abnormal results in 14 adolescents aged 14 to 19 with bipolar disorder compared to controls. He concluded that reducing cardiovascular risk in bipolar disorder is a pressing clinical and public health challenge and that treating these patients while they are adolescents may offer considerable advantages both for prevention and for understanding the progression of cardiovascular problems in patients with bipolar disorder.
Substance Use Among Canadian Adolescents with Bipolar Disorder: The Critical Need for Intervention and Prevention
At the 2012 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP), Antoinette Scavone presented a poster on correlates of substance use disorders among Canadian adolescents with bipolar disorder. Participants were 62 adolescents aged 14 to 19 with bipolar disorder. Twenty-three participants (37.1%) had a substance abuse disorder.
Those with a comorbid substance use disorder were more likely to have a comorbid panic disorder or an oppositional defiant disorder. They also had higher rates of police contact or arrest, were more likely to have been involved in assault, and were more impulsive. In addition they had experienced more stressful life events.
Editor’s Note: These data from a Canadian sample replicate previous findings in the US and again indicate the critical importance of preventing the onset of substance abuse in adolescents at especially high risk because of their bipolar disorder.
The Explosive Combination of Bipolar Disorder and Substance Abuse
At the 2012 annual meeting on pediatric bipolar disorder sponsored by the Ryan Licht Sang Foundation and Massachusetts General Hospital, Timothy E. Wilens gave a plenary talk on “The Explosive Combination of Bipolar and Substance Abuse.”
Wilens cited the statistic that 10% of adolescents in the general US population have at some time received a diagnosis of a substance abuse disorder. The age of onset of substance abuse peaks between ages 15 and 20.
Wilens said that in a recent survey about use in the past month, among participants in the general population aged 12 or higher with substance use, about 50% use marijuana and about 50% use prescription narcotics (often obtained from their parents’ medicine chest).
The rate of mortality from substance abuse has risen dramatically since 1993 and now approximates that from automobile accidents. According to Wilens, rates of emergency room visits and fatalities have increased recently, and this has been linked to opiate overdoses.
Adolescents with bipolar disorder are at greatly increased risk of substance abuse compared to the general population. Most substance abuse follows the onset of bipolar disorder, not vice versa.
Wilens cited the data of researcher Ben Goldstein that on 8-year follow up, 32% of bipolar adolescents developed a substance use disorder. Those treated with antimanic agents were much less likely to develop a substance use disorder. MORAL: Treat bipolar disorder psychopathology in adolescents well and help them avoid substance abuse.
Children with persistent emotion dysregulation were: 1) more likely to develop a substance use disorder; 2) more likely to begin using substances earlier; and 3) more likely to have a more severe form of combined (multiple) substance use disorders.
Treating Substance Use
Wilen suggested that a good interview is better than urine toxicology screens for assessing substance use. He suggested the following treatment paradigm: Read more
Sleep Apnea Common Among Rapid Cyclers
Kellen and colleagues presented a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, in which they reported that 21% of patients with rapid cycling bipolar disorder have confirmed sleep apnea. Since many patients who screened positive for sleep apnea on the study’s sleep questionnaire did not undergo follow-up sleep studies to confirm the diagnosis, it is estimated that up to 40% of rapid cycling patients may, in fact, have sleep apnea.
Editor’s note: Given such a high incidence of sleep apnea among rapid cycling bipolar patients, it would be prudent for patients and clinicians to be alert to the possibility of sleep apnea and follow up with appropriate sleep studies. Sleep apnea can cause daytime fatigue, cognitive dysfunction, and treatment resistance, so its identification and treatment with continuous positive airway pressure (CPAP) may be enormously beneficial to a substantial number of rapid cycling bipolar patients. A just-published article by Sukys-Claudino in Sleep Medicine presents findings that compared to placebo, the anti-Alzheimer’s drug donepezil (Aricept) started at 5mg/day for 2 weeks and then increased to 10 mg given twice a day (20 mg/day total) helped all measures of sleep apnea including daytime sleepiness.
Clinical hints that a patient may be suffering from sleep apnea include loud snoring, long pauses between breaths, and non-restorative sleep. The likelihood of sleep apnea increases with age and with overweight or obesity.
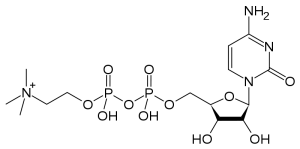
The Natural Substance Citicoline May Be Useful in Bipolar Disorder with Comorbid Stimulant Abuse
Sherwood Brown and colleagues from the University of Texas Southwestern Medical Center have completed a successful placebo-controlled trial of citicoline for bipolar and unipolar depression with comorbid methamphetamine dependence. Forty-eight participants with methamphetamine dependence and either unipolar or bipolar depression were randomized to either citicoline (2000 mg/day) or placebo for 12 weeks. Those receiving citicoline had significantly greater improvement in scores on the Inventory of Depressive Symptoms compared with those who received placebo, and patients receiving citicoline stayed in the study significantly longer, with completion rates of 41% on citicoline and 15% on placebo.
In 2007, the same team of investigators reported in the Journal of Clinical Psychopharmacology that citicoline had positive effects in bipolar patients with cocaine dependence, who experienced significant decreases in cocaine use and fewer cocaine-positive urine tests while taking citicoline.
Uric Acid Increases During Mania
At the 65th Annual Scientific Convention of the Society of Biological Psychiatry this year, Giacomo Salvadore reported that significantly higher levels of uric acid are found in patients with mania compared with normal controls.
Editor’s note: This study was particularly interesting because there was a highly significant difference between patients and controls, with very few values overlapping. The data suggest the possibility that uric acid may be a useful biological marker for mania, and is one that should be studied in childhood-onset bipolar illness to determine whether uric acid is a marker for mania in children as well.
Allopurinol, a widely used treatment for gout that reduces levels of uric acid in the blood, is an effective antimanic agent (based on data from two placebo-controlled studies, one by Machado-Vieira et al. and one by Akhondzadeh et al.). The new data on uric acid raise the possibility that high levels of uric acid may be a specific predictor of responsiveness to Allopurinol, although this hypothesis has not yet been explored.
In an article by Chung et al. just published in Psychiatry Research, it was reported that in a very large epidemiological study in Taiwan, patients with bipolar disorder have increased risk of gout.
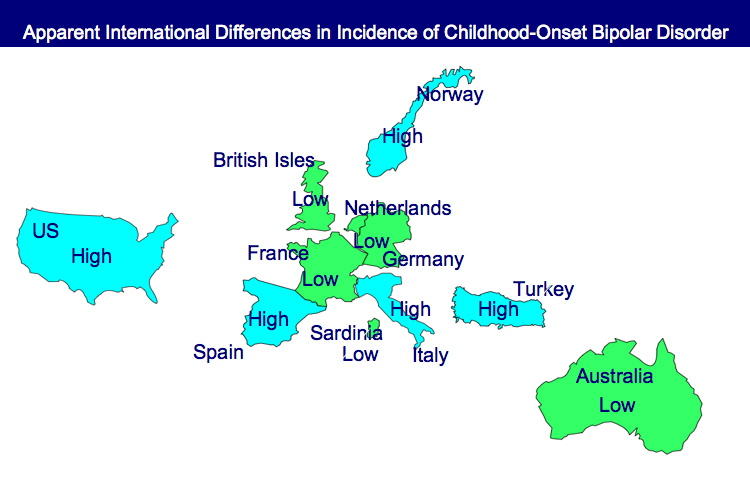
Bipolar Disorder Worse in US than Europe
New research shows that there are more early onsets of illness and more difficult courses of bipolar illness in the US than in the Netherlands or Germany.
This editor was invited to give a plenary presentation at the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March. The talk, titled “A greater incidence of early onset bipolar illness and poor prognosis factors in patients in the US compared with those in The Netherlands and Germany,” was based on studies in our Bipolar Collaborative Network.
We found that patients who were studied and treated at four sites in the US (Los Angeles, Dallas, Cincinnati, and Bethesda) had more poor-prognosis factors and indices of difficult courses of bipolar illness compared with patients studied in the same fashion at three sites in Utrecht, the Netherlands and Freiberg and Munich, Germany. We presented some of these data in a preliminary report in the British Journal of Psychiatry in 2008 and further analyzed these data for an article published last year in the Journal of Clinical Psychiatry. Read more
Smoking Multiplies Risks for Bipolar Patients
Smoking is associated with a less successful outcome in the naturalistic treatment of bipolar patients, reported Seetal Dodd and colleagues at the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March. Nicotine dependence has also been found to be a risk factor for depressive symptoms, as reported in a recent article in the British Journal of Psychiatry.
In addition to these direct effects on mental health, smoking is also a major risk factor for cardiovascular disease when combined with the presence of any three of the five primary risk factors that constitute the metabolic syndrome. (These five factors are: increased waist circumference, high blood pressure, increased cholesterol, increased triglycerides, and insulin resistance or elevated fasting blood glucose.) Cardiovascular disease co-occurs with bipolar disorder at a high rate and is one of the major causes of decreased life expectancy in those with inadequately treated illness.
Because smoking is a powerful risk factor for comorbid illnesses such as heart attack and stroke and is itself associated with a poor clinical outcome in the treatment of bipolar disorder, every effort should be made to help patients with smoking cessation. Suggestions after the jump. Read more
Inflammation in the Affective Disorders
Bipolar children exhibit more inflammation than healthy children, according to a paper presented by Pandey, Dwivedi, and Pavuluri from the University of Illinois at the American College of Neuropsychopharmacology in December 2009.
In “Pro-inflammatory cytokines in plasma of patients with pediatric bipolar disorder,” the researchers described their study in which 21 normal controls were compared with 22 children with pediatric bipolar disorder who were unmedicated for a period of at least two weeks. The level of the inflammatory cytokine interleukin-1b (IL-1b) was significantly higher in the pediatric bipolar patients compared with controls, and levels of TNF alpha, another inflammatory marker, were significantly higher as well. Not only is this evidence of increased inflammatory processes in pediatric bipolar disorder, but TNF alpha is associated with activation of transcription factors and the initiation of preprogrammed cell death, or apoptosis.
More Medical Comorbidities Among Bipolar Population
Goldstein and colleagues interpreted data from the National Epidemiological Survey in 2001-2002 that included 41,682 representative adults in the U.S. population sampled compared with 1,411 found in the community with a diagnosis of bipolar disorder.
Those with bipolar disorder had a 3.86 times higher odds of having coronary heart disease compared with those in the general population. They were also 2.15 times more likely to have hypertension. Most disturbingly, the mean age of those with coronary heart disease in the general population was 62.1 years of age, but in those with bipolar illness, it was 50.4 years of age. This indicates that the markedly increased risk and incidence of coronary artery disease occurred approximately 11 years earlier in those with bipolar illness compared with those without. Most interestingly, the number of prior depressive episodes correlated with the presence of either coronary heart disease or hypertension.