6 Minutes of Intense Cycling Produces Major Increases in BDNF
Brain derived neurotrophic factor (BDNF) is necessary for new synapses and call survival. A new study in J. Physiology (2023) reports that the increases in BDNF from short intense cycling exercise are much greater than from prolonged (90-minute) light cycling. The authors think that this is cause by the increases in lactate produced which helps up regulate BDNF production. This could be good for fighting depression and Alzheimer’s disease, where BDNF levels are low.
Bottom line: If you don’t have much time, bust your buns.
Chronic Fatigue, Depression and Anxiety Symptoms in Long COVID Are Strongly Predicted by Neuroimmune and Neuro- Oxidative Pathways Which Are Caused by the Inflammation during Acute Infection
HK Al-Hakeim et al in Michael Maes’ lab report in J. Clinical Medicine (2023) on very important findings about immune and oxidative changes in long COVID with “physio- somatic (chronic fatigue syndrome and somatic symptoms) and affective (depression and anxiety) symptoms. The severity of the long COVID physio-affective phenome is largely predicted by increased peak body temperature (BT) and lowered oxygen saturation (SpO2) during the acute infectious phase….. We recruited 86 patients with long COVID (3–4 months after the acute phase) and 39 healthy controls and assessed serum C-reactive protein (CRP), caspase 1, interleukin (IL) 1?, IL-18, IL-10, myeloperoxidase (MPO), advanced oxidation protein products (AOPPs), total antioxidant capacity (TAC), and calcium (Ca), as well as peak BT and SpO2 during the acute phase. Results: Cluster analysis revealed that a significant part (34.9%) of long COVID patients (n = 30) show a highly elevated NT (neurotoxicity) index as computed based on IL-1?, IL-18, caspase 1, CRP, MPO, and AOPPs. Partial least squares analysis showed that 61.6% of the variance in the physio-affective phenome of long COVID could be explained by the NT index, lowered Ca, and peak BT/SpO2 in the acute phase and prior vaccinations with AstraZeneca or Pfizer. The most important predictors of the physio-affective phenome are Ca, CRP, IL-1?, AOPPs, and MPO. Conclusion: The infection–immune–inflammatory core of acute COVID-19 strongly predicts the development of physio-affective symptoms 3–4 months later, and these effects are partly mediated by neuro-immune and neuro-oxidative pathways.”
Editors Note: These finding are important as they may lead to new treatment interventions. BNN readers are reminded of a previous BNN article by investigators from Yale (written by by Isabella Backman on Dec. 13, 2022) that in a new case study, they found that guanfacine plus N-acetylcysteine (which is an anti-inflammatory, anti-oxidant, and glutathione precursor) “mitigated and sometimes eliminated the cognitive impairment known as “brain fog” that often accompanies long COVID.
Adolescent Delta-9-tetrahydrocannabinol induces long-term neuronal disturbances in dorsal vs. ventral hippocampus
De Felice et al reported in Neuropsychopharmacology (2022) how adolescent THC exposure in a rodent model can induce significant morphological disturbances and glutamatergic signaling abnormalities in the hippocampus. The dorsal hippocampus is critical for cognitive and contextual processing, whereas the ventral region is critical for affective and emotional processing. Adolescent THC exposure induces long-lasting memory deficits and anxiety like-behaviors concomitant with a wide range of differential molecular and neuronal abnormalities in dorsal vs. ventral hippocampal regions.
Editors Note: While these data are in rodents, they provide insights into how THC use in adolescents exerts memory deficits and anxiety-like behavior in adulthood by dysregulation of glutamate signaling in the hippocampus. These data converge with data in humans. The bottom line is: use of marijuana in adolescence is not good for brain function, cognition, and behavior in adulthood.
A NEW VIEW ON MEMORY TO REMEMBER
Steven Ramirez PhD of Boston University gave a talk (8/9/22) on memory for the BBRF hosted by Jeffrey Borenstein President & CEO of the Brain & Behavior Research Foundation. Ramirez showed that positive (food) and negative (shock) memories of different places were stored in different neurons of the hippocampus. If he turned on the positive memories with optical stimulation while a mouse was in a negative memory place and would ordinarily show freezing representing fear behavior, much less freezing occurred with the insertion of the positive memory. Positive memories appear to trump negative memories.
Ramirez found score of genes were activated or turned off in the positive memory cells, some of which, but not all, overlapped with the negative memory cells. Remarkably, the bulk of the unique positive memory genes were related to synaptogenesis and neuroprotection, while the bulk of genes unique to the negative memory cells were related cell death and other toxic factors. Ramirez hopes these data will provide clues to not only helping people with PTSD, but also ultimately providing targets for providing protection against degenerative diseases.
When Ramirez was asked by Borenstein what people could do now, he related his own experience of every morning filling out a form for gratitude and gratefulness for at least 3 things he could be grateful for the previous day or anticipated for the current day. The positive memories that this invoked in him set up his positive and optimistic attitudes for the rest of the day. He recommends this approach of positive memories modulating the current pervasive stressors of the day. For people interested in the details of his experiments summarized above, they should look for the in press articles of Grella et al Nature Communications and Shpokayte et al Nature Communications.
Review Describes Latest Findings on the Mechanisms of Psychedelic Drugs and Their Therapeutic Potential
In a 2021 review article in a special issue of the Journal of Neurochemistry devoted to “Psychedelics and Neurochemistry,” researcher Alaina M. Jaster and colleagues summarized recent findings on psychedelic drugs, including their potential as treatments for psychiatric disorders and the structural changes they produce in the brain. The review article focused on findings in humans and provided background context based on findings in animals, particularly rodents.
In the article, Jaster and colleagues write that psychedelics “have in common a battery of acute (within minutes to hours) effects in humans that include profound changes in processes related to perception, cognition, sensory processing, and mood.” They are not considered to be addictive, and recent research has identified fast-acting and long-lasting therapeutic effects of psychedelics, particularly for the treatment of depression and substance abuse.
While psychedelic drugs interact with the brain in complicated ways, the role of serotonin 5-HT2A receptors seems to be crucial to their effects. Psychedelics have classically been divided into two groups based on their chemical structures: phenethylamines (which include mescaline and its synthetic analog DOI) and tryptamines (which include psilocybin/“magic mushrooms,” DMT/ayahuasca, and ergolines like LSD, which are sometimes separated into a third category). The authors of the review highlight that other substances with different chemical structures that do not fit into this classification can also function as psychedelics. Examples include efavirenz and quipazine, which both activate serotonin 5-HT2A receptors and change rodent behavior in the same way that other psychedelic drugs do. These drugs are providing new directions for research into how psychedelics work at both serotonin 5-HT2A receptors and monoaminergic G protein-coupled receptors (GPCRs).

Rodent studies are often used to investigate how psychedelic drugs work. Rodent behaviors such as ear scratching and head twitching increase when the rodents are given drugs that have psychedelic effects in humans. These behaviors return to normal when rodents are given drugs that function as serotonin 5-HT2A receptor antagonists, preventing the stimulation of these serotonin receptors.
While it has been established that serotonin 5-HT2A receptors play an important role in the hallucinogenic effects of psychedelic drugs, how serotonin receptors are involved in some of the therapeutic effects of psychedelics, such as antidepressant effects and changes to synaptic plasticity, is not yet clear.
According to the review, “A number of studies in animal models as well as postmortem human brain samples from subjects with depression and controls has provided evidence that mood disorders occur in conjunction with a reduction in the density of dendritic spines, particularly in the frontal cortex.” Dendrites are the projections from the cell bodies of neurons upon which nerve endings from the axons of other neurons synapse. The surface of these dendrites is covered in mushroom-shaped spines that help create these synaptic connections. The review describes in vitro and in vivo research on mice that suggests that the psychedelics DOI, DMT, and LSD can remodel dendritic spines.
At a recent scientific meeting, researcher Javier González-Maeso, one of the authors of the review, described findings from a recent study of mice given DOI. The structure of the dendritic spines in the prefrontal cortex changed rapidly in these mice. They had also been conditioned to produce a fear response, and the extinction process to get rid of this learned fear was sped up in the mice given DOI. These effects occurred via the serotonin 5-HT2 receptors. The exposure to the psychedelic also affected the regulation of genes involved in synaptic assembly for days, suggesting that epigenetic-induced changes in synaptic plasticity may underlie some of the long-lasting therapeutic effects of psychedelics.
The review also addressed “microdosing,” the recreational practice of consuming small amounts of psychedelics such as psilocybin or LSD, based on the theory that amounts too small to create a hallucinogenic effect may instead produce therapeutic results. The authors find limited data to support microdosing. Most studies in humans and rodents have found no effect or, in the case of one rat study, a worsening of dendritic spine density following microdosing.
Surface Area of Cortex Is Reduced After Multiple Manic Episodes
In a 2020 article in the journal Psychiatric Research: Neuroimaging, researcher Rashmin Achalia and colleagues described a study of structural magnetic resonance imaging (MRI) that compared 30 people with bipolar I disorder who had had one or several episodes of mania to healthy volunteers. Compared to the healthy volunteers, people with bipolar disorder had “significantly lower surface area in bilateral cuneus, right postcentral gyrus, and rostral middle frontal gyri; and lower cortical volume in the left middle temporal gyrus, right postcentral gyrus, and right cuneus.”
The surface area of the cortex in patients with bipolar I disorder who had had a single episode of mania resembled that of the healthy volunteers, while those who had had multiple manic episodes had less cortical surface area.
The data suggest that compared to healthy volunteers, people with bipolar disorder have major losses in brain surface area after multiple episodes that are not seen in first episode patients. In addition, the researchers found that both the number of episodes and the duration of illness was correlated with the degree of deficit in the thickness in the left superior frontal gyrus. These decreases in brain measures occurred after an average of only 5.6 years of illness.
Editor’s Note: These data once again emphasize the importance of preventing illness recurrence from the outset, meaning after the first episode. Preventing episodes may prevent the loss of brain surface and thickness.
Clinical data has also shown that multiple episodes are associated with personal pain and distress, dysfunction, social and economic losses, cognitive deficits, treatment resistance, and multiple medical and psychiatric comorbidities. These and other data indicate that treatment after a first episode must be more intensive, multimodal, and continuous and include expert psychopharmacological and psychosocial support, as well as family education and support. Intensive treatment like this can be life-saving. The current study also supports the mantra we have espoused: prevent episodes, protect the brain and the person.
Left Prefrontal Strokes Linked to Depression

In a 2021 article in the journal Stroke, researcher Julian Klingbeil and colleagues reported that left, but not right, ventrolateral prefrontal stroke lesions were associated with increased risk of depression at six months post-stroke.
The study included 270 participants who had their first-ever stroke. Six months following their strokes, 19.6% of the participants had depression. Those who scored higher on a scale of depression and anxiety symptoms in the first month after their stroke were more likely to have depression six months after the stroke.
The researchers identified a cluster of locations for stroke lesions, mostly within the left ventrolateral prefrontal cortex, that they linked to depression symptoms six months post-stroke. Klingbeil and colleagues hope that recognizing lesions in this region as risk factors for depression will help with early diagnosis of depression among people who recently had a stroke.
Editor’s Note: Antidepressants have been shown to improve post-stroke recovery of neurological functional (and depression) that is caused by the cutoff of blood supply during a stroke (ischemia). Patients and their family members should talk with their neurologist about treatment of ischemic strokes with antidepressants, especially when the lesions occur on the left side of the brain.
White Matter Disturbances in Bipolar Disorder
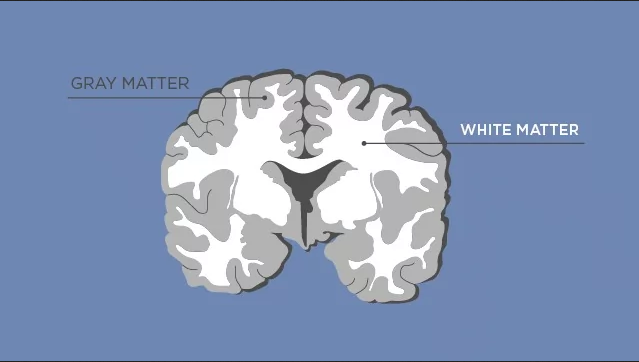
At the 2020 meeting of the International Society for Bipolar Disorders, researcher Clare Beasley described the cellular and molecular underpinnings of the white matter abnormalities typically seen in children and adults with bipolar disorder. Researchers consistently see white matter abnormalities in neuroimaging studies of bipolar disorder, but not much is understood about what creates these deficits.
Beasley and colleagues studied autopsy specimens and found that compared to controls, people with bipolar disorder had a number of abnormalities affecting glial cells, lipid composition, and axons.
The researchers found increased density of oligodendrocytes (glial cells that produce the myelin that wraps around axons, the long fibers of nerve cells where impulses travel out to other cells) and an associated protein called CNP in the prefrontal cortex. The myelin is what makes up white matter, while gray matter consists of cell bodies of neurons and glial cells.
People with bipolar disorder also had differently-shaped astrocytes, another type of glial cell that abuts synapses. The researchers found changes in lipid composition, including phospholipid and fatty acid levels, in the white matter of people with bipolar disorder. There were also problems with axons. Beasley and colleagues noted lower density of axon-associated proteins, which are involved in transport of substances along the axons in people with bipolar disorder.
The authors conclude that these data implicate specific disturbances in oligodendrocytes and axonal function associated with the white matter alterations usually seen in neuroimages of people with bipolar disorder.
Endocannabinoid System May Help Explain Tourette Syndrome

Endocannabinoids are neurotransmitters produced by the human body that attach to cannabinoid receptors in the brain, the same receptors that are affected by the consumption of cannabis products.
Tourette syndrome, a neurodevelopmental disorder characterized by tics and psychological symptoms, is probably caused by some dysfunction involving the neurotransmitter dopamine. The syndrome is usually treated with dopamine receptor blockers but is also eased by cannabis use and treatment with THC, the main psychoactive component in cannabis. Recently, researchers set out to determine whether concentrations of endocannabinoids in the cerebrospinal system are related to Tourette syndrome.
In an article published in the journal Neuropsychopharmacology in 2020, researcher Kirsten R. Müller-Vahl and colleagues report that endocannabinoid concentrations were significantly higher in the cerebrospinal fluid of 20 people with Tourette’s syndrome than in 19 control participants without Tourette’s.
The researchers found elevations in the endocannabinoids AEA and 2-AG, the endocannabinoid-like ligand PEA, and the metabolite AA in the participants with Tourette’s syndrome. Levels of 2-AG in the cerebrospinal fluid correlated with severity of attention-deficit hyperactivity disorder symptoms, an aspect of the syndrome.
It is possible that higher concentrations of endocannabinoids are present in the syndrome because they compensate for the overactive influence of dopamine. This explanation would fit with the effectiveness of cannabis in treating Tourette’s. However, that has not yet been determined, and it is also possible that the endocannabinoids are a reaction to dysfunction involving other neurotransmitters, are incidental to the syndrome, or in the best case that they are a direct cause of the syndrome.
Müller-Vahl and colleagues suggest that based on the effectiveness of cannabis in treating Tourette’s, it may turn out that the syndrome is a sort of endocannabinoid deficiency. They believe this hypothesis is not counteracted by the high levels of cannabinoids they found in Tourette’s patients in this study, because these high levels may be accompanied by a reduced number or reduced sensitivity of the cannabinoid receptors or overactivity in the enzymes that break down endocannabinoids, such that it is difficult to maintain normal levels of these neurotransmitters.
Translocator Protein Levels in Brain Predict Response to Anti-Inflammatory Celecoxib in Major Depressive Disorder
Gliosis describes changes in glia that result from damage to the central nervous system. Researchers can use PET scans (positron emission tomography) to measure the extent of gliosis in the brain. But a new study explored whether these PET scans could instead be used to determine who might respond to a given medication.
Researcher Sophia Attwells and colleagues reported in the journal Biological Psychiatry in 2020 that people with high levels of translocator protein (TSPO), a measure of gliosis and inflammation, had a better antidepressant response to the anti-inflammatory drug celecoxib than patients who started out with lower levels of TSPO.
The study participants, who had treatment-resistant depression, all received 200mg of the anti-inflammatory drug celecoxib twice/day for eight weeks on an open (non-blind) basis. Before they began taking celecoxib, the participants received PET scans to measure translocator protein total distribution volume (TSPO VT) in the prefrontal cortex and the anterior cingulate cortex.
Patients with high levels of TSPO showed greater reductions in depression ratings over the course of the study than those with normal levels of TSPO at baseline.
Attwells and colleagues conclude that “this personalized medicine approach of matching a marker of gliosis to [an anti-inflammatory treatment] …should be applied in early development of novel therapeutics, in particular for [treatment-resistant depression].”
Editor’s Note: These findings are of considerable importance, as they are among the first to indicate that measures of inflammation may predict response to an anti-inflammatory medication such as celecoxib. In a 2013 article in the journal JAMA Psychiatry, Charles L. Raison and colleagues reported that patients with high levels of the peripheral inflammatory marker CRP saw marked improvement in their depression when they received the anti-inflammatory treatment infliximab while those with lower or normal levels of inflammation actually worsened.

