Primary Care Doctors Important in Detecting and Managing Childhood Mental Illness
The National Alliance on Mental Illness (NAMI) conducted a survey to determine ways that primary care providers can better communicate with parents about a child’s mental illness. In a news release NAMI executive director Michael Fitzpatrick said, “Most Americans rely on family doctors and pediatricians for early detection of mental illness and in many cases treatment.”
NAMI concluded that primary care providers could play a larger role in detecting mental illness in children. They found that in 63% of families, the first signs of behavioral or emotional problems were evident in children by age 7. More than half of families reported that their primary care physicians were not knowledgeable about mental health treatments. Almost two-thirds of families reported that their primary care providers were not knowledgeable about local resources to support families with mentally ill children.
NAMI’s suggestions for primary care providers included educating themselves about early-onset mental illness and local resources for families, providing screening tools for parents and youth in order to encourage discussion of mental health, emphasizing that mental health is as important as physical health to a child’s wellbeing, asking questions about mental health as a routine part of office visits, and listening to families’ concerns without judgment.
Primary care providers are also encouraged to let families know that there is hope and that they are not alone in facing this difficulty, that mental illness in a child is not the parents’ fault, and that their children have many strengths.
Primary care doctors should also be prepared to: refer a mentally ill child to psychiatrists, psychologists, and other specialists if needed; follow up, including collaborating with other healthcare providers to develop and implement a treatment plan; and encourage patients and their families.
Risks and Difficulties of Treating Childhood-Onset Bipolar Disorder
 Early treatment is needed in childhood onset bipolar disorder
Early treatment is needed in childhood onset bipolar disorder
Multiple factors make childhood-onset bipolar disorder a difficult problem for affected children and families. Early onset is common, and treatment is often delayed or inappropriate. It takes an average of nine months to achieve remission, and relapses are common. In studies children have remained symptomatic for an average of two-thirds of the time they receive naturalistic follow up treatment, and the illness impairs social and educational development. Episodes and stressors tend to accumulate, and substance abuse is a frequent complication. Dysfunction and disability occur at a high rate among children with the illness, and suicidal ideation and acts are common.
When we surveyed adults in our treatment network, the Bipolar Collaborative Network (BCN), about the history of their illness, we found that the duration of the time lag between illness onset and first treatment was independently related to a poor outcome in adulthood. A longer delay to first treatment was associated in adulthood with greater depression severity, more days depressed, fewer days euthymic, more episodes, and more ultradian cycling (or cycling within a single day). Because treatment delay is a risk factor that can be avoided or prevented, efforts should be made to initiate treatment early in the course of bipolar illness. Read more
Almost 40% of Children with Bipolar Disorder May Not Receive Necessary Treatment
 An article by Geller et al. in Bipolar Disorders last year illustrates the crisis in the treatment of childhood-onset bipolar illness in the US. The article indicates that almost 40% of the children with a credible diagnosis of bipolar disorder in this study never received anything near the appropriate treatment for their illness.
An article by Geller et al. in Bipolar Disorders last year illustrates the crisis in the treatment of childhood-onset bipolar illness in the US. The article indicates that almost 40% of the children with a credible diagnosis of bipolar disorder in this study never received anything near the appropriate treatment for their illness.
It is unfortunate when children fail to receive appropriate treatment because of ambiguity about a diagnosis, but it is even more frustrating when one of the world’s experts makes a diagnosis, and a child still fails to receive treatment based on consensus guidelines.
Over 8 years of follow-up treatment in their communities, these very ill children not only did not receive helpful drugs such as atypical antipsychotics or mood stabilizers, but they often received treatments that can be counterproductive, such as antidepressants or psychomotor stimulants. Those children who did receive appropriate treatment with lithium fared better and recovered significantly earlier than the others. Read more
Treatments Studies for Childhood Onset Bipolar Illness Are Inadequately Funded
It was remarkable that at the Pediatric Bipolar Conference hosted by Massachusetts General Hospital (MGH) and the Ryan Licht Sang Bipolar Foundation this past March in Cambridge, Massachusetts, none of the plenary talks, although they were excellent and given by leaders in the field of child psychiatry, dealt directly with the topic of the conference–childhood-onset bipolar disorder. There were also no reports of systematic placebo-controlled clinical trials evaluating treatment approaches in any of the subsequent presentations or posters. A number of open and uncontrolled studies examined new treatment possibilities.
It is notable that the National Institute of Mental Health (NIMH) no longer sponsors this conference, as it did for many years. Moreover, STEP-BD, an NIMH-sponsored research program on the course and treatment of adult-onset bipolar disorder, is now defunct, and the head of STEP-BD and one of the most productive researchers in bipolar illness, Andrew Nierenberg from the MGH, has been forced to search for other funding opportunities.
These developments highlight the ongoing deficient funding and study of both childhood-onset and adult-onset bipolar disorder despite the enormous public health impact, extraordinary morbidity, and early mortality from suicide and medical illnesses like cardiovascular disease that are associated with these disorders.
Help the Child and Adolescent Bipolar Foundation win $250,000!
The Child and Adolescent Bipolar Foundation (CABF) has launched a campaign for votes to win the Pepsi Refresh Project and a $250,000 grant to aid families and children living with bipolar disorder and depression. CABF has been chosen to compete for the top grant during the month of November. Winners are decided by total votes cast via Internet and text messages throughout the month.
If selected by popular vote, CABF will use an innovative
social media awareness effort to:
- Elevate awareness about bipolar disorder & depression in children;
- Educate parents & the public about the symptoms;
- Explain the best treatment options & ways to reduce teen suicide;
- Expand the number of children receiving treatment;
- Eliminate the stigma associated with mental illness;
- Extend hope to families struggling with mental illnesses.
Supporters can vote for CABF 3 times a day, once from
each of the following sources:
1. Pepsi Refresh website
2. Facebook
3. Texting – Text 104174 to PEPSI (73774) (Normal text
rates apply).
5 Myths About Unipolar Depression
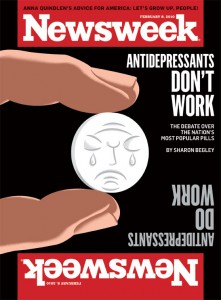 Early this year, news stories such as Newsweek’s “The Depressing News About Antidepressants” and “Antidepressant Drug Effects and Depression Severity” in the Journal of the American Medical Association (JAMA) created an inadequate picture of the seriousness of clinical depression, and the importance of preventing recurrent episodes with long-term antidepressant treatment. (For a rebuttal, see Psychiatric Times.)
Early this year, news stories such as Newsweek’s “The Depressing News About Antidepressants” and “Antidepressant Drug Effects and Depression Severity” in the Journal of the American Medical Association (JAMA) created an inadequate picture of the seriousness of clinical depression, and the importance of preventing recurrent episodes with long-term antidepressant treatment. (For a rebuttal, see Psychiatric Times.)
The consequences of this distorted depiction of depression and its treatment are potentially dire for individuals’ health. Some of the popular myths about depression deserve critical review so that patients can make more informed decisions about their own treatment.
Myth 1: Depression is all in your mind
Myth 2: Depression is over-treated
Myth 3: Antidepressant efficacy barely exceeds that of placebo
Myth 4: Antidepressants should be stopped as soon as possible
Myth 5: Depression is a minor medical problem
Myth 1: Depression is all in your mind
This might seem valid, since depression is classified as a mental illness. But depression is not abstract, imaginary, or lacking a solid physical foundation. There is now overwhelming evidence that depression coincides with disturbances in multiple brain and body systems.


