Cortex Shrinks and Amygdala Grows in Childhood Bipolar Disorder
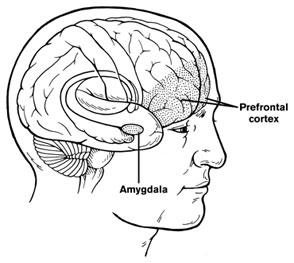 At a symposium on new research on juvenile bipolar disorder at the meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) in 2010, the discussant Kiki Chang of Stanford University reported some recent neurobiological findings on childhood bipolar disorder. He found evidence that prefrontal cortical volume appears to decrease over the course of the illness and, conversely, there was evidence of increases in amygdala volume. He also found that the volume of the striatum (or caudate nucleus, which is involved in motor control) increased in children with bipolar illness or bipolar illness comorbid with ADHD, but decreased in children with ADHD alone.
At a symposium on new research on juvenile bipolar disorder at the meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) in 2010, the discussant Kiki Chang of Stanford University reported some recent neurobiological findings on childhood bipolar disorder. He found evidence that prefrontal cortical volume appears to decrease over the course of the illness and, conversely, there was evidence of increases in amygdala volume. He also found that the volume of the striatum (or caudate nucleus, which is involved in motor control) increased in children with bipolar illness or bipolar illness comorbid with ADHD, but decreased in children with ADHD alone.
Chang cited the study of Singh et al. (2010) who found that the subgenual anterior cingulate volume early in the course of illness was smaller in adolescent-onset bipolar disorder compared to controls. Given this evidence of prefrontal cortical and anterior cingulate deficits, Dr. Chang raised the possibility that treatment with lithium and other agents with potential neurotrophic and neuroprotective effects might be able to prevent these neurobiological aspects of illness progression in young patients.
BP-NOS Often Develops Into Bipolar I or II Disorder
At a symposium on new research on juvenile bipolar disorder at the meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) in 2010, David Axelson of the University of Pittsburgh summarized the longitudinal course of sub-syndromal bipolar disorder in children and adolescents as observed in a research program called COBY (Course and Outcome of Bipolar Youth). Axelson called attention to the 35% of the bipolar spectrum children who had a diagnosis of bipolar NOS (not otherwise specified) as opposed to the 58% who had full-blown bipolar I illness. BP-NOS is defined as illness not meeting criteria for bipolar I or II, including duration of illness and number of symptoms, so it includes presentations in which there is one fewer symptom present than the four required for a diagnosis of euphoric mania or the five required for a diagnosis of irritable mania. The mania or hypomania in BP-NOS must occur for at least four hours/day for at least four days.
Overall, the COBY researchers found that among children with a BP-NOS diagnosis, it was the duration of the manic symptoms that tended to fall short of the requirements for a BP-I or BP-II diagnosis rather than any qualitative difference in clinical presentation. The COBY study followed 446 BP-NOS patients aged 7 to 17 for an average of five years using the LIFE methodology, which rates severity of ill states on a weekly basis. The assessments of LIFE data were conducted at an average of eight-month intervals.
Axelson’s key point was that within the 5-year period of the study, 45% of the children with BP-NOS, which some would consider a subthreshold bipolar disorder, converted to a full-blown bipolar disorder; 23% to a BP-I presentation and 22% to a BP-II presentation. If there was a positive family history of mania, it was even more likely that a child with BP-NOS would convert to BP-I or BP-II (58.5%, as opposed to 35.5% when there was no positive family history for mania).
Children with BP-NOS are almost as highly impaired as those with BP-I and BP-II illness, and clearly deserve early treatment intervention, both to alleviate problematic symptomatology, but also to possibly prevent the conversion to more full-blown BP-I and II syndromes. Axelson stressed the importance of treating those with BP-NOS who do not convert to BP I or II, because they too remain substantially impaired.
Bipolar Disorder in Children Continues into Adulthood, Early Intervention Important
At a symposium on new research on juvenile bipolar disorder at the meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) in 2010, researchers shared new findings about juvenile bipolar disorder. One was Kathleen Merikangas’ finding published in AACAP’s journal in 2010 that the incidence of Bipolar I and II disorders is substantial in the child population (2.6%), and most children with the illness are severely impaired. This estimate of the incidence of bipolar disorder in children approaches the 3.0% incidence of the disorder in adults.
Another finding came from Janet Wozniak of Massachusetts General Hospital. Wozniak followed children with a bipolar diagnosis longitudinally and found substantial evidence of impairment and continuity of the diagnosis over 2-3 years. She found that 73.1% of the original 78 children (aged 10.5 years at first evaluation) were still fully symptomatic with a BP-I diagnosis after 3.6 years of follow up. Only five children of the 78 achieved a euthymic status without treatment. Nine children became euthymic while on treatment, while 5 experienced subthreshold major depressive disorder and another six had subthreshold manic symptomatology.
Dr. Wozniak indicated that these data were similar to Barbara Geller’s eight-year followup study, in which patients remained symptomatic for two-thirds of the weeks of followup and 44.4% continued to show full-blown manic episodes. Researchers Barbara Geller, David Axelson, and Joe Biedermann all have found that while there is a high incidence of initial improvement or transient remission in childhood bipolar disorder, there is an equally substantial relapse rate, indicating that the considerable morbidity of childhood-onset bipolar illness continues into adolescence and young adulthood. Read more
N-acetylcysteine Improved the Irritability Associated with Autism
 At the 57th Annual Meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) in October 2010, Lawrence Fung of Stanford University reported that N-acetylcysteine (NAC), a compound sold over-the-counter in health food stores, improved irritability and other symptoms of autism in children aged 8 to 17. In this double-blind, randomized study of NAC compared with placebo, the children who received NAC were treated with 900mg once a day for four weeks, then 900mg BID (twice a day) for four weeks, and finally 900mg TID (three times a day) for the last four weeks of this three-month study. These doses significantly improved irritability and stereotypy (repetitive behaviors) compared with placebo. Side effects were minimal.
At the 57th Annual Meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) in October 2010, Lawrence Fung of Stanford University reported that N-acetylcysteine (NAC), a compound sold over-the-counter in health food stores, improved irritability and other symptoms of autism in children aged 8 to 17. In this double-blind, randomized study of NAC compared with placebo, the children who received NAC were treated with 900mg once a day for four weeks, then 900mg BID (twice a day) for four weeks, and finally 900mg TID (three times a day) for the last four weeks of this three-month study. These doses significantly improved irritability and stereotypy (repetitive behaviors) compared with placebo. Side effects were minimal.
Editor’s note: The potential for a safe compound such as N-acetylcysteine to show efficacy in autism is striking. Currently only risperidone and aripiprazole are FDA-approved for effectiveness treating irritability in autism. There has also been a positive study of valproate compared with placebo in autism, although it is not FDA-approved for this purpose.
Most double-blind, placebo controlled clinical trials of NAC have been in adults, so this is the first report that suggests NAC can safely be used in children.
NAC’s ability to improve irritability in autism raises the possibility that this drug may be useful in the treatment of irritability and repetitive behaviors in bipolar disorder, particularly since N-acetylcysteine has also been reported to improve mood, especially depression, in adults with bipolar disorder in the studies of Mike Berk and colleagues published in Biological Psychiatry in 2008.
This study adds to the evidence that suggests N-acetylcysteine may reset the brain’s habit system in the ventral striatum (also called the nucleus accumbens), which is involved in the assessment of the reward value of a variety of substances of abuse and behaviors (as described in BNN Volume 14, Issue 1 from 2010). NAC improves a number of habit-related syndromes including cocaine, heroin, and gambling addictions, trichotillomania (compulsive hair-pulling), and now the irritability and stereotypic behaviors of autism.
In light of NAC’s profile of efficacy and safety, systematic exploration of the drug in childhood-onset bipolar illness is indicated. We are aware of at least one group that is planning such a study.



