ECT Update: Some good news and some not-so-good news
 A 2013 study by Prudic et al. in the Journal of Electro-convulsive Therapy reveals some good and some not-so-good news about ECT. The good news about ECT is that it produced moderate acute remission rates. In this randomized study of ECT treatment, improvement rates were better when patients received right unilateral (RUL) ultra-brief pulse at high doses (6 times a patient’s seizure threshold) than with bilateral (BL) pulse at low doses (1.5 times the patient’s seizure threshold). RUL also has fewer cognitive side effects than BL.
A 2013 study by Prudic et al. in the Journal of Electro-convulsive Therapy reveals some good and some not-so-good news about ECT. The good news about ECT is that it produced moderate acute remission rates. In this randomized study of ECT treatment, improvement rates were better when patients received right unilateral (RUL) ultra-brief pulse at high doses (6 times a patient’s seizure threshold) than with bilateral (BL) pulse at low doses (1.5 times the patient’s seizure threshold). RUL also has fewer cognitive side effects than BL.
Prudic also found that these acute remission rates were best when antidepressant treatment was begun at the same time as ECT rather than after the end of ECT treatment.
Unfortunately, a previous study by Prudic et al. showed that relapse rates after ECT remain high. Two-thirds of patients relapse in the first six months after ECT. Half of patients who receive antidepressant treatment following ECT relapse within the first six months after their last ECT treatment. Twenty to forty percent relapse in the first month after their last ECT treatment.
In the current study, timing and likelihood of relapse was independent of whether antidepressant treatment was started at the outset of ECT or after the end of ECT. Relapse also did not depend on which pharmacological treatments are used (nortriptyine plus lithium versus venlafaxine plus lithium).
Older patients (average age 55) did better—they relapsed less often than patients with an average age of 45. Patients with unipolar and bipolar depression did not differ in relapse rates.
Previous history of illness did affect relapse. The number of prior antidepressant trials a patient had tried for a current depressive episode (a measure of treatment resistance) was related to how fast they relapsed on follow-up pharmacotherapy after receiving ECT (more antidepressant trials was associated with faster relapse).
Other studies have shown that continuation of ECT treatment is not superior to continued treatment with drugs following ECT treatment.
Editor’s Note: ECT works acutely, but too often its effects do not last long, even with intensive continuation treatment with an antidepressant and lithium. Therefore for patients with highly recurrent illness, its usefulness is largely limited to acute emergencies, such as high risk of suicide or medical deterioration.
There are currently no good controlled studies showing how to prevent depressive relapse after remission with ECT using either drug continuation therapy or maintenance ECT. Greater degrees of treatment resistance are associated with lower rates of both acute remission and faster relapse during follow-up pharmacotherapy.
If a patient is going to have ECT, RUL would be recommended over bilateral, because bilateral ECT is associated with decreases in autobiographical memory even after six months, and these deficits are in proportion to the number of bilateral ECT treatments received.
Alternatives to ECT
Other types of brain stimulation treatments could potentially serve as alternatives to ECT. Read more
Meditation Improves Mood and White Matter Integrity
New research shows that regular meditation in the form of mindfulness training improves both mood and measures of white matter (axon tract) integrity and plasticity in the anterior cingulate cortex (a key node in the brain network modulating self-regulation).
This research by Tang et al. published in the Proceedings of the National Academy of Sciences in 2012 was a continuation of the same research group’s investigation of integrative mind-body training (IMBT), a type of mindfulness training that incorporates increased awareness of body, breathing, and attention to external instructions meant to induce a state of balanced relaxation and focused attention. In a previous Tang et al. study comparing participants who received IMBT training with a control group who spent the same amount of time doing relaxation training, the participants who practiced IMBT for five days (20 minutes/day) had better scores on measures of attention, anxiety, depression, anger, fatigue, and energy. In another study the researchers found that four weeks of IMBT (30 minutes/day) increased fractional anisotrophy (FA) in white matter areas involving the anterior cingulate cortex, while four weeks of relaxation training did not bring about any effect on white matter. Decrease in FA is a part of aging. The four weeks of IMBT also decreased axial and radial diffusivity, suggesting better alignment of axons along white matter tracts.
In the most recent study, two weeks of IMBT (30 minutes/day) produced a reduction in axial diffusivity, but not effects on fractional anisotrophy or radial diffusivity, suggesting that the reduced axial diffusivity leads to the other changes seen with longer IMBT.
Editor’s Note: In those with unresolved problems with anxiety and depression, regular 20-30 minutes/day mindfulness practice may have beneficial effects not only on mood, but also on central nervous system structures. Mindfulness training involves focused attention on sequentially different parts of the body leading to exclusive focus on the physical aspects of breathing in and out. Intruding thoughts are recognized, but let go as trivial, passing interruptions, and focus is returned to the body and breathing. The aim is to clear the mind of its usual ideas, thoughts, and worries by continually refocusing on breathing. It takes practice to achieve, but regular mindfulness training can be a helpful addition to pharmaco- and psychotherapy.
It is also noteworthy that mindfulness training is one of the processes that helps elongate the ends of each strand of DNA, called telomeres. Telomeres shorten with aging, stress, and episodes of depression, and short telomeres lead to a variety of adverse medical consequences.
Lamotrigine Not Helpful as Add-on to Lithium and Valproate in Rapid Cycling Bipolar Disorder
 A 2012 study by Kemp et al. in the journal Bipolar Disorders found that lamotrigine added to combination treatment with lithium and valproate was no more effective than placebo in patients with rapid cycling bipolar disorder. Only 14% (19 out of 133) of rapid cycling patients stabilized upon initial treatment with the open combination of lithium and valproate, a startlingly low rate. In the next phase of the study, 49 patients who were not stabilized were given adjunctive treatment with either lamotrigine (n=23) or placebo (n=26) on a double-blind basis, but no significant difference was observed.
A 2012 study by Kemp et al. in the journal Bipolar Disorders found that lamotrigine added to combination treatment with lithium and valproate was no more effective than placebo in patients with rapid cycling bipolar disorder. Only 14% (19 out of 133) of rapid cycling patients stabilized upon initial treatment with the open combination of lithium and valproate, a startlingly low rate. In the next phase of the study, 49 patients who were not stabilized were given adjunctive treatment with either lamotrigine (n=23) or placebo (n=26) on a double-blind basis, but no significant difference was observed.
Editor’s Note: This study has two pieces of not-so-good news. The first is that it was so difficult to stabilize these patients with rapid cycling bipolar disorder. The second is that the add-on of lamotrigine, which is highly effective in the prevention of depressions in bipolar disorder, was in this case no more effective than placebo.
This study again demonstrates that rapid cycling bipolar disorder is difficult to treat, and even the use of three proven mood stabilizers in combination is not always effective. Many doctors would recommend an atypical antipsychotic as the next clinical option.
Lithium-Induced Hypercalcemia
In a poster at the 5th Biennial Conference of the International Society for Bipolar Disorders, researchers from the Netherlands including E.J. Regeer described the prevalence of hypercalcemia (high calcium levels) in patients with bipolar disorder who are treated with lithium. In a study of 314 patients taking lithium, Regeer and colleagues found that calcium levels were elevated in 15.6% of the patients, and the length of time patients had been treated with lithium was significantly related to the degree of hypercalcemia. It is recommended that blood levels of calcium be monitored in patients on lithium.
The researchers recommended testing for parathyroid hormone in blood in order to exclude other causes of hypercalcemia. They also suggested that when lithium cannot safely be discontinued or when its discontinuation does not resolve the hypercalcemia, other treatment for high blood calcium, including removal of the parathyroid, may be necessary.
Lithium Discontinuation Results in Only Modest Improvement in Renal Function Compared to Continued Treatment
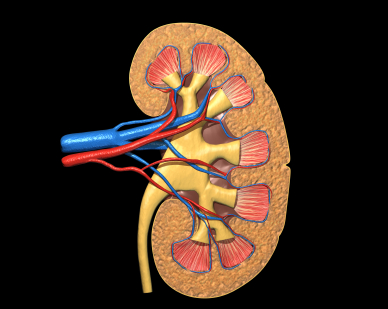 Lithium is one of the most important treatments available for bipolar disorder. Unfortunately long-term use can be complicated by renal (kidney) dysfunction and, in rare cases, renal failure. A 2012 study by Rej et al. of geriatric patients with a history of lithium use and symptoms of chronic renal failure found that after two years, differences in outcomes for patients who continued lithium use versus stopping this treatment were not significantly different, though the lithium continuers had slightly less renal function after 60 months.
Lithium is one of the most important treatments available for bipolar disorder. Unfortunately long-term use can be complicated by renal (kidney) dysfunction and, in rare cases, renal failure. A 2012 study by Rej et al. of geriatric patients with a history of lithium use and symptoms of chronic renal failure found that after two years, differences in outcomes for patients who continued lithium use versus stopping this treatment were not significantly different, though the lithium continuers had slightly less renal function after 60 months.
Editor’s Note: This study addresses one of the important unanswered questions about what to do when kidney function starts to diminish (observed as high levels of creatinine (Cr) or low Cr clearance) in patients on chronic lithium treatment.
The findings of Rej et al. suggest that the advantages of discontinuing lithium are not huge. Renal function may deteriorate a bit less (or not at all) in those who stop lithium. However, if someone is highly responsive to lithium and the “creatinine creep” upwards is slow, that patient might be able to proceed with careful monitoring and lithium continuation. Where other treatment options are readily available, the discontinuation route might be a good choice.
This study brings some much-needed randomized longitudinal data (if not a definitive recommendation) to bear on a difficult clinical decision that may have to be addressed when lithium is used in long-term approaches to bipolar disorder.
Acquired Lithium Resistance
Lithium is one of the most important treatments available for bipolar disorder. A small percentage of patients who initially respond well to lithium may develop resistance to the drug over time. Some develop tolerance to the drug’s therapeutic effects over a period of years, seen as a gradual breaking through of manic or depressive episodes that increase in severity or frequency. Others who are good long-term responders to lithium, but stop taking lithium and then suffer relapses, fail to respond as well as they had before. In a few instances, the drug no longer helps at all. This latter form of acquired lithium resistance is called lithium discontinuation-induced refractoriness.
In a review article published in the Journal of Affective Disorders in 2011, this editor (Robert Post) analyzed case series and case reports that depicted these two different types of acquired lithium resistance and reported that each must be addressed in a different way. In the case of tolerance development, a temporary break from lithium may theoretically restore its effectiveness, but the typical way to treat this situation is to add additional drugs with different mechanisms of action that are not affected by the tolerance.
In those who stop effective lithium treatment and experience relapses that are no longer responsive when lithium is re-instituted, it is not clear what the best treatment approaches are. Therefore the most conservative approach to preventive treatment with lithium is to avoid discontinuing the drug. This would appear to be a generally sound principle for the treatment of recurrent unipolar or bipolar illness. When things are going well, do not change the regimen; leave well-enough alone. Conversely, when treatment is not optimal, as in the case of loss of drug responsiveness via tolerance, a more aggressive exploration of treatment options would be warranted.
Patients should be aware of the multiple dangers of stopping effective treatment with lithium. These include: likely relapse, perhaps the necessity of hospitalization, an increased risk of suicide, and the loss of responsiveness to lithium that appears to occur in approximately 15% of patients who stop lithium when it is working effectively.
Lithium Extends Telomeres
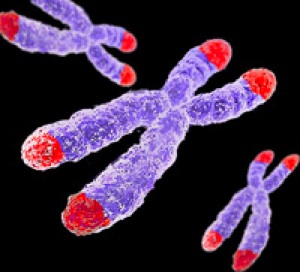 Telomeres sit at the ends of strands of DNA at each chromosome. Various events make telomeres decrease in length: cell division/replication, stress, aging, and depressive episodes in Bipolar II disorder.
Telomeres sit at the ends of strands of DNA at each chromosome. Various events make telomeres decrease in length: cell division/replication, stress, aging, and depressive episodes in Bipolar II disorder.
Martin Schalling, a professor of medical genetics at the Karolinska Institutet in Sweden, has found that lithium treatment lengthens telomeres.
Editor’s Note: This finding by Schalling, which will soon be published, adds to the list of beneficial neurobiological effects of lithium, including increasing cell survival factors BDNF and Bcl-2, decreasing cell death factors BAX and p53, increasing marker of neuronal integrity NAA, and possibly increasing hippocampal and cortical grey matter volumes.
Clinically, lithium decreases recurrence of manic and depressive episodes (mania more than depression), decreases suicidality, and may slow cognitive deterioration in those with mild cognitive impairment.
These clinical and neurobiological benefits to lithium treatment should be factored in to calculations of the risk/benefit ratio for lithium use in long-term preventative treatment of bipolar disorder.
Lithium Increases the Volume of the Prefrontal Cortex in Responders
 Studies have indicated that lithium increases gray matter and the volume of the cortex and hippocampus in patients with bipolar I disorder. A poster presented by S. Selek et al. at the 5th Biennial Conference of the International Society for Bipolar Disorders described a longitudinal study of fronto-limbic brain structures in patients with bipolar I disorder during lithium treatment.
Studies have indicated that lithium increases gray matter and the volume of the cortex and hippocampus in patients with bipolar I disorder. A poster presented by S. Selek et al. at the 5th Biennial Conference of the International Society for Bipolar Disorders described a longitudinal study of fronto-limbic brain structures in patients with bipolar I disorder during lithium treatment.
This study reported that patients whose illness failed to respond to lithium had smaller right amygdalas than euthymic bipolar I patients or healthy controls. After treatment with lithium, those who responded well to the drug showed significant enlargement of the left prefrontal cortex and the left dorsolateral prefrontal cortex, while those who responded poorly to lithium showed decreases in the volume of their left hippocampus and right anterior cingulate cortex.
Editor’s Note: This is one of several studies that suggest a relationship between volume of brain regions and degree of response to lithium. These data add to the remarkably consistent literature suggesting that lithium may have neurotrophic and neuro-protective effects, potentially because of the drug’s ability to increase neuroprotective factors such as BDNF and Bcl-2 while decreasing cell death factors such as BAX and p53.
Minute Levels of Lithium in Public Water Supply Decrease Suicide
 Blüml et al. reported in the Journal of Psychiatric Research in 2013 that among 226 counties in Texas, the ones with higher trace levels of lithium in the public water supply had lower rates of completed suicide in the general population than did the counties with lower lithium levels. The naturally occurring lithium levels in public water supplies in the geographic regions described in this study ranged from 2.8 to 219 ?g/l or 0.00043 to 0.0315 mmol/l (much lower than the levels used to treat bipolar disorder).
Blüml et al. reported in the Journal of Psychiatric Research in 2013 that among 226 counties in Texas, the ones with higher trace levels of lithium in the public water supply had lower rates of completed suicide in the general population than did the counties with lower lithium levels. The naturally occurring lithium levels in public water supplies in the geographic regions described in this study ranged from 2.8 to 219 ?g/l or 0.00043 to 0.0315 mmol/l (much lower than the levels used to treat bipolar disorder).
This is the fourth positive study describing this effect, including two in Texas, one in Japan, and one in Austria. (One study from part of England failed to show this relationship, though levels measured in that study had a much lower and restricted range, from less than 1 to 21 ?g/l.) The most recent studies have collected more water samples and used more sophisticated statistical analyses to control for socioeconomic and a variety of other demographic effects on suicide.
Editor’s Note: Why higher trace levels of lithium occurring naturally in the water supply should have this anti-suicide effect in the general population is unknown, but it is a fascinating finding. It also gives indirect credence to the clinical findings in patients with unipolar and bipolar disorder that lithium (albeit in the much higher levels achieved with medication) has anti-suicide effects.
Lithium Reduces Suicide Rate and Increases Longevity
 Suicide is an unfortunate consequence of bipolar disorder in 10-15% of patients. A study by Manchia et al. examined suicidal behavior in 737 families of bipolar patients, including 4,919 first-degree relatives. Suicidal behavior ran in families and was more prevalent in those with an early age of onset and a shorter duration of illness. The good news: lithium treatment decreased suicide risk independent of its degree of effectiveness in treating bipolar disorder. Those on lithium also had a longer median age of survival (73 versus 65 years).
Suicide is an unfortunate consequence of bipolar disorder in 10-15% of patients. A study by Manchia et al. examined suicidal behavior in 737 families of bipolar patients, including 4,919 first-degree relatives. Suicidal behavior ran in families and was more prevalent in those with an early age of onset and a shorter duration of illness. The good news: lithium treatment decreased suicide risk independent of its degree of effectiveness in treating bipolar disorder. Those on lithium also had a longer median age of survival (73 versus 65 years).
Editor’s Note: These data are consistent with a variety of other studies and raise the question why lithium is used less frequently in the US than in many European countries and Canada. Given its neuroprotective effects, its prevention of suicide and dementia, and its positive effects on longevity, it is hard to see why lithium is not included in the treatment regimens of more patients (at whatever dosage is well-tolerated), even if it alone is not sufficient for treating their manic and depressive episodes.
Research (by this editor Robert Post and colleagues) shows that bipolar disorder is a more pernicious illness in almost all respects in the US compared to the Netherlands and Germany (International Journal of Neuropsychopharmacology, 2011). Whether bipolar illness would be less severe in the US if it were more often treated with lithium is an unanswered question. The field cannot provide an answer with systematic prospective controlled data, as most study designs would be unethical (i.e. would deny useful treatment to suffering patients), although one large randomized comparative study called BALANCE did show the superiority of lithium over valproate. However, individual patients in consultation with their physician could evaluate the evidence and request that lithium be considered in their treatment regimen.
If a patient has some clinical predictors of a likely good response to lithium, the decision to include lithium should be a slam-dunk. Some of these include: a positive family history of mood disorder, especially bipolar disorder; a classic course with distinct episodes and clear periods of wellness; manic episodes that are euphoric as opposed to dysphoric (i.e. anxious/irritable); lack of an anxiety disorder or substance abuse comorbidity; the absence of mood-incongruent delusions; and a sequence of episodes of mania followed by a depression and then a well interval (MDI) rather than the sequence of DMI.




