Ambiguity in the Data on Omega-3 Fatty Acids for Depression
 In a recent randomized, controlled clinical study comparing two types of omega-3 fatty acid supplements (one with EPA and one with DHA) with placebo in 196 adults with major depression, there were no statistically significant differences in outcomes across the three groups. The participants received the treatments for eight weeks, and response and remission rates were 40-50% in those receiving either omega-3 preparation (at doses of 1000mg/day) and 30% for placebo. The research was published by David Mischoulon and colleagues in the Journal of Clinical Psychiatry.
In a recent randomized, controlled clinical study comparing two types of omega-3 fatty acid supplements (one with EPA and one with DHA) with placebo in 196 adults with major depression, there were no statistically significant differences in outcomes across the three groups. The participants received the treatments for eight weeks, and response and remission rates were 40-50% in those receiving either omega-3 preparation (at doses of 1000mg/day) and 30% for placebo. The research was published by David Mischoulon and colleagues in the Journal of Clinical Psychiatry.
If You Are Depressed After a Heart Attack, Treat the Depression
 Depression is common following heart attacks, and it can complicate recovery. A recent study by Jae-Min Kim and colleagues investigated the safety of treating depression with escitalopram in people recovering from acute coronary syndrome. In a 2015 article in the Journal of Clinical Psychiatry, they reported that 217 people with depression and acute coronary syndrome were randomized to receive either escitalopram (in flexible doses ranging from 5–20 mg/day) or placebo for 24 weeks. Patients who received escitalopram saw more improvement in their depression on a variety of scales, and also showed improvements in social and occupational functioning. There were no adverse cardiac effects from escitalopram, though some people taking it did experience dizziness.
Depression is common following heart attacks, and it can complicate recovery. A recent study by Jae-Min Kim and colleagues investigated the safety of treating depression with escitalopram in people recovering from acute coronary syndrome. In a 2015 article in the Journal of Clinical Psychiatry, they reported that 217 people with depression and acute coronary syndrome were randomized to receive either escitalopram (in flexible doses ranging from 5–20 mg/day) or placebo for 24 weeks. Patients who received escitalopram saw more improvement in their depression on a variety of scales, and also showed improvements in social and occupational functioning. There were no adverse cardiac effects from escitalopram, though some people taking it did experience dizziness.
Child Network Launches
A STUDY ASSESSING YOUR CHILD’S MOOD AND BEHAVIOR
Parents, if your child (aged 2 – 12) has mood or behavioral difficulties, we would like to enlist your participation in a study called the Child Network. Parents who enroll in the study will complete an online rating checklist of your child’s symptoms once a week by a secure web-based system.
In addition, adults who have been diagnosed with depression or bipolar disorder and are the biological parent of a child (ages 2-12) who is currently healthy and has no troublesome mood or behavioral symptoms may also be eligible to participate in this study.
If you are interested in participating in this study, please click here. For more information, click here, call 301-530-8245, or email questions to PROTECTED EMAIL ADDRESS.
ADHD and Bipolar Disorder Are Inherited Separately
While attention-deficit hyperactivity disorder (ADHD) is fairly common among people with bipolar disorder, the genetic risks of inheriting these two illnesses run separately in families. In a recent study of 465 people and 563 of their first-degree relatives by Susan Shur-Fen Gau and colleagues, people with bipolar I disorder were likely to have relatives with bipolar I disorder, and people with ADHD were likely to have relatives with ADHD, but ADHD did not increase risk of bipolar disorder and vice versa.
The researchers hypothesize that other reasons people might develop both disorders include developmental precursors to the illnesses, neurocognitive functioning, sleep problems, and personality traits such as impulsivity and disinhibition.
Editor’s Note: At a recent scientific meeting, Gau and her colleague Kathleen Merikangas said that people with bipolar disorder in the study were five times more likely to have relatives with bipolar disorder. Bipolar disorder and ADHD were comorbid in 37.8% of those with bipolar I disorder, 16.4% in bipolar II disorder, 14% in depression, and 1.1% in normal controls.
Employment Rights for People with Bipolar Disorder
“Society’s accumulated myths and fears about disability and disease are as handicapping as the…limitations that flow from actual impairment.”
—US Supreme Court
Attorney Katharine Gordon has provided some information on legal rights under the ADA.
When we think of the Americans with Disabilities Act (ADA), we might think of physical modifications to buildings, expensive lawyers, and complicated trials. But this law also gives people with bipolar ways to get fair treatment in the workplace. By learning a bit about your employment rights under this law, you can focus on excelling in your chosen career, rather than being sidetracked by ignorance, stereotypes, and stigma.
Here are a few things that you may not know about bipolar disorder and the ADA:
It is now clear that people with bipolar disorder are protected under the ADA in employment. Prior to 2008, there was often a battle of the experts to prove that a person with bipolar disorder had a severe enough impairment to be protected. This discouraged many from asking for their rights to be respected under this law in the first place. Unfortunately, companies would fire people for having bipolar disorder and then, in next breath, argue that bipolar wasn’t a real disability therefore it was legal to fire people for reasons related to their bipolar disorder.
This changed with the passage of the Americans with Disabilities Act Amendments Act of 2008, which made it easier to establish disability. The Equal Employment Opportunity Commission, the agency responsible for enforcing this law, has made it clear in official regulations that bipolar should generally be covered as a disability for the purposes of protection in employment: “It should easily be concluded that the following types of impairments will, at a minimum, substantially limit the major life activities indicated:…major depressive disorder, bipolar disorder, post-traumatic stress disorder, obsessive compulsive disorder, and schizophrenia substantially limit brain function.” 29 C.F.R. § 1630.2(j)(3)(ii), (iii).
Job applicants should never be asked whether they have bipolar disorder (or any other disability) until a conditional offer has been made. Read more
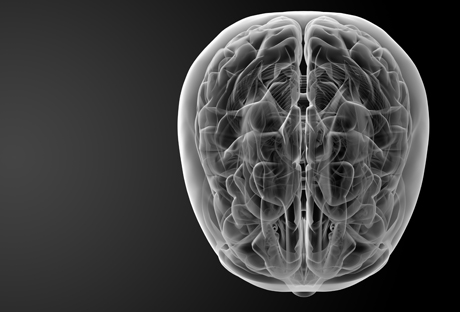
Abnormal Levels of Cytokines Found in Brains of Suicide Victims
Cytokines are chemical messengers that send signals between immune cells and between the immune system and the central nervous system. Their levels in blood are considered a measure of inflammation, which has been implicated in depression and stress. A new study by Ghanshyam Pandey and colleagues reported increased levels of cytokines in the brains of people who committed suicide. In the prefrontal cortices of people who died by suicide, there were significantly elevated levels of the inflammatory cytokines IL-1 beta, IL-6 and TNF-alpha compared to the brains of normal controls. There were also lower levels of protein expression of the cytokine receptors IL-1R1, IL-1R2 and IL-1R antagonist (IL1RA) in the suicide brains compared to controls.
The researchers concluded that abnormalities in proinflammatory cytokines and their receptors are associated with the pathophysiology of depression and suicide. This research provides direct confirmation of the indirect measures of inflammation observed in the blood of depressed patients compared to controls.
More Data on Memantine for Treatment-Resistant Depression
In 2012 we reported on an open study by Athanasios Koukopoulos and colleagues that explored whether the NMDA glutamate receptor antagonist memantine (Namenda), which is used to treat dementia, could be helpful to people with treatment-resistant bipolar disorder. In an update of that study, the researchers, led by Giulia Serra, compared patients’ symptoms during three years of treatment as usual, followed by three years with memantine added to their stable medication regime (at doses of 20–30 mg/day). Patients improved progressively over the three years of taking memantine.
Improvements in symptoms included decreased time ill, decreased severity of symptoms, decreased duration of new episodes, and fewer episodes per year. Memantine was particularly helpful for those patients who had had rapid or continuous cycling. Side effects were minimal.
Given the success of this open study, randomized controlled trials are needed to explore this much-needed option for people with treatment-resistant bipolar disorder.
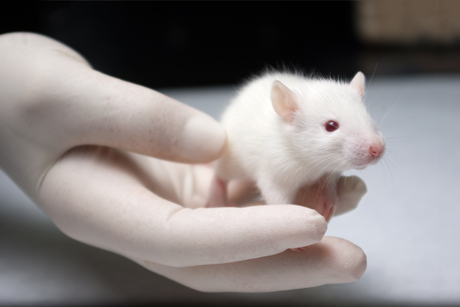
Anti-Inflammatory Treatment Prevents the Effects of Stress in Female Rats
Women are more likely than men to experience depression, and this difference begins in adolescence, when girls show more sensitivity to stress. Researchers are studying how animals react to stress in the hopes of learning what mediates these gender differences in mental illness.
At a recent scientific meeting, researcher Jodi Lukkes and colleagues presented a recent study of stress and inflammation in female rats. The rats were exposed to different types of stressors. Some were separated from their mothers for four hours a day during the first 20 days of their lives. Later, some rats were exposed to an acute stressor, witnessing another rat receiving shocks. All the rats were placed in a box in which they could escape a shock by jumping to the other end of the box, in order to measure their motivation. Because drugs that inhibit the inflammatory enzyme COX-2 had reversed the effects of maternal separation in earlier studies, the researchers also treated some rats with these anti-inflammatories.
The researchers found that anti-inflammatory treatment could prevent behavioral consequences of stress in adolescent female rats. Witnessing another rat being shocked brought about deficits in motivation (a depression-like behavior), but in rats that had received treatment with a COX-2 inhibitor, these deficits were reduced. The COX-2 treatment was only helpful to rats that had experienced an acute stressor in their lifetime, either maternal separation in infancy, or witnessing another rat receive the shocks. A history of stress was required for the anti-inflammatories to improve motivation.
Lukkes and colleagues hope that this research begins to clarify the relationship between stress, inflammation, and gender. This may eventually lead to new targets in the treatment of depression.