Transcranial Direct Current Stimulation (tDCS) Induces Gray-Matter Increases in Depression
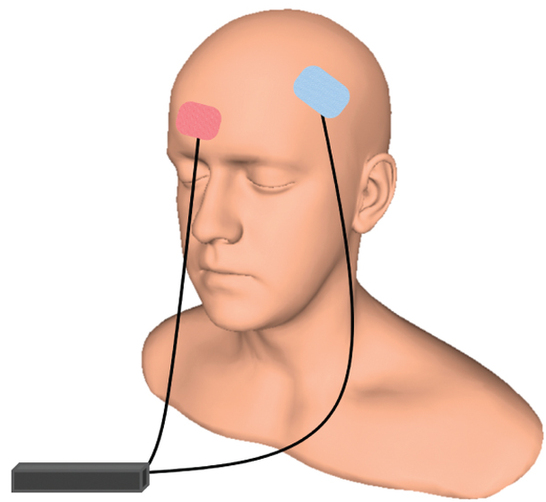
At the 2021 meeting of the Society of Biological Psychiatry (SOBP), researcher Mayank Jog and colleagues described a study of transcranial direct current stimulation (tDCS) in 59 patients with moderate depression. The patients received either tDCS sessions that delivered electrical current at 2mA for 20 minutes or a same-length sham stimulation delivered using a double-blind stimulator, for a total of 12 sessions over 12 consecutive working days. Jog and colleagues found that compared to the sham stimulation, tDCS induced increases in gray matter volume in the left dorsolateral prefrontal cortex (DLPFC) target area, with a statistically large effect size (Cohen’s d = 1.3). The researchers plan to follow up this study that found structural changes to the brain after tDCS with more research on the antidepressant effects of the treatment.
Accelerated Intermittent Theta-Burst Stimulation (aiTBS) Quickly Improved Treatment-Resistant Depression

At the 2021 meeting of the Society of Biological Psychiatry (SOBP), researcher Nolan Williams and colleagues described a sham-controlled trial of accelerated intermittent theta-burst stimulation (aiTBS) in patients with treatment-resistant depression. Theta burst stimulation is a specific protocol for rTMS, or repeated transcranial magnetic stimulation, a non-invasive form of brain stimulation. Magnets placed on a patient’s head provide bursts of high-frequency stimulation to the brain.
Participants in the study received 50 sessions over 5 days of either aiTBS or a sham procedure. Among those who received the real aiTBS treatment, 85.7% saw an improvement in their treatment-resistant depression, compared to only 26.7% of those in the sham group. AiTBS produced a rapid antidepressant response, which Williams and colleagues suggest could be useful for the treatment of patients in emergency rooms or inpatient settings.
Transcranial Near-Infrared Light May Treat Brain Injury and Neurodegeneration
At the 2021 meeting of the Society of Biological Psychiatry, there was a symposium on treatment with near-infrared light chaired by researchers Paolo Cassano and Dan Iosifescu. The treatment is known as transcranial photobiomodulation (PBM) with near-infrared light. A device worn on the head delivers infrared light that penetrates the cerebral cortex and can modulate cortical excitability. It has a variety of effects including promoting neuroplasticity, improving oxygenation, and decreasing inflammation and oxidative stress.
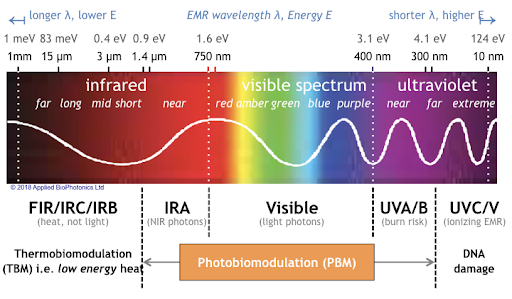
A number of studies exploring the possibility that PBM could be used as a clinical treatment for conditions such as depression, brain injury, or dementia were presented at the symposium.
Researcher Lorelei Tucker discussed promising findings from an animal model in which rats with stroke or brain injuries showed improvement after being treated with PBM.
Cassano discussed studies aimed at refining which brain areas should be targeted with PBM and how much light should be delivered in order to improve depression. In double-blind, sham-controlled studies in people with major depression, targeting the dorsolateral prefrontal cortex with PBM improved their symptoms.
Researcher Benjamin Vakoc discussed a study of low-level light therapy (LLLT) using near-infrared light compared to a sham procedure in 68 people with moderate traumatic brain injury. The researchers used magnetic resonance imaging (MRI) to assess changes in white matter in the brain over time in people recovering from an acute brain injury. Patterns of changes in white matter were different for those who received LLLT compared to those who received the sham procedure.
Researcher Linda Chao described a very small study to determine whether PBM could improve symptoms of dementia. Four patients received typical dementia care while four others underwent home treatments with the commercially available Vielight Neuro Gamma device, which delivers PBM via both the scalp and an insert in the nose. After 12 weeks, the PBM group showed improvements in cognition and brain connectivity.

Editor’s Note: We will be watching the literature to follow advances in this promising novel method of neuromodulation.

