High-Dose Vitamin D May Improve Cognition More Than Low-Dose Vitamin D
 Vitamin D deficiency has been associated with dementia and cognitive decline, but supplements may help. In a study of 82 healthy individuals with low vitamin D levels, high-dose vitamin D supplements (4000 IU/day) improved visual/nonverbal memory more than did low-dose vitamin D supplements (400 IU/day) over 18 weeks.
Vitamin D deficiency has been associated with dementia and cognitive decline, but supplements may help. In a study of 82 healthy individuals with low vitamin D levels, high-dose vitamin D supplements (4000 IU/day) improved visual/nonverbal memory more than did low-dose vitamin D supplements (400 IU/day) over 18 weeks.
The 2017 study took place in Canada, where short winter days can make it more difficult to get sufficient levels of vitamin D from sunlight. The higher-dose supplements raised blood levels of vitamin D compared with the lower-dose supplements.
Those who received the higher doses performed better at tests of visual memory such as the Pattern Recognition Memory Task and the Paired Associates Learning Task, but their performance on tests of verbal memory was not significantly different from those in the lower-dose group. This suggests that higher vitamin D levels are particularly important to visual/nonverbal memory.
The study by Jacqueline A. Pettersen was published in the journal Experimental Gerontology.
Antipsychotic Drug Pimavanserin Seems to Reduce Psychosis in People with Alzheimer’s
 The antipsychotic drug pimavanserin was approved by the US Food and Drug Administration last year as a treatment for hallucinations and delusions in Parkinson’s disease. Now it looks as though it may also help people with Alzheimer’s disease. Pimavanserin works differently than other antipsychotic medications—a selective serotonin inverse agonist, it acts at serotonin HT2A receptors to produce effects opposite to those that serotonin would produce at the same receptor.
The antipsychotic drug pimavanserin was approved by the US Food and Drug Administration last year as a treatment for hallucinations and delusions in Parkinson’s disease. Now it looks as though it may also help people with Alzheimer’s disease. Pimavanserin works differently than other antipsychotic medications—a selective serotonin inverse agonist, it acts at serotonin HT2A receptors to produce effects opposite to those that serotonin would produce at the same receptor.
In a trial of 181 patients with Alzheimer’s and psychotic symptoms, those who received 34 mg/day of pimavanserin had a significant improvement in psychotic symptoms in six weeks compared to those who received placebo.
Over 12 weeks of treatment, pimavanserin did not impair cognition, as atypical antipsychotics can do.
Pimavanserin was well tolerated. The most common side effects were falls, urinary tract infections, and agitation. Like other atypical antipsychotics, the drug carries a box warning from the FDA that there is an increased risk of death when the drug is used to treat older people with dementia-related psychosis.
The FDA has designated pimavanserin a breakthrough therapy and is giving it priority review. These designations can speed up the development and review of a drug and are granted when a drug looks like it will be substantially better or safer than existing treatments for a serious condition.
Treatment with Hormone EPO Improved Cognition in People with Unipolar and Bipolar Disorder
People with unipolar depression and bipolar disorder may experience cognitive difficulties, even when they’re not currently depressed. In a study published in the journal European Neuropsychopharmacology in 2016, researchers led by Caroline Vintergaard Ott determined that treatment with the hormone erythropoietin (EPO) may help. EPO is produced in the kidney and increases the production of hemoglobin and red cells.
Seventy-nine participants with unipolar or bipolar disorder were randomized to receive infusions of either EPO or a saline solution once a week for eight weeks. By the end of the study, those who received EPO showed significant improvements in the speed of their complex cognitive processing compared to those who received saline. EPO is known to induce the production of red blood cells. The improvements in processing speed lasted for at least another six weeks after red blood cell production would have normalized.
Those participants who received EPO not only had improved scores on tests of processing speed, they also reported fewer cognitive complaints. The EPO treatment was most likely to be effective in participants who had more impaired cognition at the beginning of the study.
In previous research by the same research group presented by Kamilla W. Miskowiak at the 2014 meeting of the International Society of Bipolar Disorders, EPO also improved sustained attention and recognition of happy faces.
Inactivity in Young Adulthood May Worsen Cognition Later in Life
The couch potato lifestyle common in the US may have consequences later, in the form of deficits in memory, executive functioning (including planning and execution) and processing speed.
At the 2015 Alzheimer’s Association International Conference, researcher Kristine Yaffe and colleagues reported that low levels of physical activity and high rates of television viewing in young adulthood may reduce cognitive capabilities in midlife.
The Centers for Disease Control report that less than 50% of adults aged 18–64 get the recommended minimum of physical activity each week. The guidelines recommend at least 150 minutes of moderate intensity aerobic activity (such as walking briskly) and two or more days of muscle-strengthening activities that work all major muscle groups.
Yaffe says that physical activity can protect against cognitive decline or dementia later on.
Participants in the long-term study who reported burning fewer than 300 calories per 50-minute session three times per week during two-thirds of their followup visits had worse cognition at year 25 than those participants who were more active. Those who watched more than four hours of television per day also had reduced cognition in midlife.
Yaffe stresses that exercising regularly is not just important in keeping weight down and protecting the heart, but also in protecting the brain. Regular physical activity may even prevent illnesses such as Alzheimer’s disease.
Guanfacine Improves Cognition in Schizophrenia
People with disorders on the schizophrenia spectrum often suffer cognition problems that affect skills such as the processing of information about people and social situations (social cognition) and the execution of plans (executive function). At the 2015 meeting of the Society for Biological Psychiatry, researcher Larry J. Siever reported that the drug guanfacine improved these types of thinking in people with disorders on the schizophrenic spectrum compared to placebo. Participants were enrolled in a 7.5-week training program to improve cognition.
Exercise Improves Cognition and Normalizes Brain Activity
Exercise isn’t just good for the body—new research suggests it can improve cognition and normalize brain activity.
At the 2015 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Benjamin I. Goldstein reported that 20 minutes of vigorous exercise on a bike improved cognition and decreased hyperactivity in the medial prefrontal cortex in adolescents with and without bipolar disorder.
At the same meeting, researcher Danella M. Hafeman reported that offspring of parents with bipolar disorder who exercised more had lower levels of anxiety.
A plenary address by James J. Hudziak also suggested that exercise, practicing music, and mindfulness training all lead to improvements in brain function and should be an integral part of treatment for children at high risk for bipolar disorder and could be beneficial for all children.
Editor’s Note: Recognizing and responding to mood symptoms is key to the prevention and treatment of bipolar disorder in children and adolescents at high risk for the illness. For these young people, exercise, a nutritious diet, good sleep habits, and family psychoeducation about bipolar disorder symptoms may be a good place to start. Joining our Child Network may also be helpful.
Approaches to Restoring Cognition in Unipolar and Bipolar Depression
Many people with bipolar disorder suffer cognitive difficulties, and these may progress as a function of the number of mood episodes they experience. At the 2015 meeting of the International Society for Bipolar Disorders, researcher Eduard Vieta described the importance of directly prescribing diet, exercise, good sleep hygiene, smoking avoidance, and cognitive exercises designed to maintain cognitive reserves in people with bipolar disorder. Vieta stressed that one of the most important approaches to maintaining cognition is to help patients achieve and maintain remission. He also noted that those patients with lithium levels of .6meq/l or greater did not see cognitive deterioration.
Some treatments for bipolar disorder can contribute to cognition problems. Topiramate and benzodiazepines can impair cognition, as can atypical antipsychotic drugs and certain antidepressants that block the neurotransmitter acetylcholine. Avoiding these treatments and those with sedative side effects may also be helpful.
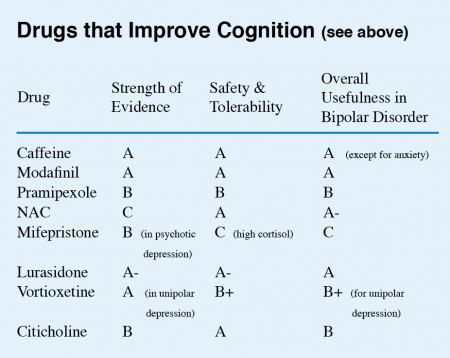
Vieta listed a series of drugs with some promise for improving cognition. (These did not include treatments for dementia, which include memantine and a group of drugs that increase acetylcholine by inhibiting its breakdown.)
This editor (Robert M. Post) has taken the liberty of giving a letter grade (A to D) to each drug on Vieta’s list on the basis of the strength of the data supporting its efficacy, its safety and tolerability, and its overall usefulness for patients with bipolar disorder. These recommendations, like other material in the BNN, are subjective and likely to change as more systematic studies on these treatments are published.
New Data on Vortioxetine for Cognition in Unipolar Depression
A 5mg dose of the antidepressant vortioxetine (Brintellix) was previously reported to have positive cognitive effects in elderly depressed patients. In a 2014 article in the International Journal of Neuropsychopharmacology, researcher Roger S. McIntyre et al. presented data from FOCUS, a study of cognition in depressed patients. The eight-week double-blind study included 18- to 65-year-olds (who were not selected for having cognitive problems per se).
McIntyre and colleagues used two tests of cognition, the Digit Symbol Substitution Test (DSST), which measures attention, psychomotor speed, and executive function, and the Rey Auditory Verbal Learning Test (RAVLT), which measures memory and acute and delayed recall. The researchers found that both the 195 patients taking 10mg/day of vortioxetine and the 207 patients taking 20mg/day of vortioxetine had better performance on both tests than the 196 patients who received placebo.
Response rates (meaning a patient achieved a 50% improvement on a scale of depression) were 47.7% on 10mg of vortioxetine, and 58.8% on 20mg of vortioxetine, compared to 29.4% on placebo. Remission rates were 29.5% on 10mg of vortioxetine and 38.2% on 20mg of vortioxetine versus 17% on placebo. McIntyre suggested that the drug worked both directly and indirectly, improving depression in some, but also improving cognition even in those whose depression did not improve.
The mechanism that could account for vortioxetine’s cognitive effects has not yet been identified. Like other selective serotonin reuptake inhibitor (SSRI) antidepressants, vortioxetine is a potent blocker of serotonin (5HT) reuptake, which it does by inhibiting the serotonin transporter (5HT-T). Unlike other SSRIs, vortioxetine is also a blocker of 5HT3 and 5HT7 receptors, an agonist at 5HT1A and 5HT1B and a partial agonist at 5HT1D receptors. It could be considered a polymodal 5HT active drug in contrast to the more selectively active 5HT-T–inhibiting SSRIs.
TDCS Promising for a Range of Illnesses
 Transcranial direct current stimulation (tDCS) shows promise for a range of problems. In new research presented at the 2014 meeting of the Society of Biological Psychiatry, it was reported to be effective for improving cognition in bipolar disorder, alleviating depression, and reducing hallucinations.
Transcranial direct current stimulation (tDCS) shows promise for a range of problems. In new research presented at the 2014 meeting of the Society of Biological Psychiatry, it was reported to be effective for improving cognition in bipolar disorder, alleviating depression, and reducing hallucinations.
How TDCS Works
At the meeting, researcher Marom Bikson discussed tDCS technology. The treatment can be delivered with a 12-volt battery. The anode directs current inward and is excitatory, while the cathode directs current outward and is inhibitory. The dendrites at the top of neurons under the anode are hyperpolarized by the tDCS, leading to relative depolarization of the cell soma, thus increasing excitation. TDCS, unlike repetitive transcranial magnetic stimulation (rTMS), which causes cells to fire, is only neuromodulatory, inducing minor changes in membrane polarization.
TDCS Improved Cognition in Bipolar Disorder
At the 2014 meeting of the American Psychiatric Association, Roberto Delle Chiaie et al. reported that two mA tDCS for 20 minutes for 15 days (anode over the left prefrontal cortex and cathode over the right cerebellum) improved immediate and delayed recall, trail making with a pointer, and motor coordination in 17 euthymic bipolar patients. This very promising result deserves further study and replication.
Antidepressant Effects of TDCS
At the 2014 meeting of the Society of Biological Psychiatry, Collen Loo reported that tDCS had positive effects in depressed patients compared to sham treatment. This complements a 2013 article by Brunoni et al. in JAMA Psychiatry that tDCS plus the selective serotonin reuptake inhibitor (SSRI) antidepressant sertraline (Zoloft) was more effective than either treatment alone.
TDCS for Treatment-Resistant Hallucinations
Jerome Brunelin et al. reported at the meeting that tDCS had positive effects in patients with schizophrenia who had hallucinations that resisted treatment. The positive electrode (anode) was placed over the left prefrontal cortex and the negative electrode (cathode) over the left temperoparietal area, where hallucinations are thought to originate. Stimulation was at two mA for 20 minutes, five days per week for two weeks. Effects lasted as long as 30 days and were associated with reduced functional connectivity of these brain regions.
Low frequency (1Hz) rTMS, which decreases neural activity, also improves refractory hallucinations when applied over the temperoparietal area, which is important for language. Placing the cathode over this area in tDCS is also inhibitory, so comparisons of rTMS with tDCS for suppressing hallucinations would be of great interest and importance.
New Antidepressant Vortioxetine May Improve Cognition and Treatment-Resistant Depression
Vortioxetine (Brintellix) is a new antidepressant that has a range of effects on serotonin receptors, making it different from selective serotonin reuptake inhibitors (SSRIs), the most common type of antidepressants, which work only on the serotonin transporter. Researcher Johan Areberg et al. reported at the 2014 meeting of the American Psychiatric Association that the drug is an antagonist at receptors 5-HT3, 5-HT7, and 5-HT1D; a partial agonist at 5-HT1B; a full agonist at 5-HT1A; and an inhibitor of the 5-HT transporter. The researchers suggested that at doses of 5mg/day, vortioxetine occupies the 5-HT3 receptors and 50% of the serotonin transporter. As dosage increases to 20mg/day, vortioxetine is believed to occupy all of the serotonin targets at clinically relevant levels. Doses of 20mg/day were found to be effective in nine studies. Researcher Gennady Smagin et al. also reported that vortioxetine activates central histamine receptors.
Vortioxetine appears to be useful in patients who have previously failed to respond to antidepressants. Researcher George I. Papakostas et al. reported that in a cohort of about 500 patients who responded inadequately to previous prescriptions of selective serotonin reuptake inhibitors (SSRIs) and serotonin and norepinephrine reuptake inhibitors (SNRIs), the 252 taking vortioxetine improved more than the 241 taking the antidepressant agomelatine.
Editor’s Note: Vortioxetine’s superior effects are impressive, as agomelatine, which is approved for use in at least 41 countries including the UK, Canada, and Australia, but is not available in the US, has previously been shown to be more effective than a number of SSRIs in head-to-head comparisons. Agomelatine improves sleep and circadian rhythms via its dual effects as an agonist at melatonin M1 and M2 receptors and an inhibitor of 5HT2C receptors, which results in the release of norepinephrine and dopamine in the frontal cortex.
Vortioxetine may be unique among antidepressants in that it appears to improve cognition. Researcher John E. Harrison et al. reported that patients saw increases in executive function, attention, speed of processing, and memory while taking vortioxetine. This is consistent with studies in aged mice, whose cognition improves more on vortioxetine than on the SSRI fluoxetine, according to researcher Yan Li and colleagues.