Update: Memantine as an Adjunct to Lamotrigine for Bipolar Depression
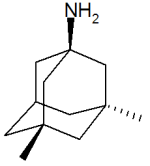
Memantine (Namenda), which is approved by the Federal Drug Administration (FDA) for use in Alzheimer’s Dementia, is increasingly being used for other conditions. Some doctors prescribe memantine for hyperactivity and attention problems in attention deficit hyperactivity disorder (ADHD), for obsessive compulsive disorder (OCD), and most recently as an adjunct to lamotrigine in bipolar depression. We wrote about the findings of Amit Anand et al. on the use of memantine and lamotrigine in January. These findings have just been published in Bipolar Disorders. The study indicates that the combination of lamotrigine with memantine brought about a rapid onset and greater magnitude of antidepressant effects than the combination of lamotrigine and placebo. The initial dose of memantine was 5mg/day, which was increased to 20mg/day during the study.
Editor’s Note: The potential mechanism of this effect makes sense. Lamotrigine decreases release of glutamate, and memantine blocks glutamate’s actions at the NMDA receptor. Thus the two together would more efficiently decrease glutamate’s effects.
It is possible that memantine could be effective without effecting the normal functions of glutamate. The drug blocks NMDA glutamate receptors that are situated away from the synapse, while allowing NMDA glutamate receptors at the synapse to fulfill their normal functions that support learning and memory. The blocking of only those receptors outside the synapse (extra-synaptic) could explain why memantine has relatively few side effects.
Lamotrigine Effective Adjunct for Lithium in Bipolar Disorder
 In a long-term study of bipolar patients taking lithium published in Bipolar Disorders last year, the addition of lamotrigine (or paroxetine for those who did not respond to lamotrigine) was significantly better than the addition of placebo. Patients taking lamotrigine with lithium averaged 10 months until a recurrence of a depressive or manic episode, while patients taking placebo with lithium averaged 3.5 months until an episode.
In a long-term study of bipolar patients taking lithium published in Bipolar Disorders last year, the addition of lamotrigine (or paroxetine for those who did not respond to lamotrigine) was significantly better than the addition of placebo. Patients taking lamotrigine with lithium averaged 10 months until a recurrence of a depressive or manic episode, while patients taking placebo with lithium averaged 3.5 months until an episode.
Aripiprazole Makes Lamotrigine More Effective
 In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Rahman and colleagues reported that in patients being treated for bipolar disorder, the addition of atypical antipsychotic aripiprazole to maintenance treatment with lamotrigine was more effective than the addition of placebo to the same maintenance treatment with lamotrigine. Improvements in Young Mania Rating Scores (YMRS) with the combination of aripiprazole plus lamotrigine were significantly greater than that of lamotrigine plus placebo.
In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Rahman and colleagues reported that in patients being treated for bipolar disorder, the addition of atypical antipsychotic aripiprazole to maintenance treatment with lamotrigine was more effective than the addition of placebo to the same maintenance treatment with lamotrigine. Improvements in Young Mania Rating Scores (YMRS) with the combination of aripiprazole plus lamotrigine were significantly greater than that of lamotrigine plus placebo.
Editor’s note: These data add to a growing literature that shows that an atypical antipsychotic added to a mood stabilizer is associated with better prophylactic effects than use of the mood stabilizer alone. Previously, most of the studies of this type of combination used lithium or valproate as the mood stabilizer and, to our knowledge, this is the first to demonstrate that long-term prevention with lamotrigine is enhanced by the addition of an atypical antipsychotic.
Many of the atypical antipsychotics are FDA-approved as adjunctive treatments to mood stabilizers in the long-term treatment of bipolar disorder. The controlled clinical trial data that led to this FDA approval support the practice of many clinicians who prescribe combination treatment rather than monotherapy in order to achieve a more rapid onset of anti-manic stabilization and longer-term maintenance effects. The use of aripiprazole and quetiapine as adjuncts to lithium and valproate is particularly common in bipolar disorder since the same atypical antipsychotics are FDA-approved as adjunctive treatments in unipolar depression, and clinicians are familiar with prescribing them to improve ineffective acute antidepressant treatment.
Methylene Blue Successfully Augments Lamotrigine in the Treatment of Bipolar Disorder
 In a double-blind, placebo-controlled trial for patients with bipolar disorder, Martin Alda and colleagues from Dalhousie University in Halifax, Nova Scotia found that the compound methylene blue was an effective augmentation for mood stablizers. Methylene blue inhibits nitric oxide synthetase and guanylate cyclase, the overproduction of which might be associated with neuronal damage. Since bipolar disorder has consistently been associated with neuronal and glial cell dysfunction and loss, methylene blue could be a promising treatment.
In a double-blind, placebo-controlled trial for patients with bipolar disorder, Martin Alda and colleagues from Dalhousie University in Halifax, Nova Scotia found that the compound methylene blue was an effective augmentation for mood stablizers. Methylene blue inhibits nitric oxide synthetase and guanylate cyclase, the overproduction of which might be associated with neuronal damage. Since bipolar disorder has consistently been associated with neuronal and glial cell dysfunction and loss, methylene blue could be a promising treatment.
Methylene blue turns urine blue, so in place of a placebo the researchers used very low doses (15 mg daily) of methylene blue compared with the active dose of 195 mgs daily.
Thirty-seven patients were enrolled in the randomized 26-week trial, and all patients were treated with lamotrigine as their primary mood stabilizer and with any additional medications they were already taking. Patients entered in a well or euthymic state (n =20), mildly depressed (n=14), or while minimally cycling (n = 3).
Scores on both the Montgomery-Asberg Depression Rating Scale and the Hamilton Rating Scale for Depression improved significantly, with an effect size of 0.47 and 0.42, respectively. Hamilton Anxiety Rating Scale scores also improved significantly with an effect size of 0.46.
Methylene blue was well tolerated, with only transient and mild side effects observed. However, the FDA has issued a warning that using methylene blue with serotonin active agents can lead to a severe serotonin syndrome (because methylene blue is a potent inhibitor of MAO-A and will increase brain serotonin levels when used in conjunction with serotonin active antidepressants). Symptoms of serotonin syndrome can include confusion, hyperactivity, sweating, fever, shivering, diarrhea, trouble with coordination, and even seizures.
The researchers at Dalhousie University concluded that methylene blue used as an adjunctive medication to lamotrigine and other previously inadequately effective agents (only those which are NOT serotonin active) significantly improved depression and anxiety in patients with bipolar disorder. They proposed further exploration of the mechanisms involved in this change, with the possibility that other drugs with similar actions could also be effective in this disorder.
Dopamine D2 and D3 Agonist Pramipexole May Enhance Cognitive Function in Bipolar I Disorder
Anil Malhotra from the Zucker Hillside Hospital found that pramipexole (Mirapex), a dopamine D2 and D3 agonist used in the treatment of Parkinson’s disease, improved measures of processing speed and working memory in euthymic bipolar patients (whose average age was 42) when compared with placebo in an adjunctive clinical trial.
Editor’s Note: Bipolar patients in a euthymic phase have consistently been shown to have some degree of cognitive dysfunction that is typically correlated with the number of prior depressive and/or manic episodes they have experienced. This is one of the first studies to directly target this cognitive dysfunction with a pharmacotherapeutic agent.
Pramipexole may be of additional value among depressed patients, because in two small, placebo-controlled studies, one led by Carlos Zarate at the National Institute of Mental Health and one led by Joseph F. Goldberg in New York, pramipexole has been shown to exert acute antidepressant effects in bipolar patients in the depressive phase of the illness. The new data from Malhotra raise the possibility that there could be a two-for-one benefit when pramipexole is used in the depressive phase of bipolar illness—improvement in both depression and cognition.
Other approaches to improving cognition in patients with bipolar disorder
Lamotrigine for BP II depression: Not FDA-Approved, but Likely Effective
At the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March, Jae Seung Chang of South Korea reported that in a year-long naturalistic, open label study of long-term adjunctive lamotrigine therapy in 109 patients with bipolar II depression, depression severity decreased when lamotrigine was added to patients’ regular treatment with mood stabilizers.

Interestingly, in addition to the data on lamotrigine, these investigators also found that having had a higher number of prior episodes was associated with a decreased response to lithium, a finding that has often been reported in the literature. Another finding was that a history that included a serious suicide attempt was associated with a decreased lamotrigine response. Read more
Anti-Alzheimers’s Drug Memantine (Namenda) May Augment the Antidepressant Effects of Lamotrigine
 At the 65th Annual Scientific Convention of the Society of Biological Psychiatry in May, Amit Anand reported that the anti-Alzheimer’s drug memantine (20 mg/day) was superior to placebo in augmenting the acute antidepressant effects of lamotrigine. These data are of particular interest since one of the assumed mechanisms of action of lamotrigine is to decrease the release of glutamate.
At the 65th Annual Scientific Convention of the Society of Biological Psychiatry in May, Amit Anand reported that the anti-Alzheimer’s drug memantine (20 mg/day) was superior to placebo in augmenting the acute antidepressant effects of lamotrigine. These data are of particular interest since one of the assumed mechanisms of action of lamotrigine is to decrease the release of glutamate.
Memantine is a drug approved for the treatment of Alzheimer’s disease and is a partial antagonist (blocker) of glutamate NMDA receptors. This suggests that the dual actions of inhibiting glutamate’s release pre-synaptically (with lamotrigine) and blocking glutamate receptor activity post-synaptically (with memantine) combine to produce a better effect than that of lamotrigine alone.
Lamotrigine for Bipolar Disorder in Kids
Dr. Gagin Joshi of Massachusetts General Hospital reported the results of a study using lamotrigine (Lamictal) for 12 weeks in 39 children with bipolar disorder. Average dose was 160 mg/day and was titrated very slowly because of the increased risk of rash in children treated with lamotrigine compared with adults. Thirty-eight percent of the children achieved remission in mania, and 42% in depression.
In terms of side effects, 28% of individuals experienced gastrointestinal upset; 26% headache, 18% allergy, and 18% dermatological problems which led seven patients to discontinue the trial. However, none of the rashes were severe. This article is to be published in the journal CNS Science and Therapeutics this year.
One Expert’s Personal Treatment Algorithm for Bipolar Disorder in Young Children
EDITOR’S NOTE: Dr. Gagin Joshi of Massachusetts General Hospital, who presented the work on carbamazepine and lamotrigine on page 1 provided us with his own general treatment algorithm for youngsters with bipolar disorder.

Omega-3 Fatty Acids (photo from ironmagazine.com)
Joshi typically starts with 0.5 to 2 gms of omega-3 fatty acids because of their benign side-effects profile, the many studies suggesting they are effective in adult mood disorders, and a recent article indicating that they were effective in preventing the conversion of prodromal schizophrenia into full-blown illness in a randomized double-blind controlled study in Australia.
After the omega-3 fatty acids, Joshi’s second choice is typically the atypical antipsychotic aripiprazole (Abilify) because of its lesser degree of weight gain compared to atypicals quetiapine (Seroquel) or risperidone (Risperidol). Risperidone can be a third option if aripiprazole is not effective or tolerated.
Lamotrigine plus Valproate: Better than Lamotrigine Alone for Bipolar Depression
In a study comparing valproate monotherapy with the combination of lamotrigine and divalproex (Valproate) extended release (ER), the combination appeared more effective in bipolar depression. At the American College of Neuropsychopharmacology meeting in December 2009, Vivek Singh, Charles Bowen, Richard Weisler, and colleagues from The University of California, San Diego reported on the randomized, double-blind, eight-month maintenance study of bipolar depressed patients.
Patients who could be stabilized for two consecutive weeks on the combination treatment of both lamotrigine and divalproex were then randomized to either lamotrigine alone or the combination for the duration of the study. Most of the data collected about these 87 subjects favored the treatment with the combination (lamotrigine plus divalproex) compared with lamotrigine alone. Combination therapy was superior for manic symptomatology and resulted in lower rates of unanticipated worsening of depression (greater than 20 points on the Montgomery-Asberg depression rating scale (MADRS)) that led to termination from the study than lamotrigine monotherapy did.
Read more