An Inflammatory State Impedes Treatment for Bipolar Disorder
 A 2017 study by in the Journal of Clinical Psychiatry links inflammation to a poor antidepressant response in bipolar disorder. Many previous studies have found that elevated inflammatory markers are common in mood disorders, and that an inflammatory state seems to prevent response to certain therapies.
A 2017 study by in the Journal of Clinical Psychiatry links inflammation to a poor antidepressant response in bipolar disorder. Many previous studies have found that elevated inflammatory markers are common in mood disorders, and that an inflammatory state seems to prevent response to certain therapies.
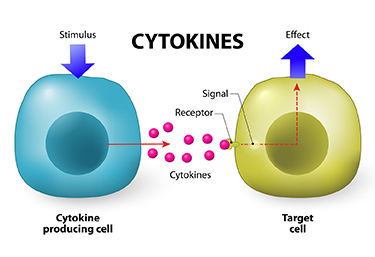
Researcher Francesco Benedetti and colleagues report that high levels of inflammatory cytokines (a type of small proteins) predicted a worse response to treatment with sleep deprivation and light therapy for bipolar depression. This treatment typically brings about a rapid antidepressant response.
Benedetti and colleagues measured 15 immune-regulating compounds in 37 patients who were experiencing an episode of bipolar depression and 24 healthy volunteers. Among those participants with bipolar disorder, 84% had a history of non-response to medication. Twenty-three of the 37 patients, or 62%, responded to the sleep deprivation/light therapy combination. Those who did not had higher levels of five cytokines: interleukin-8, monocyte chemoattractant protein-1, interferon-gamma, interleukin-6, and tumor necrosis factor-alpha.
Body mass index was correlated with cytokine levels and also reduced response to the treatment.
The finding supports a link between the immune system and mood disorders. Evaluating a patient’s level of inflammation may, in the future, allow doctors to predict the patient’s response to a given therapy. Patients with high levels of inflammation might benefit most from treatments that target their immune system.
Inflammation Predicts Poor Response to Sleep Deprivation with Light Therapy
A 2017 article by Francesco Benedetti and colleagues in the Journal of Clinical Psychiatry reports that people with bipolar depression who have higher levels of certain inflammatory markers may have a poor antidepressant response to the combination of sleep deprivation and light therapy, compared to those with lower levels of inflammation.
The study included 37 participants with bipolar disorder who were in the midst of a major depressive episode. Of those, 31 participants (84%) had a history of poor response to antidepressant medication. The patients were treated with three cycles of total sleep deprivation and light therapy within one week, a combination that can often bring about a rapid improvement in depression.
Depression improved in a total of 23 patients (62%) following the therapy. Blood analysis showed that compared to those who had a good response, the non-responders had higher levels of five intercorrelated inflammatory markers: IL-8, MCP-1, IFN-gamma, IL-6, and TNF-alpha. Those with higher body mass index had more inflammation, indirectly decreasing response to the therapy.
Midday Bright Light Therapy Improved Bipolar Depression
A study by Dorothy K. Sit and colleagues published in the American Journal of Psychiatry in 2017 found that delivering bright white light therapy to patients with bipolar depression between the hours of noon and 2:30pm improved their depression compared to delivering inactive dim light, and did not cause mood switches into mania. The study included 46 patients with moderate bipolar depression, no hypomania and no psychosis.
The active therapy group was exposed to broad-spectrum bright white fluorescent light at 7,000 Lux while the inactive group received dim red light at 50 Lux. Both groups were instructed to sit 12 inches from the light and face it without looking directly at it. The therapy began with 15-minute afternoon sessions and increased to 60 minutes per day by 4 weeks. Participants were assessed weekly. Remission rates increased dramatically in the active group beginning in the fourth week. At weeks 4 through 6, the remission rate for those in the active bright light group was 68.2% compared to only 22.2% in the dim light group.
Mean depression scores were better in the treated group, as were global functioning and response rates.
Some participants were taking antidepressants concurrently, and these participants were evenly distributed across the two study groups.
An earlier pilot study by the same researchers had found that bright light therapy delivered in the morning was followed by some hypomanic reactions or bipolar cycling. The midday sessions did not cause any mood switching.
Bright light therapy is often used to treat seasonal affective disorder (SAD) using a 10,000 Lux light box. This study took place mostly during the fall and winter months.
Editor’s Note: Bright light therapy is generally safe and boasts a high remission rate. Light boxes can be acquired without a prescription and are portable and easy to use. Midday light may have the best results and the least risk of provoking a mood switch into mania.
In Small Study, High Intensity Light Therapy Boosts Libido in Men
The same type of high-intensity light therapy used to treat seasonal affective disorder (SAD) and as an adjunctive treatment for non-seasonal depression has been found to boost testosterone and improve sexual satisfaction in men with low libido.
In a study by Andrea Fagiolini and colleagues, men with low sexual desire or trouble getting aroused were exposed to the high intensity light (10,000 Lux) for a half hour upon waking. Compared to men who used a lightbox that filtered the light to only 100 Lux, men exposed to the high-intensity light for two weeks showed increased testosterone in the blood and reported greater sexual satisfaction. Testosterone levels increased from around 2.1 ng/ml to 3.6 ng/ml in the high-intensity light group. (There were no significant changes in the comparison group.) Light therapy is quite safe for people without eye problems.
Fagiolini explained that in the Northern hemisphere, testosterone production declines from November to April and then rises again through the spring and summer, peaking in October. He suggests that the light therapy mimics the effect of summer light on the body, perhaps by inhibiting the pineal gland, which secretes hormones.
Fagiolini and colleagues hope to replicate the study with a greater number of participants and to determine how long the results may last.The study of 38 participants was presented at the 29th Congress of the European College of Neuropsychopharmacology in 2016.
Light Therapy Effectively Treats Non-Seasonal Depression
Doctors have known for some time that treatment with high-intensity light (7,000–10,000 Lux) can improve seasonal depression. In an 8-week study published in the journal JAMA Psychiatry in 2015, researcher Raymond Lam compared four different treatment options for non-seasonal major unipolar depression: bright light therapy for 30 minutes per day first thing in the morning, 20 mg of the antidepressant fluoxetine per day, combined bright light therapy and fluoxetine, and a placebo device paired with a placebo pill.
The combination of bright light therapy and fluoxetine produced remission in 58.6% of the participants who received it, compared to remission rates of 43.8% for bright light alone, 19.4% for fluoxetine alone, and 30% for placebo. It is notable that the effects of fluoxetine did not exceed those of placebo, but the effects of light alone did. There were few side effects in any group.
These data provide convincing evidence of the efficacy of light therapy in the treatment of non-seasonal unipolar depression. Use of light therapy for non-seasonal depression should now be more routinely considered, particularly when combined with antidepressant treatment.
Patients who had previously failed to respond to two or more antidepressants and patients with bipolar depression were excluded from the study. Bright light therapy administered in the morning can sometimes bring about mixed states in people with bipolar disorder. A 2007 case study by D. Sit and colleagues in the journal Bipolar Disorders found that midday light led to more improvement and less risk of mixed states than morning light among women with bipolar disorder.