In Mice, Knockout of Circadian CLOCK Genes Resembles Mania
Colleen McClung reviewed and extended previous findings of hers that knocking out a gene known as CLOCK in mice could reproduce most aspects of bipolar mania, including symptoms such as hyperactivity; decreased sleep; less depression; more impulsivity, risk taking, and novelty seeking; and increased reward-seeking including substances such as cocaine, alcohol, and sucrose. This syndrome in mice can be reversed by giving the mice lithium and valproate.
Knocking out the CLOCK gene produced an increased firing rate and burst firing of dopamine neurons in the ventral tegmental area (VTA). Localized knockout of the CLOCK gene in the VTA alone also reproduced the increase in dopamine cell firing.
When McClung and colleagues knocked out CLOCK in the medial prefrontal cortex, the normal development of a type of neurons called GABAergic parvalbumin interneurons did not occur in adolescent mice, and in adulthood, certain neural nets did not mature, leading to increases in oxidative stress, mitochondrial and cellular dysfunction, and the behavioral abnormalities that resembled mania. This animal model thus gives insight into how a genetic deficit in circadian rhythm genes in humans could influence the timing of behavioral abnormalities starting in adolescence and lasting through adulthood.
Lithium Reverses Thinning of the Cortex That Occurs in Bipolar Disorder
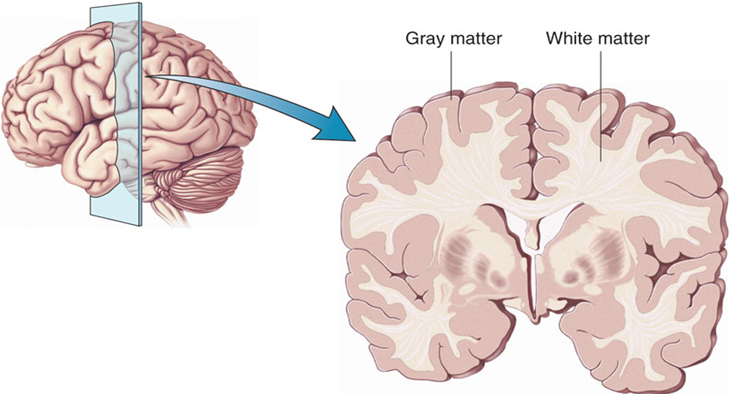
In a 2018 article in the journal Molecular Psychiatry, researcher Derrek P. Hibar reported findings from the largest study to date of cortical gray matter thickness. Researchers in the ENIGMA Bipolar Disorder Working Group, which comprises 28 international research groups, contributed brain magnetic resonance imaging (MRI) from 1837 adults with bipolar disorder and 2582 healthy control participants.
Hibar and colleagues in the working group found that in adults with bipolar disorder, cortical gray matter was thinner in the frontal, temporal, and parietal regions of both brain hemispheres. They also found that bipolar disorder had the strongest effect on three regions in the left hemisphere: the pars opercularis, the fusiform gyrus, and the rostral middle frontal cortex.
Those who had had bipolar disorder longer (after accounting for age at the time of the MRI) had less cortical thickness in the frontal, medial parietal, and occipital regions.
A history of psychosis was associated with reduced surface area.
The researchers reported the effects of various drug treatment types on cortical thickness and surface area. In adults and adolescents, lithium was associated with improvements in cortical thickness, and the researchers hypothesized that lithium’s protective effect on gray matter was responsible for this finding. Antipsychotics were associated with decreased cortical thickness.
In people taking anticonvulsant treatments, the thinnest parts of the cortex were the areas responsibly for visual processing. Visual deficits are sometimes reported in people taking anticonvulsive treatments.
Small Percentage of Patients Do Not Re-Respond After Stopping Lithium
 Researcher Ralph Kupka reviewed the literature on the small subgroup of patients who do well on long-term lithium treatment, stop taking the drug, suffer a relapse, and then fail to re-respond as well as they had (or, in some cases, at all) once they begin taking lithium again. These observations are supported by small case series, and appear to occur in approximately 10 to 15% of patients who stop taking lithium. Slowly tapering off lithium treatment did not seem to influence whether or not patients would re-respond to lithium later, while there was some indication that more time off lithium could lower the likelihood of a good re-response.
Researcher Ralph Kupka reviewed the literature on the small subgroup of patients who do well on long-term lithium treatment, stop taking the drug, suffer a relapse, and then fail to re-respond as well as they had (or, in some cases, at all) once they begin taking lithium again. These observations are supported by small case series, and appear to occur in approximately 10 to 15% of patients who stop taking lithium. Slowly tapering off lithium treatment did not seem to influence whether or not patients would re-respond to lithium later, while there was some indication that more time off lithium could lower the likelihood of a good re-response.
Earlier data from researcher Trisha Suppes suggested that slowly tapering off lithium treatment (over about two weeks) is superior to tapering rapidly (over a few days), and a slow taper reduced the rate of relapse. Kupka added that he would taper lithium even more slowly (over a period of one to two months) so that early signs of relapse could more readily be observed.
Optimum Lithium Levels
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Willem Nolen discussed optimal lithium levels to prevent episodes of bipolar disorder. Based on the limited number of controlled trials that have examined this issue and a survey of experts in the field, Nolen concluded that the standard dosing target to prevent bipolar episodes would be a blood concentration of 0.6 to 0.8 mEq/liter. This concentration could be dropped to 0.4 to 0.6 mEq/liter for patients who responded well to a higher dosage but needed to reduce side effects, and the concentration could be increased to 0.8 to 1.0 mEq/liter for patients who tolerated lithium treatment but showed an inadequate response.
There was no consensus as to optimal blood concentrations of lithium to prevent bipolar episodes in children and adolescents, but some researchers endorsed the same standard recommended for adults. For elderly patients, the majority of researchers recommended a slightly lower concentration of 0.4 to 0.6 mEq/liter, with the option to increase to a maximum of 0.8 mEq/liter in those under age 80 and 0.7 mEq/liter in those over age 80.
Lithium Reverses Some White Matter Abnormalities in Youth with Bipolar Disorder
 Multiple groups of researchers have reported the presence of white matter tract abnormalities in patients with bipolar disorder. Some of these abnormalities correlate with the degree of cognitive dysfunction in these patients. These white matter tract abnormalities, which are measured with diffusion tensor imaging (DTI), are widespread and can appear as early as childhood in people with bipolar disorder. Researcher Vivian Kafantaris mentioned at the 2019 meeting of the International Society for Bipolar Disorders that lithium treatment in children and adolescents normalizes these alterations, as described in an article she and her colleagues published in the journal Bipolar Disorders in 2017.
Multiple groups of researchers have reported the presence of white matter tract abnormalities in patients with bipolar disorder. Some of these abnormalities correlate with the degree of cognitive dysfunction in these patients. These white matter tract abnormalities, which are measured with diffusion tensor imaging (DTI), are widespread and can appear as early as childhood in people with bipolar disorder. Researcher Vivian Kafantaris mentioned at the 2019 meeting of the International Society for Bipolar Disorders that lithium treatment in children and adolescents normalizes these alterations, as described in an article she and her colleagues published in the journal Bipolar Disorders in 2017.
Editor’s Note: This is another reason to consider the use of lithium in children with bipolar disorder. Lithium treatment may help normalize some of the earliest signs of neuropathology in the illness.
Lithium FDA-Approved for Bipolar Disorder in Children 7–17
 In April 2019, the US Food and Drug Administration approved lithium for both the acute treatment of mania and for ongoing maintenance treatment of bipolar disorder in children and adolescents aged 7 to 17. Combined analysis of several studies indicates that lithium is effective and well-tolerated in both children and adolescents with bipolar disorder, both for acute treatment and to prevent bipolar episodes.
In April 2019, the US Food and Drug Administration approved lithium for both the acute treatment of mania and for ongoing maintenance treatment of bipolar disorder in children and adolescents aged 7 to 17. Combined analysis of several studies indicates that lithium is effective and well-tolerated in both children and adolescents with bipolar disorder, both for acute treatment and to prevent bipolar episodes.
Early Predictors of Suicide and Lithium as an Anti-Suicide Drug
 At the 2019 meeting of the International Society for Bipolar Disorders, researcher Gin S. Malhi discussed early predictors of suicide in people with bipolar disorder, such as younger age of illness onset, early life stressors, and family history of suicide. Impulsivity, hopelessness, cognitive deficits and substance use are risk factors, both for suicide in general and for an imminent suicide attempt. Proximal risk factors that indicate someone may make a suicide attempt soon include: mood swings, rapid cycling, increased depression, hospitalization, and severe anxiety.
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Gin S. Malhi discussed early predictors of suicide in people with bipolar disorder, such as younger age of illness onset, early life stressors, and family history of suicide. Impulsivity, hopelessness, cognitive deficits and substance use are risk factors, both for suicide in general and for an imminent suicide attempt. Proximal risk factors that indicate someone may make a suicide attempt soon include: mood swings, rapid cycling, increased depression, hospitalization, and severe anxiety.
Editor’s Note: Among all psychotropic drugs, lithium has the best data supporting its anti-suicide effects, both at therapeutic doses in patients with bipolar disorder and at trace levels in the water supply in the general population. People who live in locations where more lithium is naturally present in the water supply have lower rates of suicide than those who live in places with less lithium in the water. Malhi also noted that the antioxidant N-acetylcysteine (NAC), which has positive effects on mood and habitual behaviors, can reduce the incidence of lithium-induced dysfunction of the kidneys.
Family History of Lithium Response A Potent Predictor of Lithium Effectiveness
Researcher Martin Alda and colleagues reported at a 2018 scientific meeting that a family history of good response to lithium is highly predictive of response to lithium in a current bipolar patient. A good prospective response to lithium was seen in 68.6% of patients with a family member who responded well to lithium. Only 22% of those without a family member with a positive lithium response responded well to lithium.
Editor’s Note: Other predictors of a good response to lithium include: a family history of mood disorder, classical euphoric mania with clear-cut well intervals between episodes, lack of a simultaneous anxiety or substance abuse disorder, starting lithium early rather than late in the course of illness after many episodes or rapid cycling has occurred, and a sequential pattern of episodes of mania followed by depression, and then an interval of wellness (i.e. M-D-I rather than D-M-I). Even in those without these characteristics, lithium has many benefits including neuroprotection, reduction of suicide risk, and improved medical health (perhaps through its ability to increase the length of telomeres which are bits of DNA at the end of each chromosome). Longer telomeres are protective, while people with shorter ones may be vulnerable to some medical and psychiatric illnesses.
Lithium Superior to Other Mood Stabilizers in a Longitudinal Study of Bipolar Youth
At a late-2018 scientific meeting, researcher Danella Hafeman and colleagues reported some results of the Course and Outcome of Bipolar Youth (COBY) study. The study includes long-term follow up of 413 youth with bipolar disorder, who ranged in age from 7 to 17 years old. Hafeman and colleagues reported that taking lithium more than 75% of the time was linked to fewer suicide attempts, fewer depressive symptoms, and fewer psychosocial difficulties than taking another mood stabilizer (such as an atypical antipsychotic, lamotrigine, or valproic acid) more than 75% of the time after adjusting for demographic variables.
Despite the limitations of observational studies such as this one, the authors concluded, “Our findings are consistent with studies in adult populations, showing that lithium (compared to other mood stabilizers) is associated with decreased suicidality, less depression, and better psychosocial functioning. Given the paucity of evidence regarding lithium in children and adolescents, these findings have important clinical implications for the pharmacological management of youth with [bipolar disorder].”
Editor’s Note: These observations are consistent with several other studies. Researcher Barbara Geller and colleagues observed in eight years of follow up of children diagnosed with bipolar disorder that those who were treated with lithium spent more time in remission than those who took other medicines. A randomized controlled study by researcher Robert Findling and colleagues documented that maintenance lithium treatment was more effective than placebo at preventing bipolar episodes. Together, these data suggest that lithium should be used more often in the long-term treatment of children with bipolar disorder.
Way ahead of his time in about 1993, the renowned child psychiatrist Dennis Cantwell said something like this: “If I had an adolescent child with a first manic episode, I would have him stay on lithium for the rest of his life.” He seems to have been prescient, as evidence of the many benefits of lithium over other alternatives in the treatment of both children and adults has been accumulating.
An open-access review article this editor (Robert M. Post) published in the journal Neuropsychopharmacology in 2017, “The New News about Lithium: An Underutilized Treatment in the United States,” argues that lithium’s many benefits have been underestimated, while its side effects have been overestimated. It is my view that it would be beneficial if lithium were more often included in the treatment regimen of adults as well as children and adolescents with bipolar disorder.
Lithium has an astounding range of effectiveness. It prevents recurrent depressions and suicide (even in those with unipolar depression), increases hippocampal and cortical volume, protects memory, and increases the length of telomeres (the end portions of chromosomes that protect them as they replicate). In multiple animal models of neurological diseases, it has also been found to be neuroprotective and to reduce the size of brain lesions.
Risk of Suicide in People with Bipolar Disorder: Lowest with Lithium, Highest with Antidepressants
Researcher Markku Lähteenvuo and colleagues reported in the journal JAMA Psychiatry in early 2018 that long-acting injectable antipsychotics and lithium were best at preventing re-hospitalization in 18,018 bipolar patients in Finland who received an average of more than 7 years of follow up. Lähteenvuo and colleagues have now gone on to analyze suicide data from the same cohort of patients with bipolar disorder, and report that those taking lithium had the lowest rate of suicide, while those taking valproate had the next lowest suicide rate. Those patients with bipolar disorder who were treated with antidepressants had the greatest suicide rate. The suicide rate was particularly high for those once-hospitalized patients taking the MAO inhibitor antidepressant meclobemide, which is not approved for use in the US. Increased rates of suicide were also seen with use of sedatives and benzodiazepines.
Editor’s Note: Evidence continues to mount that lithium should be the definitive first line therapy in bipolar disorder for a multitude of reasons (as this editor Robert M. Post reviewed in an open-access article in the journal Neuropsychopharmacology in 2017). Still, lithium is not often prescribed for people with bipolar disorder in the US, and this does not seem to be in these patients’ best interests.
Use of antidepressants in bipolar disorder has remained controversial, but it is common in clinical practice despite a lack of evidence that it is effective, and the presence of some evidence that it is actually harmful. Antidepressant use in a person with bipolar disorder may cause switching into mania, cycle acceleration, dysphoria induction, and even suicide.
Clinicians should take these data seriously and overcome the impulse (leftover from treating unipolar depression) to use unimodal antidepressants as first line or adjunctive therapy for bipolar depression. Antidepressants are only effective in the long term in about 15% of patients with bipolar depression, and now it appears antidepressant use also carries an additional risk of suicide.