Lurasidone Effective Long-Term in Pediatric Bipolar Depression

At the 2020 meeting of the American Society of Clinical Psychopharmacology, researcher Manpreet Singh presented data showing that children aged 10–17 with bipolar depression had an excellent long-term response to the antipsychotic medication lurasidone (trade name Latuda).
Lurasidone has been approved by the US Food and Drug Administration as a monotherapy treatment of bipolar depression in children and adolescents since 2018. Following a six-week double-blind study comparing lurasidone with placebo in 305 children and adolescents, Singh and colleagues carried out an open-label extension study in which all of the young participants, including those in the placebo group, had the option of taking lurasidone for up to two more years.
Of those, 195 children completed one year of treatment, and 93 completed two years of treatment. Rates of response were 51.0% after the six-week preliminary study; 88.4% at one year; and 91.1% at two years. Rates of remission were 24.3% after the six-week study; 61.3% at one year, and 75.6% at two years, while rates of recovery were 17.7% after the preliminary study; 53.8% at one year; and 73.8% at two years.
This improvement in depression had a strong correlation with improvement in functioning, as measured by the Children’s Global Assessment score (CGAS). The results show progressive increases in rates of response, remission, and recovery with duration of treatment that are associated with improvement in functioning.
Lurasidone Highly Effective in Open Continuation in Youth with Schizophrenia
 Researcher Michael Tocco and colleagues reported at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) that in adolescents between the ages of 13 and 17 with schizophrenia, taking lurasidone for two years following a double-blind, placebo-controlled study led to steady improvement. There was a remarkably high 91% response rate and a 66% remission rate. Out of all the participants, 51.3% were rated as recovered.
Researcher Michael Tocco and colleagues reported at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) that in adolescents between the ages of 13 and 17 with schizophrenia, taking lurasidone for two years following a double-blind, placebo-controlled study led to steady improvement. There was a remarkably high 91% response rate and a 66% remission rate. Out of all the participants, 51.3% were rated as recovered.
Improvement in Bipolar Depression on Open-Label Lurasidone
Researcher Katherine Burdick and colleagues of Brigham and Women’s Faulkner Hospital and Harvard University reported in a poster at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) that youth between the ages of 10 and 17 with bipolar depression who continued taking lurasidone on a non-blind basis following a double-blind placebo-controlled six-week trial of the drug, or those who began taking lurasidone (for those who had been in the placebo group during the trial) saw improvement over a period of one to two years. All of the patients began the extension portion of the study at a dose of 20 mg/day.
Lurasidone appeared to be effective and well-tolerated. In addition, Burdick and colleagues reported a lack of cognitive difficulties in the youth taking lurasidone. Interestingly, a measure of visual learning substantially and progressively improved over the course of the study.
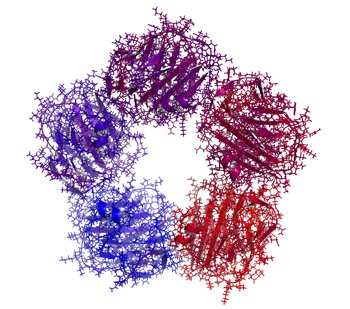
Baseline Levels of CRP Could Help Predict Clinical Response to Different Treatments
C-reactive protein, or CRP, is a marker or inflammation that has been linked to depression and other illnesses. People with high levels of CRP respond differently to medications than people with lower CRP, so assessing CRP levels may help determine which medications are best to treat a given patient.
High baseline levels of CRP (3–5pg/ml) predict a poor response to selective serotonin reuptake inhibitor antidepressants (SSRIs) and to psychotherapy, and are associated with increased risk of recurrent depression, heart attack, and stroke.
However, high baseline CRP predicts a better response to the antidepressants nortriptyline and bupropion. High CRP is also associated with better antidepressant response to infliximab (a monoclonal antibody that inhibits the inflammatory cytokine TNF alpha), while low levels of CRP predict worsening depression upon taking infliximab.
High baseline CRP also predicts good antidepressant response to intravenous ketamine (which works rapidly to improve treatment-resistant depression), minocycline (an anti-inflammatory antibiotic that decreases microglial activation), L-methylfolate (a supplement that can treat folate deficiency), N-acetylcysteine (an antioxidant that can improve depression, pathological habits, and addictions), and omega-3 fatty acids (except in people with low levels of DHA).
High baseline CRP also predicts a good response to the antipsychotic drug lurasidone (marketed under the trade name Latuda) in bipolar depression. In people with high baseline CRP, lurasidone’s positive results have a huge effect size of 0.85, while in people with low CRP (<3pg/ml) the improvement on lurasidone has a smaller effect size (0.35).
In personal communications with this editor (Robert M. Post) in 2018, experts in the field (Charles L. Raison and Vladimir Maletic) agreed that assessing baseline CRP levels in a given patient could help determine optimal strategies to treat their depression and predict the patient’s responsiveness to different treatment approaches.
At a 2018 scientific meeting, researchers Cynthia Shannon, Thomas Weickert, and colleagues reported that high baseline levels of CRP were associated with symptom improvement in patients with schizophrenia when they were treated with the drug canakinumab (marketed under the trade name Ilaris). Canakinumab is a human monoclonal antibody that targets the inflammatory cytokine interleukin-1 beta (Il-1b). Il-1b is elevated in a subgroup of patients with depression, bipolar disorder, or schizophrenia, and CRP levels are an indication of the associated inflammation.
High Baseline Levels Of C-Reactive Protein Predict Better Response To Lurasidone in Bipolar Depression
In a study presented at the 2017 meeting of the International Society for Affective Disorders, Charlies L. Raison and colleagues examined whether baseline levels of the inflammatory marker C-reactive protein (CRP) affected antidepressant response to the antipsychotic drug lurasidone in bipolar depression. The participants were divided into three double-blind groups: one received 20–60mg/day of lurasidone, another received 80–120 mg/day of lurasidone, and the third received placebo over a period of six weeks. The effect was dramatic—in people with CRP levels above 5 mg/L at the beginning of the study, lurasidone (at either dosage level) had a very large effect size (d=0.85), while in people with baseline CRP levels below 5 mg/L the effect size was smaller (d=0.35).
Interestingly, 118 of the participants (24.5%) had CRP levels above 5mg/L at baseline, indicating a substantial amount of inflammation was present in a quarter of the bipolar depressed patients. Higher levels of CRP at baseline were correlated with better improvement on specific items on the Montgomery–Åsberg Depression Rating Scale (MADRS): “lassitude” (or lack of energy), “apparent sadness,” “reported sadness,” and “pessimistic thoughts.” Raison and colleagues concluded: “These findings suggest that the efficacy of lurasidone in patients with bipolar depression may in part be linked to the inflammatory status of patients prior to treatment. If confirmed in prospective investigations, [the results of a wide-range CRP assay] may prove useful as a predictive biomarker that could help optimize the use of lurasidone for the treatment of patients with bipolar depression.”
Editor’s Note: In many instances, high levels of CRP predict a poor response to treatment (such as to selective serotonin reuptake inhibitor antidepressants (SSRIs) in unipolar depression), so these findings are of considerable interest. They also suggest the untested possibility that lurasidone has anti-inflammatory effects, as those with high levels of inflammation at baseline often respond better to drugs with direct anti-inflammatory effects such as celecoxib (Celebrex) or the antioxidant N-acetylcysteine (NAC).
FDA Approves Lurasidone for Bipolar Depression in Children and Adolescents
 In March 2018, the US Food and Drug Administration approved the antipsychotic drug lurasidone (Latuda) for the treatment of bipolar depression in children and adolescents aged 10–17 years. Lurasidone was already approved for adults with bipolar depression, as an add-on treatment to the mood stabilizers lithium and valproate, and for schizophrenia in people aged 13 years and up.
In March 2018, the US Food and Drug Administration approved the antipsychotic drug lurasidone (Latuda) for the treatment of bipolar depression in children and adolescents aged 10–17 years. Lurasidone was already approved for adults with bipolar depression, as an add-on treatment to the mood stabilizers lithium and valproate, and for schizophrenia in people aged 13 years and up.
A 6-week clinical trial in 347 youth compared lurasidone (in doses ranging from 20 to 80 mg/day) to placebo and found that those who received lurasidone showed significant improvements in depression compared to those who received placebo. The average dose was below 40 mg/day. The research by Melissa P. DelBello and colleagues was published in the Journal of the American Academy of Child and Adolescent Psychiatry in 2017.
In the study, lurasidone was well-tolerated. Side effects included nausea, sleepiness, minimal weight gain, and insomnia. Lurasidone did not seem to affect glucose, triglycerides, cholesterol, or blood pressure.
Editor’s Note: This is the first drug to be approved for bipolar depression in this age range. This editor (Robert M. Post) has written extensively on the high incidence of childhood onset bipolar disorder in the US, and especially in the offspring of parents with bipolar disorder.
It is important to be alert to the possibilities of depression and bipolar disorder in children in the US (along with related illnesses such as anxiety, oppositional defiant disorder, and attention deficit hyperactivity disorder (ADHD)), as early-onset illness tends to have a more severe long-term course than adult-onset depression and bipolar disorder. A longer delay between the emergence of symptoms and the first treatment for bipolar disorder is also a risk factor for more severe depression, more time depressed, and a poorer outcome in adulthood.
Parents of children aged 2-12 who have mood or behavioral problems are encouraged to consider joining the Child Network at our website, bipolarnews.org (click on the tab for the Child Network). By participating in this research network, parents are able to make a weekly rating of the severity of their children’s symptoms of anxiety, depression, ADHD, oppositional behavior, and mania via the secure website. The ratings can then be shared with the child’s clinicians for easy visualization of the course of symptoms over time, which may help with treatment decisions.
Lurisadone is Effective in Mixed Unipolar Depression
Lurasidone (Latuda) has been approved by the US Food and Drug Administration (FDA) for the treatment of bipolar depression. A new study indicates that lurasidone is also effective in those with unipolar depression complicated by a few manic features, i.e. mixed depression, which is often more severe and less responsive to traditional antidepressants than traditional unipolar depression.
At a 2015 scientific meeting, Andrew Nierenberg and colleagues presented the results of a six-week study comparing 20–60 mg of lurasidone to placebo in about 200 depressed patients who had some manic symptoms. Lurasidone significantly improved unipolar depressive symptoms in addition to the mixed manic symptoms.
At baseline, the patients’ manic symptoms included: flight of ideas/racing thoughts in 66.8% of the participants, pressured speech in 61.1%, decreased need for sleep in 40.8%, increased energy or activity in 28.0%, elevated or expansive mood in 18.0%, increased or excessive involvement in pleasurable activities in 15.6%, and inflated self-esteem or grandiosity in 6.6%.
Mixed Depression
Mixed depression describes a state of depression accompanied by a few symptoms typically associated with mania. At the 2015 meeting of the International Society for Bipolar Disorders, researcher Roger McIntyre shared some findings about mixed depression.
People with mixed depression have higher levels of MHPG, which is produced as the neurotransmitter norepinephrine breaks down. They also have higher levels of the stress hormone cortisol and their depressions are more difficult to treat. Those with unipolar mixed depression may respond poorly to traditional antidepressants.
There are also medical risks associated with mixed depression. People with mixed depression are more susceptible to cardiovascular disease than are people with depressive symptoms alone.
The drugs lurasidone, olanzepine, and ziprasidone have each shown efficacy in mixed depression.
Vitamin B6 May Reduce Restless Legs in Patients Taking Antipsychotics
The atypical antipsychotic lurasidone (Latuda) is one of only a few drugs effective at treating bipolar depression. But 5–10% of patients who take lurasidone experience akathisia, or restless legs.
At a recent meeting, psychiatrist Cynthia Turner-Graham told this editor (Robert Post) of her success in treating a patient with lurasidone-related akathisia that had been resistant to all the standard treatments, including dose reduction, anticholinergic drugs, benzodiazepines, beta-blockers, etc. Vitamin B6 at a dose of 600mg twice a day gave the patient complete relief.
Dr. Turner-Graham was kind enough to direct me to a small double-blind study supporting this clinical observation in patients with schizophrenia who experienced akathisia from treatment with antipsychotics. The study by V. Lerner and colleagues was published in the Journal of Clinical Psychiatry in 2004.
Atypical Antipsychotic Lurasidone Normalizes a Gene Important in Circadian Rhythms
Disruptions to circadian rhythms are common in mood disorders, leading some researchers to believe that normalizing these daily rhythms may improve the illnesses. Several genes, called CLOCK genes, are implicated in circadian rhythms. In animal studies, researcher Marco Riva and colleagues are examining the expression of CLOCK genes in different brain regions as a result of chronic stress that is meant to produce behaviors resembling human depression.
Male rats were exposed to chronic mild stress for two weeks, and divided into those that were susceptible to stress (identified by their loss of interest in sucrose) and those who were not. Then the rats were randomized to receive either a placebo treatment or 3 mg/kg/day of the atypical antipsychotic lurasidone (trade name Latuda), which has been effective in bipolar depression, during five more weeks of the stress procedure.
The researchers observed the expression of clock genes Clock/Bmal1, Per1, Per2, Cry1, and Cry2. In susceptible rats, the chronic mild stress decreased the clock genes Per1, Per2, and Cry2 in the prefrontal cortex. Lurasidone reversed these CLOCK gene abnormalities and the rats’ depression-like behaviors, which may explain some of the drug’s efficacy in bipolar depression.
Editor’s Note: Lurasidone is also a potent inhibitor of 5HT7 serotonin receptors, an effect that has been linked to antidepressant efficacy. Lurasidone also increases brain-derived neurotrophic factor (BDNF), which is important for learning and memory, and prevents stress from decreasing BDNF. Now it seems that lurasidone’s normalization of CLOCK genes may be another mechanism that explains the drug’s antidepressant effects.