How Stress Triggers Inflammation and Depression
 Depression and bipolar disorder are associated with increases in markers of inflammation that can be found in the brain and blood. It is increasingly clear that the mechanisms that cause depression are not just in the brain, but actually throughout the body. These include two signaling systems that begin in the bone marrow and the spleen.
Depression and bipolar disorder are associated with increases in markers of inflammation that can be found in the brain and blood. It is increasingly clear that the mechanisms that cause depression are not just in the brain, but actually throughout the body. These include two signaling systems that begin in the bone marrow and the spleen.
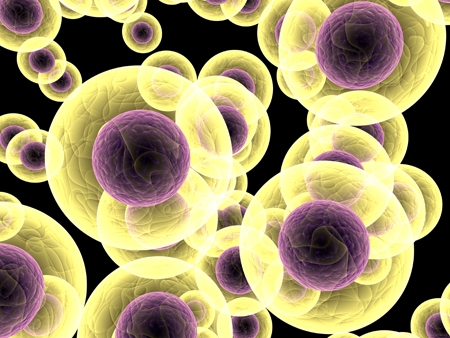
When a small mouse is repeated defeated by a larger animal, they show depression-like symptoms known as defeat stress. Animal studies have shown that stress and danger signals are perceived and relayed to the amygdala and the hypothalamus. The sympathetic nervous system releases the neurotransmitter norepinephrine into bone marrow, where stem cells are turned into activated monocytes (a type of white blood cells) that are then released into the blood. The monocytes travel to the brain, leading to the activation of more inflammatory cells.
Blocking part of this process can prevent the depression-like behaviors from occurring. If the bone marrow monocytes are blocked from entering the brain, inflammation and defeat stress behaviors like social avoidance do not occur. However, if there is a second bout of defeat stress, primed monocytes that have been stored in the spleen are released and travel to the brain, producing further increases in inflammatory cells and even more defeat stress behaviors.
If these monocytes from the spleen are blocked, the inflammation and the reaction to the new stressor do not occur.
Stress also activates lymphocytes (another type of white blood cells) to secrete the inflammatory cells Il-6. If this Il-6 secretion is inhibited, defeat stress behaviors can be prevented.
Defeat stress also leads to the release of the neurotransmitter glutamate. Some of this cascade begins in the brain, which evaluates stressors and releases IL-1 beta, another type of inflammatory cell. It slows down the production of glutamate, while IL-6 can endanger neurons and is associated with anhedonia—loss of interest in pleasurable activities. This cascade also leads to the production of another type of inflammatory cell, TNF-alpha, which has adverse effects on biochemistry, brain, and behavior.
This understanding of the role of the brain and body provides new targets for drug development. If inflammatory processes are blocked, defeat stress behaviors do not occur. Researcher Michael D. Weber and colleagues described this process in detail in the journal Neuropsychopharmacology Reviews in 2017.
Together these observations suggest that inflammatory processes in the body are crucial to the development of some stress- and inflammation-related depressive behaviors.
White Blood Cells Can Convey Resilience to Stress
Mice subjected to chronic defeat stress (being placed in the home cage of a larger, more aggressive mouse) behave in ways that resemble human anxiety and depression. In new research by Miles Herkenham and colleagues at the National Institute of Mental Health, in which they explored the adaptive immune system’s affect on mood, mice exposed to this type of stress showed increases in inflammatory cytokines in the blood (including TNFalpha, IL-1beta, IL-2, IL-3, IL-6, IL-17, and IFNgamma) compared to a control group. Interestingly, when white blood cells (lymphocytes) from stressed animals were transferred to a new set of animals, the recipient mice seemed to benefit from greater resilience to stress in a variety of ways.
Mice that received white blood cells from defeat-stressed animals had lower levels of TNFalpha, IL-1beta, IL-2, IL-3, and IL-17 than a control group that received white blood cells from unstressed mice. The recipient mice also exhibited reduced anxious and depressive behaviors in a litany of behavioral tests compared to both the group that received white blood cells from unstressed mice and a group that received a saline injection instead. Lastly, the recipients of the white blood cells from stressed animals showed more new neurons in the dentate gyrus of the hippocampus. (Hippocampal neurogenesis is decreased by stressors and increased by antidepressants.)
Herkenham and colleagues concluded that psychopathology is not just a downward spiral—the immune system plays an active role in adapting to stress, with lymphocytes being programmed by stress to provide antidepressant functions.
Editor’s Note: These data add a new twist to the studies of Scott Russo, who found that IL-6 secreted by white cells of animals subject to defeat stress was the cause of the depressive-like behaviors they exhibited. If IL-6 was blocked, the behaviors did not occur. Now it would appear from Herkenham’s work that something about the timing, the type of cytokines, or the transfer of the white cells conveyed protective antidepressant-like effects in this case.