Management of Unipolar and Bipolar Depression During Pregnancy
 At the Maryland Psychiatric Research Society’s continuing medical education conference in November, Lauren Osbourne, Assistant Director of the Women’s Mood Disorders Clinic at Johns Hopkins Hospital, gave a presentation on the management of mood and anxiety during pregnancy and lactation. She had a number of important ideas for physicians and patients to consider in their decision-making process.
At the Maryland Psychiatric Research Society’s continuing medical education conference in November, Lauren Osbourne, Assistant Director of the Women’s Mood Disorders Clinic at Johns Hopkins Hospital, gave a presentation on the management of mood and anxiety during pregnancy and lactation. She had a number of important ideas for physicians and patients to consider in their decision-making process.
According to Osbourne, 60%-70% of pregnant women with unipolar depression who discontinue their antidepressants relapse. Of those with bipolar disorder who discontinue their mood stabilizers, 85% relapse, while 37% of those who stay on their medications relapse.
Something to consider when deciding whether to continue medication while pregnant is that depression in pregnancy carries its own risks for the fetus. These include preterm delivery, low birth weight, poor muscle tone, hypoactivity, increased cortisol, poor reflexes, and increased incidence of attention deficit hyperactivity disorder (ADHD) and other behavioral disorders.
The placenta makes an enzyme 11-BHSD2 that lowers the stress hormone cortisol in the baby. However, this enzyme is less active in depression, exposing the fetus to higher levels of cortisol.
Thus, the decision about whether to continue medications during pregnancy should consider the risks to the fetus of both the mother’s depression and the mother’s medications.
Most antidepressants are now considered safe during pregnancy. There have been reports of potential problems, but these data are often confounded by the fact that women with more severe depression are more likely to require antidepressants, along with other risk variables such as smoking or late delivery (after 42 weeks). When these are accounted for by using matched controls, the apparent risks of certain antidepressants are no longer significant. This includes no increased risk of persistent pulmonary hypertension, autism, or cardiac malformations.
There may be a possible increased risk of Neonatal Adaption Syndrome (NAS) in the first weeks of life in babies who were exposed to selective serotonin reuptake inhibitor (SSRI) antidepressants in the third trimester. This syndrome presumably results from antidepressant withdrawal, and can include respiratory distress, temperature changes, decreased feeding, jitteriness/irritability, floppiness or rigidity, hypoglycemia, and jaundice. There is not yet a robust literature on the syndrome, but Osbourne suggested that it disappears within 2 weeks of birth.
In her practice, Osbourne prefers to prescribe sertraline, which has the best safety data, along with fluoxetine. Sertraline is also OK for breastfeeding. There is less data on bupropion, but it also appears to be safe during pregnancy. Endocrine and enzyme changes in pregnancy typically cause a 40% to 50% decrease in concentrations of antidepressants, so doses of antidepressants typically must be increased in order to maintain their effectiveness.
Osbourne ranked mood stabilizers for bipolar disorder, from safest to most worrisome. Lamotrigine is safest. There is no evidence linking it to birth defects, but higher doses are required because of increased clearance during pregnancy. Lithium is next safest. There are cardiac risks for one in 1,200 patients, but these can be monitored. Carbamazepine is third safest. One percent of babies exposed to carbamazepine will develop spina bifida or craniofacial abnormalities. Valproate is least safe during pregnancy. Seven to ten percent of babies exposed to valproate will develop neural tube defects, other malformations, or developmental delay, with a mean decrease of 9 IQ points. The atypical antipsychotics all appear safe so far.
Alternatives and Adjuncts to Medications in Pregnancy
Effectiveness of Continuation Right Unilateral ECT Plus Pharmacotherapy Compared to Pharmacotherapy Alone
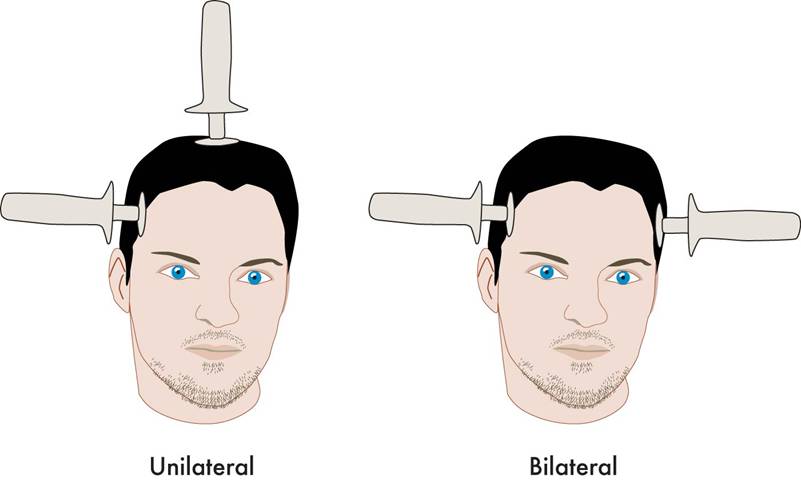
A new study is one of the first to find that after successful electroconvulsive therapy (ECT) treatment for depression, continuation of ECT together with pharmacotherapy was superior to continuation with pharmacotherapy alone. ECT produces a seizure while a patient is under anesthesia. The treatment has been successful in acutely treating many patients with severe depression who have not responded to other treatments. The question remains how to maintain the positive acute effects of ECT for a longer duration.
The new research was published in the Journal of ECT in 2013 by Axel Nordenskjöld et al. Patients with unipolar or bipolar depression who improved after an acute series of ECT (usually given 3 times per week) were randomized to receive either continuing ECT plus pharmacotherapy or pharmacotherapy alone. The ECT continuation group received weekly ECT for 6 weeks and every 2 weeks thereafter for a total of 29 ECT treatments in one year. The pharmacotherapy consisted of antidepressants (98%), lithium (56%), and antipsychotics (30%). Venlafaxine (Effexor) was considered the first choice for medication, and lithium augmentation was offered to all patients (not just those with bipolar depression). Of the participants, 64% had recurrent unipolar depression, while less than 20% had bipolar depression.
Among all the patients who were randomized at the beginning of the study (the intent-to-treat cohort), the one-year relapse rate was 61% for patients treated with pharmacotherapy alone and 32% for patients treated with the ECT plus pharmacotherapy (p=0.036). Relapse rates at 6 months were 54% for the pharmacotherapy alone group and 29% for the group receiving ECT plus pharmacotherapy. Some patients required inpatient care during the trial—36% of the patients in the pharmacotherapy alone group and 20% of those in the pharmacotherapy plus ECT group. There was no evidence of a differential effect on cognition across the two groups. (There is concern that bilateral ECT can adversely affect cognition, especially autobiographical memory, but this is not a concern with right unilateral ECT.)
Various parameters for ECT have been studied. This research used unilateral ultrabrief pulse ECT. These parameters are standard in Sweden, where the study took place, and these results are of particular interest as they differ from a US study that used bilateral ECT with treatments given more intermittently. In that study, in which response to ECT with pharmacotherapy did not differ from response to pharmacotherapy alone, ECT continuation was given in the form of 4 weekly treatments, 4 biweekly treatments and then 2 monthly treatments, and this regimen resulted in a relapse rate of 37% within 6 months (Kellner et al. 2006).
Only one other study in geriatric patients who were psychotically depressed showed superiority of continuation ECT.
Editor’s Note: The take-home message from this study may be that for patients with recurrent unipolar depression who respond positively to a course of right unilateral ultrabrief pulse ECT, continuation of regular ECT plus pharmacotherapy is worth considering over pharmacotherapy alone. While direct comparative studies have not been performed, it would appear reasonable to use weekly ECT for 6 weeks and then every 2 weeks thereafter for the continuation ECT treatment rather than a more intermittent series of treatments as in the studies of Kellner et al. Previous studies have shown that the addition of lithium to antidepressants is superior to antidepressants alone in the continuation phase of ECT (Sackeim et al. 2001), so having lithium in the regimen would also appear useful.
Most Online Pharmacies Fake, Says FDA
In late 2012, the Federal Drug Administration announced that 97% of online pharmacies violated state or federal laws and/or safety and practice standards set by the National Association of Boards of Pharmacy. Medications sold by fake pharmacies may be fake, expired, contaminated, not approved by the FDA, or unsafe.
Here are some warning signs that may mean an online pharmacy is fake:
- Allows you to buy medications without a prescription.
- Offers prices that are too good to be true.
- Sends spam emails offering discount prices.
- Is located outside the US.
- Is not licensed in the US
Real pharmacies are licensed by the state where they are located. They should provide a physical address and phone number, where you can reach a pharmacist who can answer your questions.
Track Your Moods with Life Charting
If you have unipolar depression or bipolar disorder and are having trouble stabilizing your mood, we recommend nightly charting of mood, medications and side effects on the easy-to-use Monthly Mood Chart Personal Calendar (pictured below) or the National Institute of Mental Health Life Chart (NIMH-LCM), both of which are available for download.
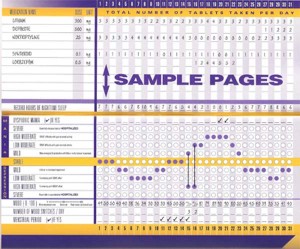
Sample Mood Chart
Click on the Life Charts tab above to download the personal calendar, which includes space for rating mood, functioning, hours of sleep, life events, side effects, and other symptoms such as anxiety. Then bring the chart to each visit with your physician to help in the assessment of treatments.
Life charting can help determine which medications are working partially and need to be augmented further, and which need to be eliminated because of side effects. Since there are now many potential treatments for depression and bipolar disorder (some FDA-approved and some not), a careful assessment of how well each new treatment works for a particular patient is essential to finding the optimal treatment regimen.