Baseline Levels of CRP Could Help Predict Clinical Response to Different Treatments
C-reactive protein, or CRP, is a marker or inflammation that has been linked to depression and other illnesses. People with high levels of CRP respond differently to medications than people with lower CRP, so assessing CRP levels may help determine which medications are best to treat a given patient.
High baseline levels of CRP (3–5pg/ml) predict a poor response to selective serotonin reuptake inhibitor antidepressants (SSRIs) and to psychotherapy, and are associated with increased risk of recurrent depression, heart attack, and stroke.
However, high baseline CRP predicts a better response to the antidepressants nortriptyline and bupropion. High CRP is also associated with better antidepressant response to infliximab (a monoclonal antibody that inhibits the inflammatory cytokine TNF alpha), while low levels of CRP predict worsening depression upon taking infliximab.
High baseline CRP also predicts good antidepressant response to intravenous ketamine (which works rapidly to improve treatment-resistant depression), minocycline (an anti-inflammatory antibiotic that decreases microglial activation), L-methylfolate (a supplement that can treat folate deficiency), N-acetylcysteine (an antioxidant that can improve depression, pathological habits, and addictions), and omega-3 fatty acids (except in people with low levels of DHA).
High baseline CRP also predicts a good response to the antipsychotic drug lurasidone (marketed under the trade name Latuda) in bipolar depression. In people with high baseline CRP, lurasidone’s positive results have a huge effect size of 0.85, while in people with low CRP (<3pg/ml) the improvement on lurasidone has a smaller effect size (0.35).
In personal communications with this editor (Robert M. Post) in 2018, experts in the field (Charles L. Raison and Vladimir Maletic) agreed that assessing baseline CRP levels in a given patient could help determine optimal strategies to treat their depression and predict the patient’s responsiveness to different treatment approaches.
At a 2018 scientific meeting, researchers Cynthia Shannon, Thomas Weickert, and colleagues reported that high baseline levels of CRP were associated with symptom improvement in patients with schizophrenia when they were treated with the drug canakinumab (marketed under the trade name Ilaris). Canakinumab is a human monoclonal antibody that targets the inflammatory cytokine interleukin-1 beta (Il-1b). Il-1b is elevated in a subgroup of patients with depression, bipolar disorder, or schizophrenia, and CRP levels are an indication of the associated inflammation.
CRP, A Readily Available Marker of Inflammation, Predicts Response To Two Antidepressants
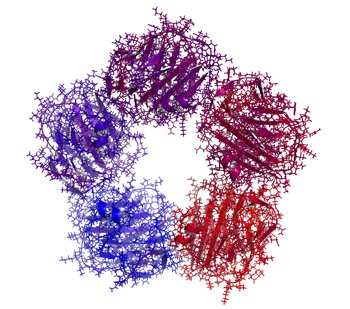
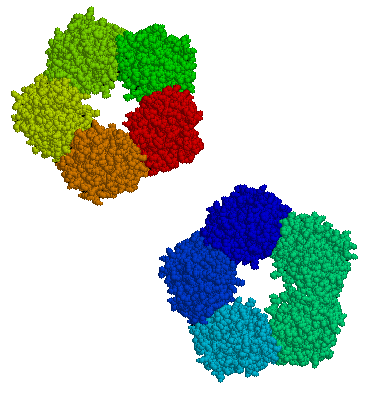
C-reactive protein, or CRP, is a protein found in blood plasma, the levels of which rise in response to inflammation. In a recent study, levels of CRP were able to predict which of two antidepressants a patient was more likely to respond to.
The 2014 article by Rudolph Uher et al. in the American Journal of Psychiatry reported that low levels of CRP (<1 mg/L) predicted a good response to the selective serotonin reuptake inhibitor (SSRI) escitalopram (Lexapro) while higher levels of CRP predicted a good response to the tricyclic antidepressant nortriptyline, a blocker of norepinephrine reuptake.
The research was part of the Genome-Based Therapeutic Drugs for Depression (GENDEP) study, a multicenter open-label randomized clinical trial. CRP was measured in the blood of 241 adult men and women with major depressive disorder. In the article the researchers say that CRP and its interaction with medication explained more than 10% of the individual variance in response to the two antidepressants.
If these findings can be replicated with these and similarly acting drugs, it would be a very large step in the direction of personalized medicine and the ability to predict individual response to medications.
Inflammatory Markers May Predict Antidepressant Response
There appears to be a link between inflammation and depression. In the journal Neuropsychopharmacology, Cattanes et al. reported in 2013 that compared to controls, depressed patients had significantly higher baseline levels of inflammatory cytokines, less glucocorticoid receptor function, less neuroplasticity, and fewer neuroprotective factors. Certain variables predicted response to treatment, others were seen only in responders, and still others changed in everyone with antidepressant treatment.
Higher baseline levels of inflammatory markers interleukin IB, macrophage inhibitory factor (MIF), and tumor necrosis factor TNF? were each associated with nonresponse to antidepressant treatment, and the three combined accounted for 50% of the variance in response—that is, they were the major predictor of whether a patient responded to treatment.
Levels of other factors changed in only those patients who responded well to antidepressants. The biggest changes were the normalization in levels of the neurotrophic factors BDNF and VEGF.
Several other markers normalized with antidepressant treatment regardless of whether the patients responded to treatment, and these included decreases in cytokines interleukin-IB and MIF and improved glucocorticoid receptor function.
The three different kinds of findings about these biomarkers were observed regardless of what type of antidepressant was used—SSRI versus tricyclic nortriptyline (which blocks norepinephrine reuptake).
Editor’s Note: This study replicates other studies in depression where signs of inflammation have been observed, including increases in inflammatory cytokines, decreases in glucocorticoid receptor function (needed to suppress high levels of the stress hormone cortisol) and lower levels of neuroplasticity and neuroprotection markers. This, however, is one of the first studies to show that levels of these markers at baseline may predict response to antidepressant treatment.
Also novel are the findings that while some high interleukin levels at baseline predicted antidepressant non-response, other ones normalized only in responders, and still others changed with treatment independent of whether the patients’ depression improved. These exciting findings require replication, but suggest the future possibility of personalized medicine, that is, choosing medications based on an individual biochemical marker profile. Eventually direct use of anti-inflammatory agents may be necessary in those with the highest levels of cytokines (predicting non-response to conventional antidepressant treatment). The same types of studies are needed in bipolar depression to determine the relationship between these inflammatory markers and treatment response.