Transcranial Direct Current Stimulation Plus Zoloft Has Better Antidepressant Effects Than Either Treatment Alone
 Transcranial direct current stimulation (tDCS), in which a barely perceptible level of electrical current is applied directly from one side of a patient’s scalp to the other, is a promising treatment for patients with tought-to-treat depression. A 2013 study by Brunoni et al. in JAMA Psychiatry examined whether combined treatment using tDCS and the selective-serotonin reuptake inhibitor (SSRI) antidepressant sertraline (Zoloft) would be a safe and effective treatment for unipolar depression. The combination was better than either treatment alone and better than placebo.
Transcranial direct current stimulation (tDCS), in which a barely perceptible level of electrical current is applied directly from one side of a patient’s scalp to the other, is a promising treatment for patients with tought-to-treat depression. A 2013 study by Brunoni et al. in JAMA Psychiatry examined whether combined treatment using tDCS and the selective-serotonin reuptake inhibitor (SSRI) antidepressant sertraline (Zoloft) would be a safe and effective treatment for unipolar depression. The combination was better than either treatment alone and better than placebo.
The six-week study used what is called a 2×2 factorial design, in which 120 patients with unipolar depression received either 50 mg/day of sertraline or placebo and also received either real tDCS or a sham procedure. The tDCS was administered in twelve 30-minute sessions, one per day Monday through Friday during the first two weeks, followed by one every other week. TDCS consists of an anodal (positive) and cathodal (negative) current placed at particular positions on the head. This study used 2 microamps of anodal left/cathodal right prefrontal stimulation for the tDCS treatment.
While the combination of sertraline and tDCS was significantly better than all three other treatment options (sertraline plus sham procedure, placebo plus tDCS, and placebo plus sham procedure), sertraline by itself and tDCS by itself resulted in similar efficacies. However, TDCS by itself was also significantly better than placebo, while sertraline by itself was not.
Side effects among the different treatment options were similar, except those who received tDCS had more scalp redness. There were seven instances of patients developing mania or hypomania during the study, five of which occurred in the combined tDCS and sertraline treatment group, higher than the 1–2% rate that would be expected in a study of unipolar depression.
Buspirone and Melatonin Together May Treat Unipolar Depression
The combination of the anti-anxiety drug buspirone (trade name Buspar) and melatonin, a hormone that regulates cycles of sleep and waking, may be effective for depression. Researcher Maurizio Fava and other researchers at Massachusetts General Hospital report that low-dose buspirone (e.g. 15 mg/day) combined with a 3 mg dose of melatonin produced significant antidepressant effects in a six-week study of patients with unipolar depression.
While buspirone is not a potent antidepressant at low doses, the combination of buspirone and melatonin exerted significant effects, leading to better antidepressant response than did either placebo or 15 mg of buspirone alone. Another benefit of the combination is that the low dose of buspirone minimizes side effects.
Buspirone is a serotonin 5HT1A receptor partial agonist, meaning that it produces weak activity at this serotonin receptor, but does not allow it to get overstimulated.
Cognitive Behavioral Therapy Tailored For Children and Adolescents
At a symposium on early-onset depression at the 2013 meeting of the American Academy of Child and Adolescent Psychiatry, Betsy Kennard described a course of cognitive behavioral therapy tailored to eliminating residual symptoms in children with unipolar depression who had no family history of a parent with bipolar disorder. In the same study Graham Emslie discussed, the investigators considered cognitive behavioral therapy for the treatment of childhood- and adolescent-onset depression.
The therapy was aimed at achieving health and wellbeing and focusing on positive attributes and strengths in the child, and it was designed to be a shorter than usual course (i.e. four weekly sessions, then four every other week, and one at three months). This regimen typically also included three to five family sessions. Other key components of the therapy included anticipating and dealing with stressors, setting goals, and practicing all the skills learned.
On a visual timeline, children identified and wrote down past stressors, how they felt when depressed, their automatic cognitions, ways they would know when they were feeling down again (i.e. feeling isolated, angry at parents, etc.), their strengths and skills, what obstacles to feeling better existed and how to circumvent them, and their long-term goals.
The therapy was based on the research of Martin Seligman and Giovanni A. Fava, plus Rye’s Six S’s (soothing, self-healing, social, success, spiritual, and self-acceptance). The children participated in practice and skill-building in each domain. Sleep hygiene and exercise were emphasized. The idea of “making it stick” was made concrete with phrases on sticky notes taken home and put up on a mirror. Postcards were even sent between sessions as reminders and for encouragement.
Editor’s Note: Most depressed kids don’t get completely well (only about 20% after an acute course of medication). Something must be added. This kind of specialized cognitive behavior therapy works and keeps patients from relapsing. This study included only those children with unipolar depression whose parents did not have bipolar disorder. However, Emslie noted that depressed children of a bipolar parent also had an exceedingly low rate of switching into mania (2 to 4%) in his experience, so fluoxetine followed by cognitive behavioral therapy might be considered for treating unipolar depressed children of a bipolar parent.
Once children have developed bipolar disorder, evidenced by hypomania or mania followed by depression, antidepressants are to be avoided in favor of mood stabilizers and atypical antipsychotics, since there is a higher switch rate in these youth when they are prescribed antidepressant monotherapy.
Since children with bipolar disorder are at such high risk for continued symptoms and relapses, the strategy of adding cognitive behavioral therapy to their successful drug treatment would appear appropriate for them as well as those with unipolar depression, especially since there is a large positive literature on the efficacy of cognitive behavioral therapy, psychoeducation, and Family Focused Therapy (FFT) in children and adults with bipolar depression. As noted previously, FFT is very effective for children at high risk because of a parent with bipolar disorder and who are already symptomatic with anxiety, depression or BP-NOS.
Moral of the story: getting kids with unipolar or bipolar depression well and keeping them well is a difficult endeavor that requires specialized, combined medication and therapy approaches and follow-up education and therapy. This is for sure. The hope would also be that good early and long-term intervention would yield a more benign course of recurrent unipolar or bipolar disorder than would treatment as usual (which all too often consists of medication only).
Irritability and Unipolar Depression in Kids
 At the 2012 Pediatric Bipolar conference sponsored by the Ryan Licht Sang Foundation, Graham J. Emslie gave a talk on irritable mood and unipolar depression in youth.
At the 2012 Pediatric Bipolar conference sponsored by the Ryan Licht Sang Foundation, Graham J. Emslie gave a talk on irritable mood and unipolar depression in youth.
Irritability is common in unipolar depression. Emslie suggested that if a child’s irritability is severe and the child destroys objects and denies being irritable, bipolar disorder might be likely. Irritable unipolar depressed children will generally acknowledge being irritable.
Emslie reported that 96% of youth in his randomized placebo-controlled studies of selective serotonin reuptake inhibitor antidepressants (SSRIs) recovered from their unipolar depression, but 46.6% relapsed. Those children with residual depressive symptoms were at double the risk for relapse into a depression compared to those who remitted completely. In those without residual depressive symptoms, there were no relapses if the children stayed on their medications.
Children were excluded from Emslie’s study if they had a positive family history of bipolar disorder, and perhaps because of this, very few participants switched into mania with antidepressants.
MORAL: Treat to remission and stay on the antidepressants associated with the remission. This has previously been found to be important for adults as well. (Emslie added that he would advise that a child stay on an antidepressant for at least a year after a remission was achieved, and longer if the child had difficulties in academic performance or relationships at school.)
Children with unipolar major depression who had a few manic symptoms at a subsyndromal level had poorer outcomes in Emslie’s study. The presence of subsyndromal manic symptoms in bipolar depressed adults is a risk factor for increased switching into mania when antidepressants are added to a mood stabilizer.
Comorbid substance abuse is another risk factor for poor outcome in childhood depression.
Long-term Outcomes for Childhood-Onset Disorders: Depression
A symposium at the 2012 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP) examined long-term outcomes of childhood onset disorders, including bipolar disorder, unipolar depression, ADHD, and anxiety disorder.
The Course of Childhood Onset Depression
Gabrielle Carlson presented the work of Karen Wagner on unipolar depression, in which there was a 15.3% incidence of unipolar depression in female adolescents, and 7.7% incidence in males. The overall incidence increased with age; from 8.4% in children aged 13, to 12.6% in children age 15 and 21.4% in children age 17. Average duration of a depressive episode was 17 months. While 85% recovered, 40% of those who recovered experienced a recurrence.
Carlson also presented data from Barbara Geller indicating that among children hospitalized with pre-pubertal onset of depression, 33% eventually were diagnosed with bipolar I disorder. If diagnoses of bipolar II and BP-NOS were included, the rate at which these children who got depressed before puberty eventually developing a bipolar disorder increased to an astonishingly high 49%. Thus, very early onset depression has a 50/50 chance of predicting an eventual bipolar disorder diagnosis.
Predictors of a more difficult course of depressive illness presentation were: earliest onset, more than 3 episodes, longer duration of depressive illness, and a positive family history. Those with early-onset depression had more suicidality, smoking, drug abuse, alcoholism, and an increased incidence of not having children when they became adults.
The Treatment for Adolescents with Depression Study (TADS) performed at the National Institute of Mental Health compared antidepressant response to fluoxetine, cognitive behavioral therapy (CBT), or the combination of fluoxetine plus CBT. Early in the study, the combination was most effective, with response in 39% of the children, compared to 24% for fluoxetine and 19% for CBT alone. However, after 3 years of follow up, all of the groups showed a relatively similar percent response: 60% for the combination; 55% for fluoxetine; and 64% for CBT.
N-acetylcysteine (NAC) Also Effective in Unipolar Depression
In 2008, Michael Berk and colleagues showed that N-acetylcysteine (NAC) is effective as an adjunctive treatment for bipolar depression. At the 2012 meeting of the International Congress of Neuropsychopharmacology, Berk reported that NAC (1000 mg twice a day) was also effective in unipolar depression, significantly beating placebo in a randomized double-blind 12-week study.
Editor’s Note: NAC has a broad spectrum of clinical efficacy in bipolar and unipolar depression, negative symptoms of schizophrenia (such as apathy and withdrawal), irritability in autism, trichotillomania (compulsive hair-pulling), gambling addiction, obsessive-compulsive disorder, and many substance-abuse disorders, such as cocaine, heroin, alcohol, and marijuana.
How can one substance do all this? NAC has antioxidant effects, it turns into glutathione (an antioxidant that is the body’s main defense against oxidative stress and free radicals), it has neuroprotective effects (causing neurite sprouting), and it re-regulates glutamate in the reward area of the brain, the nucleus accumbens. Berk believes it is NAC’s antioxidant properties that produce its positive effects in such a range of illnesses, while this editor (Robert M. Post) favors the glutamate mechanism (as discussed in BNN Volume 14, Issue 1 from 2010 and Volume 16, Issue 1 from 2012) as an explanation of NAC’s effects.
Whatever its mechanism turns out to be, NAC is worthy of consideration as an adjunctive treatment. It is readily available from health food stores without a prescription, relatively inexpensive (less than $20 for 100 pills), and relatively well-tolerated. Minor gastrointestinal upsets were the most common reported side effect in the Berk’s clinical trial. However, this editor has had one patient experience a worsening of psychosis.
Editor Robert M. Post’s Personal Opinion About NAC
With the usual caveat that all treatment strategies discussed in the BNN must be evaluated and administered by a physician, it may be useful to consider adding NAC to a treatment regimen for a patient struggling with recurrent unipolar or bipolar depression, and/or a comorbid substance use disorder. Using conventional treatments early in the course of these disorders for acute treatment and for long-term prevention would be the first approach. For less than satisfactory acute responses, conventional adjunctive treatments (as recommended in treatment guidelines elsewhere) might be considered along with NAC, which in some cases can have a delayed onset of action. (Three months may be required to see maximal effects in bipolar disorder.)
Antidepressants Work Better in Major Depressive Disorder than Previously Thought
As we’ve written before, the popular media has sometimes questioned the efficacy of antidepressants for unipolar depression. A reanalysis of data from previous controlled trials of fluoxetine and venlafaxine that was recently published in the Archives of General Psychiatry provides new evidence that these drugs are significantly more efficacious than placebo in youth, adult, and geriatric populations with major depressive disorder.
The researchers concluded,
To our knowledge, this is the first research synthesis in this area to use complete longitudinal person-level data from a large set of published and unpublished studies. The results do not support previous findings that antidepressants show little benefit except for severe depression. The antidepressants fluoxetine and venlafaxine are efficacious for major depressive disorder in all age groups, although more so in youths and adults compared with geriatric patients. Baseline severity was not significantly related to degree of treatment advantage over placebo.
The Risk-Benefit Ratio Encourages the Use of Antidepressants in Unipolar Depression
Wednesday we reviewed new data that shows that despite the FDA warning that antidepressants can increase suicidal ideation among young people in the first few months they are taken, antidepressants actually reduce acute suicidal ideation and decrease suicidal acts. As we described last year in our article on five myths about antidepressants, antidepressant treatment in recurrent unipolar depression is important to patients’ long-term wellbeing, cognitive functioning, and even life expectancy.
Untreated depression, and particularly untreated recurrent depression, carries high risks not only for lethality by suicide, but also for increases in medical mortality, particularly from cardiovascular disease. In addition to these medical risks, data from many studies suggest that a higher number of prior depressions is associated with increased cognitive dysfunction, and recent large data sets from a case registry in Denmark indicate that patients with four or more prior unipolar or bipolar depressive episodes have double the risk of receiving a diagnosis of dementia in old age. Thus, depressions are dangerous for a patient’s psychological, medical, and cognitive health.
Antidepressants Are Highly Effective in Depression Prevention
In 1992 researcher John Davis completed a meta-analysis of all antidepressant data available at the time in unipolar depression studies and not only found that antidepressant continuation was more effective than placebo in reducing the likelihood of later depressions, but also calculated that the statistical likelihood that this finding was due to chance was minuscule, i.e., p<10-34. John Geddes and colleagues in a meta-analysis in 2003 indicated that there was an approximate 70% reduction in the risk of depressive recurrences with antidepressant continuation compared with discontinuation.
Treatment of a first or second episode of unipolar depression is recommended for six to nine months following achievement of remission. After a third episode, all treatment guidelines of which this editor is aware recommend long-term preventive treatment with antidepressants, particularly if episodes have been severe or close together temporally. This long-term antidepressant continuation for prophylaxis is much like long-term treatment of high blood pressure or high cholesterol recommended for those with or at high risk for cardiovascular disease.
There is some evidence that cognitive behavior therapy reduces the risk for depressive recurrence in those discontinuing antidepressant treatment, but it appears maximally beneficial to engage both psychotherapeutic and pharmacological treatment to prevent future episodes. Read more
Antidepressants Prevent Suicide in Patients with Unipolar Depression
Researcher A. Kahn reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in Boca Raton in 2011 that severely depressed and suicidal patients taking citalopram (Celexa) or a combination of citalopram and low dose lithium experienced improvements in depression and suicidal thoughts. This study was unusual because most clinical trials exclude actively suicidal patients. In the group of subjects receiving citalopram plus lithium (300 mg/day and achieving 0.5 mEq/l or higher), there were several indications of better anti-suicide effects than in those on citalopram alone. The authors concluded that with appropriate doses, antidepressants plus lithium may prospectively reduce suicidal thoughts, and that it is possible to conduct clinical trials in severely depressed and suicidal patients if adequate safety measures are included.
Surprisingly, improvement in suicidal ideation preceded improvement in depressed mood per se.
Editor’s note: The study reported here suggests that in those with high suicidal ideation scores at baseline, antidepressants with or without lithium may quickly bring about anti-suicidal effects on thoughts, desires, and behaviors. Whether these effects occur reliably in studies in other groups of patients and in younger individuals remains to be established.
These data are an interesting contrast to data on antidepressant use in those with low levels of suicidality at baseline. A number of studies have suggested that in children and adolescents who were exposed to an antidepressant, a small percentage experienced increases in suicidal ideation in the first two months of treatment compared to patients taking placebo. This led to a Federal Drug Administration (FDA) warning (directed at all patients taking antidepressants) that increases in suicidal ideation and action may occur upon starting antidepressants.
It is important to note that the warning does not refer to completed suicides; the data set that led to the FDA warning included no completed suicides. More than 70% of those with suicidal ideation do not make an attempt, and the vast majority of attempts do not result in a completed suicide.
Most of the studies that found the slight increase in suicidal ideation in some patients after beginning antidepressant treatment actively excluded acutely suicidal patients. Since the study of citalopram and lithium above used a population of severely depressed and suicidal patients and found that antidepressants improved suicidality, it appears important to consider a patient’s baseline state when considering psychiatric interventions. In another example, there is an interesting difference between the way depressed patients and non-depressed normal volunteers respond to one night’s sleep deprivation: depressed patients often show dramatic improvement, while normal volunteers tend to feel worse.
More Evidence that Antidepressants Prevent Suicide in Unipolar Depression
A new study by DeLeon published in the Journal of Clinical Psychiatry in 2011 found that during periods of life when unipolar patients were taking antidepressants (compared to times when they were not taking them) the patients experienced 20% fewer suicidal acts or completed suicides. Read more
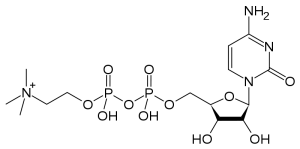
The Natural Substance Citicoline May Be Useful in Bipolar Disorder with Comorbid Stimulant Abuse
Sherwood Brown and colleagues from the University of Texas Southwestern Medical Center have completed a successful placebo-controlled trial of citicoline for bipolar and unipolar depression with comorbid methamphetamine dependence. Forty-eight participants with methamphetamine dependence and either unipolar or bipolar depression were randomized to either citicoline (2000 mg/day) or placebo for 12 weeks. Those receiving citicoline had significantly greater improvement in scores on the Inventory of Depressive Symptoms compared with those who received placebo, and patients receiving citicoline stayed in the study significantly longer, with completion rates of 41% on citicoline and 15% on placebo.
In 2007, the same team of investigators reported in the Journal of Clinical Psychopharmacology that citicoline had positive effects in bipolar patients with cocaine dependence, who experienced significant decreases in cocaine use and fewer cocaine-positive urine tests while taking citicoline.