Easier Vagal Nerve Stimulation Via the Ear
Vagal nerve stimulation (VNS) is an FDA-approved treatment for seizures and treatment-resistant depression. It typically requires an operation to insert a stimulator in a patient’s chest wall that delivers electrical impulses to their left vagus nerve via electrodes placed on the patient’s neck. New research by Bashar W. Badran and colleagues may have identified a less invasive and less expensive way to stimulate the vagal nerve—via electrodes placed on the ear.
The researchers tested different parameters for vagal nerve stimulation via the ear on 15 healthy volunteers and found that this type of VNS was feasible, tolerable, and reasonably safe. Among the different parameters tested, a stimulation pulse width of 500 microseconds at 25Hz had the greatest effect on heart rate, slowing it by about 4.25 beats per minute compared to a sham treatment.
Next Badran and colleagues plan to study the effects of this type of VNS on brain activity using functional magnetic resonance imaging (fMRI).
Over 5 Years, Vagal Nerve Stimulation Better than Treatment as Usual for Severe Depression
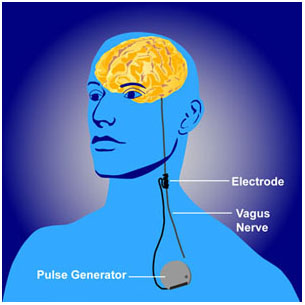 Vagal nerve stimulation (VNS) is an FDA-approved treatment for both seizures and depression that has resisted other treatments. It requires an operation for the insertion of a stimulator in the chest wall and electrodes on the left vagus nerve in the neck. A new study by Scott T. Aaronson and colleagues presented at the 2015 meeting of the Society of Biological Psychiatry observed severely depressed patients, 494 who received VNS and 301 who received treatment as usual in the community, over a period of five years. The patients who received VNS had greater response rates, they were more likely to have experienced remission, and their remissions lasted longer than those who received treatment as usual. Overall the patients who received VNS had lower mortality rates and suicide rates as well. VNS might be a good option for patients with depression that has not responded to most other treatments.
Vagal nerve stimulation (VNS) is an FDA-approved treatment for both seizures and depression that has resisted other treatments. It requires an operation for the insertion of a stimulator in the chest wall and electrodes on the left vagus nerve in the neck. A new study by Scott T. Aaronson and colleagues presented at the 2015 meeting of the Society of Biological Psychiatry observed severely depressed patients, 494 who received VNS and 301 who received treatment as usual in the community, over a period of five years. The patients who received VNS had greater response rates, they were more likely to have experienced remission, and their remissions lasted longer than those who received treatment as usual. Overall the patients who received VNS had lower mortality rates and suicide rates as well. VNS might be a good option for patients with depression that has not responded to most other treatments.
Brain Stimulation for Treatment-Resistant Depression
There are many methods of stimulating the brain directly, ranging from the very invasive to the non-invasive. Below we discuss deep brain stimulation, frontal lobe and vagal nerve stimulation, repeated transcranial magnetic stimulation, electroconvulstive therapy (in particular the new right unilateral ultra-brief pulse method), and low level magnetic fields.
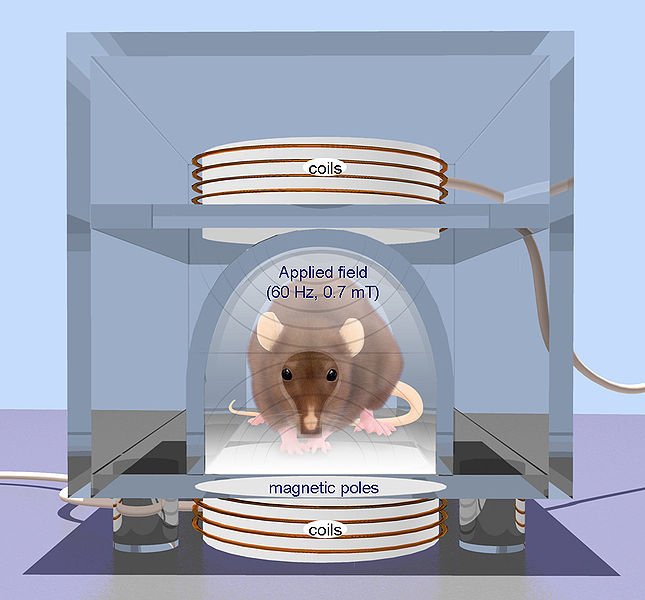
- Repetitive transcranial magnetic stimulation (rTMS) is a technique for noninvasive stimulation of the adult brain. Stimulation is produced by generating a brief, high-intensity magnetic field by passing a brief electric current through a magnetic coil. Compared with the growing number of clinical trial with rTMS, there are surprisingly few animal studies on its basic mechanisms of action, constraining the ability to perform hypothesis-driven clinical studies.
This is an Open Access image distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited. From: Arias-Carrión International Archives of Medicine 2008 1:2 doi:10.1186/1755-7682-1-2
Deep Brain Stimulation
At the American Psyciatric Association meeting in San Francisco in May 2009, Giacobbe et al. reported on the results of deep brain stimulation of an anterior-ventral part of the prefrontal cortex called the subgenual cingulate cortex in patients with refractory major depressive disorder. In deep brain stimulation, electrodes are inserted directly into the brain. Twenty-one patients received this treatment in an open study at sites in Canada at McGill University, the University of British Columbia, and the University of Toronto. This multi-center trial replicated results reported by Mayberg et al. (2005) with stimulation of what is also called Broadman’s area 25, or the part of the prefrontal cortex just under the anterior part of the corpus callosum (which carries fiber tracts between the left and right sides of the brain).
Read more


