Parents’ History of Mood and Anxiety Disorders Increases Risk of These Disorders in Offspring
A 2016 article by researcher Petra J. Havinga and colleagues in the Journal of Clinical Psychiatry suggests that offspring of a parent with a mood or anxiety disorder are at higher risk for these disorders than offspring from non-ill parents. Havinga and colleagues studied 523 offspring of parents with one of these disorders. Among these offspring, 38.0% had had a mood or anxiety disorder by age 20, and 64.7% had had such a disorder by age 35. (Rates of these disorders in the general population are closer to 10%.)
The risk of offspring developing one of these disorders was even higher when both parents had a history of a mood or anxiety disorder, when a parent had an early onset of one of these illnesses, and when the offspring was female. The good news is that balanced family functioning had a protective effect, reducing the likelihood that the offspring would develop a mood or anxiety disorder.
Researcher David Axelson reported in a 2015 study published in the American Journal of Psychiatry that approximately 74% of the offspring of a parent with bipolar disorder went on to have a major psychiatric diagnosis over 6.7 years of followup. Similarly, researcher Myrna Weissman and colleagues reported in 2006 that the same high incidence of psychiatric diagnoses was true of the offspring of a parent with unipolar depression over 20 years of followup.
Editor’s Note: It is important to be vigilant for mood or behavioral disorders that may emerge in the offspring of a parent with a mood or anxiety disorder. Children at high risk should maintain a healthy diet and good sleep hygiene, exercise regularly, and perhaps try practicing mindfulness and meditation, as recommended by researcher Jim Hudziak. Family-focused therapy (developed by researcher David Miklowitz) can help when early symptoms appear in the offspring of a parent with bipolar disorder.
Another option is joining our Child Network, a secure online program that allows parents to track their children’s symptoms of anxiety, depression, attention-deficit hyperactivity disorder (ADHD), oppositional behavior, and mania. This may facilitate earlier recognition and treatment of dysfunctional symptoms, which can be treated with psychotherapy and medication.
Recent Birth Cohorts May Have More Depression and Bipolar Disorder
In medicine, the ‘cohort effect’ describes the idea that more recent birth cohorts have an increased incidence and younger age of onset of their illness. A 2016 article by this editor (Robert M. Post) and colleagues in the Journal of Clinical Psychiatry presented evidence that younger patients with bipolar disorder have an earlier age of onset of bipolar disorder and more relatives with mood disorders than older patients with bipolar disorder.
The research was carried out by the Bipolar Collaborative Network in four US cities (Dallas, Cincinatti, Los Angeles, and Bethesda) and three northern European ones (Utrecht, Freiburg, and Munich). On both continents, patients born more recently had an earlier age of onset of their bipolar disorder. Younger patients also had parents and grandparents with a greater incidence of depression, bipolar disorder, and alcohol and substance abuse compared to older patients.
Editor’s Note: Other researchers have found evidence of a cohort effect for unipolar depression, substance abuse, and attention-deficit hyperactivity disorder (ADHD). The data indicate that childhood onset of psychiatric illnesses may be becoming more common. Research aimed at earlier detection and treatment is needed to reverse these trends.
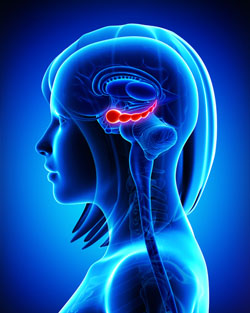
Specific Regions of Hippocampus Linked to Bipolar Disorder
It has been clear for some time that the volume of the hippocampus, a brain region implicated in mood and memory processing, plays a role in bipolar disorder. A 2017 article by researcher Bo Cao and colleagues in the journal Molecular Psychiatry links loss of volume in specific sub-regions of the hippocampus with bipolar disorder.
The study by Cao and colleagues used magnetic resonance imaging (MRI) and a special segmentation technique to compare the volume of certain hippocampal sub-regions across people with bipolar disorder, people with major depression, and healthy control participants.
Participants with bipolar disorder had lower volumes in subfield 4 of the cornu ammonis, two cellular layers (the granule cell layer and the molecular layer), and the tail part of the seahorse-shaped hippocampus compared to the other subjects. Participants with bipolar I disorder had particularly severe volume loss in these areas.
Cao and colleagues also found that volume loss progressed along with the illness. The volumes of the right cornu ammonis, the molecular layer, and the subiculum decreased further in patients who had bipolar disorder for longer. As manic episodes increased, the volume of both sides of the cornu ammonis and the hippocampal tail decreased.
Therapy Reduces Relapses, Promotes Medication Adherence
A 2017 meta-analysis published in the British Journal of Psychiatry indicates that psychosocial interventions were linked to reduced relapse rates, better adherence to medication, and other benefits in people with bipolar disorder. The meta-analysis by researcher Mary Lou Chatterton and colleagues evaluated data from 41 studies with a total of 3,119 participants. The studies examined psychosocial interventions such as cognitive-behavioral therapy, psychoeducation, and family-focused therapy compared to treatment as usual.
Chatterton and colleagues found that interventions that targeted family members who act as caregivers reduced manic and depressive relapse rates. Combined psychoeducation and cognitive-behavioral therapy was more successful than any other intervention, and had a large effect in reducing symptoms of mania. This combination also improved general functioning. Psychoeducation alone and in combination with cognitive behavioral therapy reduced medication non-adherence. Unfortunately, no intervention reduced depressive symptoms.
Mood Stabilizers with Atypical Antipsychotics Reduce Relapses Compared to Mood Stabilizers Alone or with Typical Antipsychotics
An Israeli study reports that treatment with mood stabilizers and atypical antipsychotics reduces bipolar relapses compared to treatment with mood stabilizers alone or mood stabilizers combined with typical antipsychotics. The study, by Eldar Hochman and colleagues in the journal Bipolar Disorders, compared one-year hospitalization rates after patients with bipolar disorder were discharged from the hospital following a manic episode. All of the 201 discharged patients were prescribed a mood stabilizer (lithium or valproate), and some were also prescribed an antipsychotic, either atypical or typical.
Those participants who received the combination of a mood stabilizer and an atypical antipsychotic had re-hospitalization rates of 6.3% compared to 24.3% of those who received mood stabilizers alone and 20.6% of those who received mood stabilizers with a typical antipsychotic.
While the study did not determine which treatment is best for ongoing maintenance treatment of bipolar disorder, it does suggest that the combination of mood stabilizers and atypical antipsychotics can reduce hospitalizations during the one-year period following a manic episode.
Lithium May Reduce Cancer Risk
New research suggests that cumulative exposure to lithium may correlate with reduced cancer risk in patients with bipolar disorder. A 2016 article by Yi-Hsin Yang and colleagues in the British Journal of Psychiatry reports findings from a Taiwanese population database study of 4,729 adult patients with bipolar disorder, 115 of whom were diagnosed with cancer. Those who had been prescribed lithium (with or without anticonvulsants) had lower rates of cancer (1.96%) than those who received only anticonvulsants (2.65%).
Incidence of cancer was higher among the patients with bipolar disorder than the general population in the study. Other studies have indicated that cancer risk is higher among people with bipolar disorder than those without.
Those people who took a recommended maintenance lithium dose for 215 days or longer had a 44.8% lower risk of cancer than those who took only anticonvulsants.
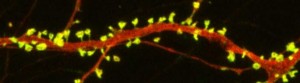
Lithium May Work by Restoring Dendritic Spines
New research on mice clarifies lithium’s effects on neurons and suggests how it can lead to improved symptoms. Dendrites are the long projections on neurons that seem to reach out to form synapses with other neurons. The surface of these dendrites is covered in mushroom-shaped spines that help create these synaptic connections. A 2016 article by research Ben Cheyette and colleagues in the journal Molecular Psychiatry reports that in mice with a genetic mutation common to people with autism, schizophrenia, and bipolar disorder, lithium restored healthy numbers of the mushroom-shaped spines. The lithium treatment also reversed symptoms such as lack of interest in social interactions, lack of motivation, and anxiety in the mice.
Cheyette and colleagues first identified a genetic mutation that affects signaling in what is known as the brain’s Wnt pathway. The mutation, while rare, is 80% more common in people with bipolar disorder, autism, and schizophrenia than in people without these disorders.
When the mice were given a similar mutation, they exhibited symptoms such as anxiety, decreased sociability, and lack of motivation. They also had reduced numbers of dendritic spines and impaired Wnt signaling.
Lithium can improve Wnt signaling by blocking an enzyme called GSK-3 beta that impairs the signaling.
Treating the mice with lithium restored their dendritic spines and improved their behavior.
Wnt signaling and dendritic spines may offer the key to lithium’s success in treating a variety of psychiatric disorders in people.
Combo of Memantine and Sertraline Effective for Unipolar Depression
A 2016 study in the Journal of Clinical Pharmacy and Therapeutics finds that the combination of memantine (Namenda), a drug used to treat Alzheimer’s disease, and the antidepressant sertraline (Zoloft) improved unipolar depression more than sertraline plus placebo.
The study by Meysam Amidfar and colleagues included 66 patients with moderate to severe unipolar depression. They were divided into two groups—one received sertraline plus memantine for six weeks, while the other received sertraline and a placebo.
The memantine group showed significantly greater improvement at 2 weeks, 4 weeks, and 6 weeks, and significantly greater response at 4 and 6 weeks. There were also more early improvers in the mematine group, and more rapid response to treatment. Both groups improved significantly over the six weeks of treatment.
Larger studies are needed to learn more about the safety and efficacy of memantine combined with sertraline for the treatment of unipolar depression, but this initial study is promising. In 2012, researcher Amit Anand and colleagues reported that in bipolar depression, memantine potentiates the effects of lamotrigine. Memantine also helped rapid cyclers when added to ongoing treatment in an open study of the drug treatment by Athanasios Koukopoulus and colleagues in 2012.
Immune Response to Repeated Stress Alters Behavior in Mice
In research presented at the 2016 meeting of the Society of Biological Psychiatry, Jonathan P. Godbout described how an immune reaction to repeated stressors may lead to anxious behaviors in mice.
Mice were repeatedly defeated by a larger animal, a form of stress that produces a depression-like state. This provoked an immune response in the mice—the release of a type of white blood cells called monocytes from the bone marrow into the circulatory system. These inflammatory monocytes then traveled to the brain and spleen, attracted by signaling proteins called chemokines. The monocytes in turn produced inflammatory marker interleukin-1beta.
The defeat stress also provoked a reaction in the central nervous system, where microglia were activated.
These changes produced inflammation and anxiety-like behaviors in the mice. Blocking the microglial activation, monocyte recruitment to the brain, or interleukin-1beta signaling each reversed the anxiety-like behaviors.
Another researcher, Scott Russo, has shown that leukocytes, another type of white blood cells, secrete inflammatory interleukin-6 following defeat stress, and blocking this secretion prevents defeat stress–related behaviors.
Only Fluoxetine is More Effective Than Placebo for Children and Adolescents with Depression
 In a meta-analysis published in 2016, researchers Andrea Cipriani, Xinyu Zhou, and colleagues reported that many antidepressants are not effective in children and adolescents. Fluoxetine alone was more effective than placebo. Other antidepressants also caused high study drop-out rates compared to placebo.
In a meta-analysis published in 2016, researchers Andrea Cipriani, Xinyu Zhou, and colleagues reported that many antidepressants are not effective in children and adolescents. Fluoxetine alone was more effective than placebo. Other antidepressants also caused high study drop-out rates compared to placebo.
In an article published in the journal The Lancet, Cipriani, Zhou, and colleagues analyzed 34 randomized, controlled clinical trials of antidepressants in children and adolescents. These trials included a total of 5,260 participants and 14 different antidepressants.
The researchers determined that much of the evidence was of a low quality. Only fluoxetine was statistically significantly more effective than placebo. Fluoxetine was also more tolerable to patients than duloxetine or imipramine. Patients who received imipramine, venlafaxine, or duloxetine were more likely to drop out of studies due to adverse events compared to patients who received placebo.
The authors suggest that prescribing antidepressants to children or adolescents may not necessarily be beneficial, and that fluoxetine is probably the best option to consider.
Editor’s Note: It may be best to use caution when prescribing antidepressants to children or adolescents. First, these data that suggest that many antidepressants are ineffective in young people. In addition, depression in children and adolescents may be a sign of bipolar disorder, and antidepressant use may cause activation or switching into mania in vulnerable patients.
While there is a warning about using antidepressants in young people because of the risk of increased suicidal ideation, the actual suicide rate in young populations decreases when these patients take antidepressants and cognitive behavioral therapy. Psychotherapy should be a high priority. Other safe adjunctive approaches might include omega-3 fatty acids, N-acetylcysteine, vitamin D3, and folic acid. Evidence for the efficacy of rTMS in young people is also positive and growing.