Galantamine Did Not Improve Cognitive Deficits in People with Bipolar Disorder
In a recent study by researcher Dan V. Iosifescu and colleagues, the drug galantamine, which is used to treat dementia, did not improve cognitive function in euthymic people with bipolar disorder. The drug had done so in earlier studies. Seventy-two participants with bipolar disorder that was in remission were randomized to receive either a placebo or galantamine extended release for a period of two weeks. Doses of galantamine ranged from 8 to 24 mg/day.
The participants took several tests of attention and memory over the course of the study. After 16 weeks of treatment, those taking galantamine did not show significant improvements in functioning compared to those who received placebo.
This research was presented at the 2016 meeting of the Society of Biological Psychiatry.
Inflammation Linked to Non-Response to Antidepressants
In a symposium on inflammation’s role in psychiatric disorders at the 2016 meeting of the Society of Biological Psychiatry, researcher Carmine Pariante reviewed the considerable literature indicating that major depression is often associated with measures of inflammation. Depression has been linked to elevated blood levels of the inflammatory proteins interleukin-1, interleukin-6, TNF alpha, and c-reactive protein, with about one-third of depressed patients having an elevated level of at least one of these proteins. People with elevated inflammatory markers are also less likely to respond to traditional antidepressants such as selective serotonin reuptake inhibitors (SSRIs).
Pariante reported that in depressed people, interleukin-6 is also elevated in cerebrospinal fluid in addition to blood, suggesting that inflammation in depression extends to the central nervous system. Increased secretion of interleukin-6 has been linked to depressive behaviors in mice exposed to stress.
There is some hope that anti-inflammatory treatments can help patients who do not respond to traditional antidepressant treatment. Some anti-inflammatory medications that may eventually be used to treat depression with inflammation include the COX-1 inhibitor aspirin, the COX-2 inhibitor celecoxib (Celebrex), or the antibiotic minocycline. Each of these approaches gained some support in preliminary clinical trials, but it has not yet been established that these anti-inflammatory treatments produce a better response in people with elevated inflammatory markers.
Methylene Blue May Help Bipolar Depression
 We have previously reported on the research by Martin Alda and colleagues that the chemical compound methylene blue had positive effects in patients with bipolar depression. The research was published in the British Journal of Psychiatry in 2016.
We have previously reported on the research by Martin Alda and colleagues that the chemical compound methylene blue had positive effects in patients with bipolar depression. The research was published in the British Journal of Psychiatry in 2016.
Now a new article by Ashley M. Feen and colleagues in the Journal of Neurotrauma reports that methylene blue has an antidepressant-like effect in mice with traumatic brain injury (TBI). Methylene blue reduced inflammation and microglia activation in the animals. Methylene blue reduced levels of the pro-inflammatory cytokine Il-1b and increased levels of the anti-inflammatory cytokine Il-10.
These findings are of particular interest as many patients with classical depression (and no brain injury) have abnormal levels of these inflammatory markers. It remains to be seen whether methylene blue is more helpful in those patients with elevated inflammatory markers and if levels of the markers can predict treatment response or not.
Methylene blue causes urine to turn blue, so low doses of the compound are used as a placebo. Alda and colleagues reported that the active dose 195mg reduced depression and anxiety significantly more than the placebo dose (15mg) in a 13-week crossover study. In that study, methylene blue was added to lamotrigine which had not had a complete enough effect.
In a 1986 study by G.J. Naylor and colleagues in the journal Biological Psychiatry, patients were treated with either 15mg/day or 300mg/day of methylene blue for one year and crossed over to the other dose in the second year. Participants had significantly less depression during the year of taking the active 300mg/day dose.
The FDA has issued a warning about the danger of a serotonin syndrome if methylene blue is combined with serotonin active agents (presumably because it inhibits MAO-A). Symptoms of the serotonin syndrome can include lethargy, confusion, delirium, agitation, aggression, decreased alertness, and coma. Neurological symptoms, such as jerky muscle contractions, loss of speech, muscle tension, and seizures; or autonomic symptoms, such as fever and elevated blood pressure, are also common. Patients should call their doctor if they are taking a serotonergic psychiatric medication and develop any of the above symptoms.
Creatine Supplements May Speed Up Response to Escitalopram, Improve Brain Connectivity
Antidepressants can take weeks to begin working, and researchers have been investigating ways to speed up this process. A 2012 study by In Kyoon Lyoo and colleagues in the American Journal of Psychiatry found that among 52 women taking the selective serotonin reuptake inhibitor (SSRI) antidepressant escitalopram (Lexapro) for unipolar depression, those who were prescribed an additional creatine supplement had earlier and greater decreases in depression symptoms than those who received a placebo in addition to the escitalopram.
The difference between the two groups was evident by the second week of treatment. At the end of the 8-week study, 52% of those who received creatine had achieved remission, compared to 26% of those in the placebo group.
Creatine, a supplement sometimes used by weightlifters, increases cellular energy. The women received 3g/day of creatine for the first week of the study, and 5g/day thereafter.
The same research group recently published more data from their creatine study. The new article by Sujung Yoon and colleagues in the journal Biological Psychiatry shows that following the creatine supplementation, the women in the creatine group had greater levels of N-acetylaspartate (a sign of healthy neurons) in their prefrontal cortex and also had greater levels of brain connectivity than women in the placebo group.
Cool Head May Help Insomnia
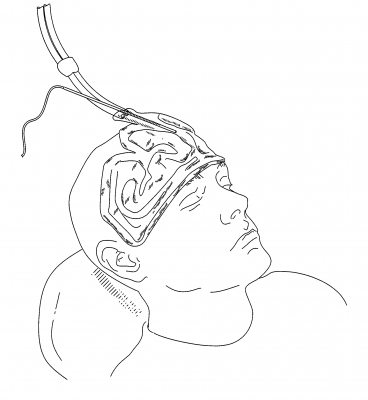
The US Food and Drug Administration recently approved a device that improves sleep by cooling the forehead. People with insomnia often have an active frontal cortex that keeps their thoughts racing as they try to fall asleep, preventing deeper, more restorative sleep. Through conducting functional brain imaging studies, researcher Eric Nofzinger found that cooling participants’ foreheads to a precise level during the night improved the quality of their sleep.
The sleep studies included more than 230 patients observed over 3800 research nights. One such study found that participants reached stage 1 and stage 2 sleep faster when they used the device.
Nofzinger founded the company Cerêve to produce the new bedside device, which pumps cooled fluid to a pad worn on the forehead. The company expects to release the device in 2017.
Insomnia may affect as many as 55 million Americans, frustrating them at night and leading to decreased alertness the following day. Sleeping pills are the most common treatment, but they can also cause impairment the following day.
In Small Study, High Intensity Light Therapy Boosts Libido in Men
The same type of high-intensity light therapy used to treat seasonal affective disorder (SAD) and as an adjunctive treatment for non-seasonal depression has been found to boost testosterone and improve sexual satisfaction in men with low libido.
In a study by Andrea Fagiolini and colleagues, men with low sexual desire or trouble getting aroused were exposed to the high intensity light (10,000 Lux) for a half hour upon waking. Compared to men who used a lightbox that filtered the light to only 100 Lux, men exposed to the high-intensity light for two weeks showed increased testosterone in the blood and reported greater sexual satisfaction. Testosterone levels increased from around 2.1 ng/ml to 3.6 ng/ml in the high-intensity light group. (There were no significant changes in the comparison group.) Light therapy is quite safe for people without eye problems.
Fagiolini explained that in the Northern hemisphere, testosterone production declines from November to April and then rises again through the spring and summer, peaking in October. He suggests that the light therapy mimics the effect of summer light on the body, perhaps by inhibiting the pineal gland, which secretes hormones.
Fagiolini and colleagues hope to replicate the study with a greater number of participants and to determine how long the results may last.The study of 38 participants was presented at the 29th Congress of the European College of Neuropsychopharmacology in 2016.
Psilocybin May Improve Treatment-Resistant Depression
A small, uncontrolled study in the journal Lancet Psychiatry suggests that psilocybin, an ingredient in hallucinogenic mushrooms, relieved depression symptoms for up to three months in seven of 12 participants with unipolar depression that had not responded to at least two antidepressant medications.
Psilocybin has a different mechanism of action than typical treatments for depression. It activates 5HT2A serotonin receptors.
The participants, who had moderate to severe depression, were given two oral doses of psilocybin, a low dose (10mg) to establish the safety of the intervention, and a higher dose (25mg) seven days later. Psychedelic effects (anxiety, confusion, nausea, and headache) peaked within two to three hours and had dissipated by six hours after the intervention.
Depression began to improve within 24 hours after the 25mg dose. Depression symptoms were significantly improved by one week after the intervention. Eight of the 12 participants had a complete remission of their depression after one week, and this lasted the full three months in five participants. By the end of the three months, a total of seven of the 12 participants met the criteria for response to psilocybin.
The study’s authors, led by Robin L. Carhart-Harris, suggest that their preliminary results warrant more systematic investigation of psilocybin, but because there was no comparison group in this study, a large placebo effect cannot be ruled out.
Mindfulness-Based Cognitive Therapy May Improve Depression More Than Fitness Intervention
In a study by researcher Stuart Eisendrath and colleagues, people with treatment-resistant unipolar depression responded better to an intervention that combined mindfulness training with cognitive therapy than to one that included exercise, nutrition counseling, and music therapy.
The 173 participants had failed to respond to at least two different antidepressant medications. During the study period, all participants were taking an antidepressant, but none were receiving other types of therapy.
After eight weeks, the mindfulness-based cognitive therapy (MBCT) group showed greater improvement in their depression symptoms than the exercise and nutrition group. Of the MBCT group, 29.58% had a large reduction in symptoms, while 17.19% of the comparison group showed a similarly large reduction in symptoms.
A subgroup of the participants also received functional magnetic resonance imaging (fMRI) as part of the study. While completing a task related to emotional working memory, the MBCT group showed enhanced activation of the dorsal lateral prefrontal cortex (to levels seen in non-depressed people). This area is related to executive control of depression and memory functions. The MBCT group also showed reduced activation of the ventral lateral prefrontal cortex compared to the comparison group. Members of the MBCT whose depression symptoms had improved also showed better regulation of the amygdala during the task compared to the exercise and nutrition group.
The research was presented at the 2016 meeting of the American Psychiatric Association.
Combination of SSRIs and Statins Better than SSRIs Alone
A large study in Denmark suggests that taking selective serotonin reuptake inhibitor (SSRI) antidepressants alongside cholesterol-lowering statin drugs improved depression more than SSRIs alone. The findings, by Ole Köhler and colleagues were reported in the American Journal of Psychiatry in 2016.
The study included 872,216 people in Denmark’s national health care database who took SSRIs between 1997 and 2012. The most common SSRIs were citalopram, sertraline, and escitalopram. Of these people taking SSRIs, 13.0% also took a statin drug, typically simvastatin. Those patients who were taking both an SSRI and a statin were less likely than those taking an SSRI alone to be hospitalized for any psychiatric problem, or for depression specifically.
Depression is known to be correlated with inflammation throughout the body. Statins reduce this inflammation as well as lowering cholesterol. A 2013 study by Ahmad Ghanizadeh and Arvin Hedayati in the journal Depression and Anxiety showed that the SSRI fluoxetine and the statin lovastatin reduced depression severity compared to fluoxetine alone.
The combination of SSRIs and statins did not seem to reduce deaths or suicidal behavior compared to SSRIs alone. Statins have some side effects, but combining them with antidepressants did not increase the risks associated with their use.
SSRI Use During Pregnancy Linked to Adolescent Depression in Offspring
A 2016 article by Heli Malm and colleagues in the Journal of the American Academy of Child and Adolescent Psychiatry suggests that in utero exposure to selective serotonin reuptake inhibitor (SSRI) antidepressants may increase the risk of depression in adolescence. However, the study included potentially confounding factors. It is possible that women who took SSRIs during pregnancy had more severe depression than those who went unmedicated during pregnancy. The mothers in the study who took SSRIs also had more comorbid conditions such as substance abuse.
Editor’s Note: Women should balance the risks and benefits of antidepressant use during pregnancy, since depression itself can have adverse effects on both mother and fetus. It has recently been established that SSRI use during pregnancy does not cause birth defects, so women with depression that has not responded to non-pharmaceutical interventions such as psychotherapy, omega-3 fatty acid supplementation, exercise, mindfulness, and repeated transcranial magnetic stimulation (rTMS) may still want to consider SSRIs.