6 Minutes of Intense Cycling Produces Major Increases in BDNF
Brain derived neurotrophic factor (BDNF) is necessary for new synapses and call survival. A new study in J. Physiology (2023) reports that the increases in BDNF from short intense cycling exercise are much greater than from prolonged (90-minute) light cycling. The authors think that this is cause by the increases in lactate produced which helps up regulate BDNF production. This could be good for fighting depression and Alzheimer’s disease, where BDNF levels are low.
Bottom line: If you don’t have much time, bust your buns.
U.S. FDA Approves VRAYLAR® (cariprazine) as an Adjunctive Treatment for Major Depressive Disorder
“A Phase 3 Study 3111-301-001 showed a clinically and statistically significant change from baseline to week six in the Montgomery-Åsberg Depression Rating Scale (MADRS) total score for patients treated with cariprazine at 1.5 mg/day + ADT compared with placebo + ADT. A second registration-enabling study, RGH-MD-75, showed a clinically and statistically significant change from baseline to week eight in the MADRS total score for patients treated with cariprazine at 2-4.5 mg/day (mean dose 2.6 mg) + ADT compared with placebo + ADT.
Cariprazine was generally well tolerated in 6- and 8-week studies. Mean weight change was < 2lbs and ? 3% of patients had a weight increase of ? 7%.
The starting dosage of VRAYLAR is 1.5 mg once daily. Depending upon clinical response and tolerability, the dosage can be increased to 3 mg once daily on Day 15. In clinical trials, dosage titration at intervals of less than 14 days resulted in a higher incidence of adverse reactions. The maximum recommended dosage is 3 mg once daily.
Most common adverse reactions observed in the adjunctive MDD studies (? 5% and at least twice the rate of placebo) were:
Akathisia, nausea, and insomnia at the recommended doses in 6-week, fixed-dose trials
Akathisia, restlessness, fatigue, constipation, nausea, increased appetite, dizziness, insomnia, and extrapyramidal symptoms in one 8-week flexible-dose trial at a titration of less than 14 days”
Intermittent theta burst magnetic stimulation (iTBS) is FDA approved.
As reported in Psych. News:?The Food and Drug Administration (FDA) has cleared the SAINT Neuromodulation System for the treatment of refractory depression in adults, Magnus Medical Inc. (the manufacturer of the product)?announced?Tuesday. SAINT is a?modified form of transcranial magnetic stimulation?(TMS) that compresses weeks of conventional TMS therapy into just five days”. ?Regular TMS takes 20-30 minutes per daily session while iTBS takes about 5 minutes and thus can be applied many times in a single day. ?”As demonstrated in a clinical trial?published?in?The American Journal of Psychiatry, Montgomery-Åsberg Depression Rating Scale (MADRS) scores dropped by 62% among participants following five days of SAINT stimulation compared with a 14% drop among participants receiving sham stimulation. These improvements were sustained over a four-week follow-up.” ?The method was developed by Nolan Williams and he used MRI to best target the site of stimulation
Cannabidiol (CBD) does not make cannabis safer
Amir Englund et al reported in Neuropsychopharmacology in A randomised, double-blind, cross-over trial of cannabis with four different CBD:THC ratios that CBD did not protect against the adverse effect of THC. These included impaired delayed verbal recall ( p?=?0.001) and induced positive psychotic symptoms on the PANSS ( p?=?2.41?×?10–5).
Editors Note: Not only does marijuana impair memory, it is a risk factor the onset of bipolar disorder and schizophrenia. When pot is used by a person with a unipolar or bipolar mood disorder, there are increases in depression and anxiety and an overall less favorable course of illness. If a person with a mood disorder uses heavy amounts of marijuana, they could consider buying N-acetylcysteine (NAC) 500mg and increasing the dose to 1,000mg twice a day within a week as this has been shown to decrease drug use compared to placebo in adolescents and young adults using and abusing pot. Most people who sell pot, are not well-informed about its dangers and just want to make money.
Cariprazine Effective in AD-Resistant MDD
Maletic, V, et al. reported on Efficacy of Adjunctive Cariprazine Across Individual Depressive Symptoms in Major Depressive Disorder: A Post-Hoc Analysis. Poster presented at Psych Congress 2022; September 17-20, 2022.
“With 751 patients (502 on CARIPRAZINE (CAR) and 249 on PBO), the LSMD (95% CI) score change from baseline to week 6 was significant in favor of CAR. Items of the MADRS scale were assessed individually over the course of the study, including apparent sadness, reported sadness, reduced appetite, lassitude, inability to feel, pessimistic thoughts, and suicidal thoughts, showing improvement compared to PBO. “
First and Only Oral NDMA Receptor Antagonist for MDD Can Now Be Prescribed
| October 28, 2022 |
| FEATURED NEWS: First and Only Oral NDMA Receptor Antagonist for MDD Can Now Be Prescribed Extended-release dextromethorphan HBr-bupropion HCl (Auvelity™), the only oral N-methyl D-aspartate (NMDA) receptor antagonist approved for the treatment of major depressive disorder (MDD), is now available by prescription in the United States, maker Axsome Therapeutics Inc. announced. The drug is supplied in 105-mg tablets in 30-count bottles.On August 18th, 2022, the US Food and Drug Administration (FDA) approved dextromethorphan HBr-bupropion HCl extended-release tablets 45mg/105mg |
Psilocybin Comparable to Escitalopram in the Treatment of Depression

Four randomized, controlled clinical trials have established that psilocybin, the hallucinogenic compound in “magic mushrooms,” has anti-depressant effects. Recently, a phase 2 clinical trial compared the effects of psilocybin to a US Food and Drug Administration (FDA)–approved treatment for depression, the selective serotonin-reuptake inhibitor (SSRI) escitalopram. The study by Robin Carhart-Harris and colleagues was published in the New England Journal of Medicine in 2021.
The 59 participants in the 6-week study, which took place in the United Kingdom, had longstanding moderate-to-severe major depressive disorder. They were randomized to two groups. The psilocybin group received two separate doses of 25 mg of psilocybin 3 weeks apart, plus 6 weeks of daily placebo. The escitalopram group received two separate doses of 1 mg of psilocybin 3 weeks apart plus 6 weeks of daily oral escitalopram. (The small doses of psilocybin administered to the escitalopram group were assumed to have negligible psychiatric effects.) All participants were told they would receive psilocybin (though not the dose) in order to standardize their expectations.
In addition to the drug treatments, all participants also received psychological support, which consisted of monitoring immediately after the administration of the drugs (given the expectation that the 25mg dose of psilocybin would produce an “altered quality of conscious experience”), psychological debriefings, and an active listening session.
Psilocybin improved depression symptoms to a greater extent than escitalopram did. Among the participants, 70% of the psilocybin group responded to the treatment, compared with 48% of the escitalopram group. Remission occurred in 57% of the psilocybin group compared with 28% of the escitalopram group. These differences in the outcomes for the two groups were not statistically significant.
The FDA has designated psilocybin a “Breakthrough Therapy” for severe depression, which indicates that the therapy may be a substantial improvement over existing therapies for a serious condition. The designation is intended to speed up the drug development and review process.
The state of Oregon legalized psilocybin-assisted therapy in 2020.
Transcranial Direct Current Stimulation (tDCS) Induces Gray-Matter Increases in Depression
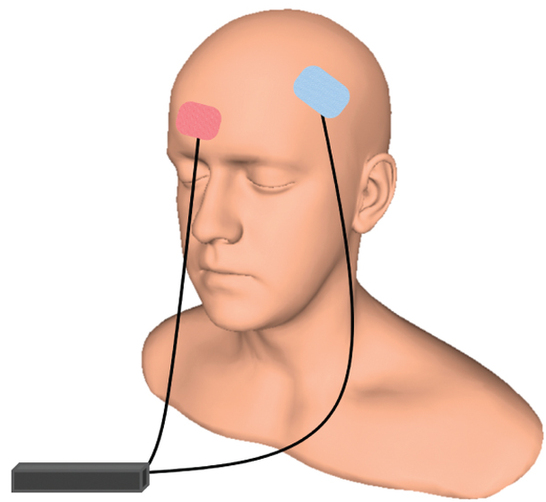
At the 2021 meeting of the Society of Biological Psychiatry (SOBP), researcher Mayank Jog and colleagues described a study of transcranial direct current stimulation (tDCS) in 59 patients with moderate depression. The patients received either tDCS sessions that delivered electrical current at 2mA for 20 minutes or a same-length sham stimulation delivered using a double-blind stimulator, for a total of 12 sessions over 12 consecutive working days. Jog and colleagues found that compared to the sham stimulation, tDCS induced increases in gray matter volume in the left dorsolateral prefrontal cortex (DLPFC) target area, with a statistically large effect size (Cohen’s d = 1.3). The researchers plan to follow up this study that found structural changes to the brain after tDCS with more research on the antidepressant effects of the treatment.
Good Outcomes Among Patients with Major Depressive Disorder Treated with Transcranial Magnetic Stimulation in a Large Study

At the 2021 meeting of the Society of Biological Psychiatry (SOBP), researcher Harold Sackeim and colleagues reported on data collected from patients in clinical treatment for major depression who received transcranial magnetic stimulation (TMS) at 103 practice sites. A total of 5,010 depressed patients were included in the intent-to-treat sample, and 3,814 completed the study, meaning that they either reached remission or were treated at least 20 times and went through a final assessment. “Response (58–83%) and remission (28–62%) rates were notably high across self-report and clinician-administered assessments,” and women had better outcomes than men. Sackeim and colleagues concluded, “Strong efficacy and the low side effect and medical risk profile suggest that TMS be evaluated as a first-line treatment for [major depressive disorder].”
Accelerated Intermittent Theta-Burst Stimulation (aiTBS) Quickly Improved Treatment-Resistant Depression

At the 2021 meeting of the Society of Biological Psychiatry (SOBP), researcher Nolan Williams and colleagues described a sham-controlled trial of accelerated intermittent theta-burst stimulation (aiTBS) in patients with treatment-resistant depression. Theta burst stimulation is a specific protocol for rTMS, or repeated transcranial magnetic stimulation, a non-invasive form of brain stimulation. Magnets placed on a patient’s head provide bursts of high-frequency stimulation to the brain.
Participants in the study received 50 sessions over 5 days of either aiTBS or a sham procedure. Among those who received the real aiTBS treatment, 85.7% saw an improvement in their treatment-resistant depression, compared to only 26.7% of those in the sham group. AiTBS produced a rapid antidepressant response, which Williams and colleagues suggest could be useful for the treatment of patients in emergency rooms or inpatient settings.

