Children at Risk for Bipolar Disorder May Have Adverse Reactions to Antidepressants
 At the 2015 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Jeffrey R. Strawn reported that among children at high risk for bipolar disorder (because of a family history of the disorder) who are prescribed antidepressants for depression and anxiety, adverse reactions are common. These reactions include irritability, aggression, impulsivity, and hyperactivity, and often lead to discontinuation of the antidepressant treatment.
At the 2015 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Jeffrey R. Strawn reported that among children at high risk for bipolar disorder (because of a family history of the disorder) who are prescribed antidepressants for depression and anxiety, adverse reactions are common. These reactions include irritability, aggression, impulsivity, and hyperactivity, and often lead to discontinuation of the antidepressant treatment.
Younger patients at risk for bipolar disorder were more likely to have an adverse reaction to antidepressants. Risk of an adverse reaction decreased 27% with each year of age.
Offspring of Bipolar Parents at High Risk for Psychiatric Disorders
Researcher Juan David Palacio reported at the 2015 meeting of the American Academy of Child and Adolescent Psychiatry that compared to offspring of non-ill parents, children of parents with bipolar I disorder are at high risk for psychiatric disorders, particularly bipolar spectrum disorders and substance use disorders. They were also at risk for symptoms of anxiety disorders and conduct disorder. Palacio’s findings from Colombia mirror those from other studies of familial risk and suggest the importance of vigilance to detect these disorders early and provide appropriate treatment. Our Child Network may help.
Facial Emotion Recognition Deficient in Bipolar Disorder
In the past decade, several studies have indicated that people with bipolar disorder have less ability to recognize the emotions expressed on people’s faces than do healthy controls. A 2013 meta-analysis by Cecilia Samamé and colleagues concluded that facial emotion recognition was deficient in people with bipolar disorder regardless of their current state. A 2011 quantitative review article by Christian G. Kohler and colleagues revealed that this difficulty distinguishing emotions is general, rather than specific to any one emotion.
A 2015 study by Esther Vierck and colleagues in the journal Psychiatry Research showed that both euthymic patients with bipolar disorder and their first-degree relatives without bipolar disorder performed worse on tests of emotion recognition than did normal controls. The findings in healthy relatives suggest that the deficit may be a familial risk factor for the development of bipolar disorder.
These deficits in facial emotion recognition have also been seen in 4 out of 5 studies of children with early-onset bipolar disorder, including those who are euthymic. 2008 studies by Melissa A. Brotman and colleagues showed that even children just at high risk for bipolar disorder due to a family history of the disorder had deficient emotion recognition.
This literature indicates that deficiencies in facial emotion recognition consistently accompany bipolar disorder and may also be a sign that a child or teenager is at risk for bipolar disorder. Since these deficits can create social and interpersonal difficulties, it may be useful to teach better emotion recognition skills to people with bipolar disorder or those at high risk for the illness.
Reduced Cognitive Function and Other Abnormalities in Pediatric Bipolar Disorder
 At the 2015 meeting of the International Society for Bipolar Disorders, Ben Goldstein described a study of cognitive dysfunction in pediatric bipolar disorder. Children with bipolar disorder were three years behind in executive functioning (which covers abilities such as planning and problem-solving) and verbal memory.
At the 2015 meeting of the International Society for Bipolar Disorders, Ben Goldstein described a study of cognitive dysfunction in pediatric bipolar disorder. Children with bipolar disorder were three years behind in executive functioning (which covers abilities such as planning and problem-solving) and verbal memory.
There were other abnormalities. Youth with bipolar disorder had smaller amygdalas, and those with larger amygdalas recovered better. Perception of facial emotion was another area of weakness for children (and adults) with bipolar disorder. Studies show increased activity of the amygdala during facial emotion recognition tasks.
Goldstein reported that nine studies show that youth with bipolar disorder have reduced white matter integrity. This has also been observed in their relatives without bipolar disorder, suggesting that it is a sign of vulnerability to bipolar illness. This could identify children who could benefit from preemptive treatment because they are at high risk for developing bipolar disorder due to a family history of the illness.
There are some indications of increased inflammation in pediatric bipolar disorder. CRP, a protein that is a marker of inflammation, is elevated to a level equivalent to those in kids with juvenile rheumatoid arthritis before treatment (about 3 mg/L). CRP levels may be able to predict onset of depression or mania in those with minor symptoms, and is also associated with depression duration and severity. Goldstein reported that TNF-alpha, another inflammatory marker, may be elevated in children with psychosis.
Goldstein noted a study by Ghanshyam Pandey that showed that improvement in pediatric bipolar disorder was related to increases in BDNF, a protein that protects neurons. Cognitive flexibility interacted with CRP and BDNF—those with low BDNF had more cognitive impairment as their CRP increased than did those with high BDNF.
Offspring of Parents with Psychiatric Disorders At Increased Risk for Disorders of Their Own
At a symposium at the 2015 meeting of the International Society for Bipolar Disorder, researcher Rudolph Uher discussed FORBOW, his study of families at high risk for mood disorders. Offspring of parents with bipolar disorder and severe depression are at higher risk for a variety of illnesses than offspring of healthy parents.
Uher’s data came from a 2014 meta-analysis by Daniel Rasic and colleagues (including Uher) that was published in the journal Schizophrenia Bulletin. The article described the risks of developing mental illnesses for 3,863 offspring of parents with schizophrenia, bipolar disorder, or major depression compared to offspring of parents without such disorders.
Previous literature had indicated that offspring of parents with severe mental illness had a 1-in-10 likelihood of developing a severe mental illness of their own by adulthood. Rasic and colleagues suggested that the risk may actually be higher—1-in-3 for the risk of developing a psychotic or major mood disorder, and 1-in-2 for the risk of developing any mental disorder. An adult child may end up being diagnosed with a different illness than his or her parents.
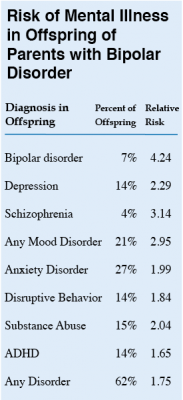 At the symposium, Uher focused on families in which a parent had bipolar disorder. These families made up 1,492 of the offspring in the Rasic study. The table at right shows the risk of an illness among the offspring of bipolar parents compared to that risk among offspring of healthy parents, otherwise known as relative risk. (For example, offspring of parents with bipolar disorder are 4.24 times more likely to be diagnosed with bipolar disorder themselves than are offspring of non-bipolar parents.) The table also shows the percentage of offspring of parents with bipolar disorder who have each type of disorder.
At the symposium, Uher focused on families in which a parent had bipolar disorder. These families made up 1,492 of the offspring in the Rasic study. The table at right shows the risk of an illness among the offspring of bipolar parents compared to that risk among offspring of healthy parents, otherwise known as relative risk. (For example, offspring of parents with bipolar disorder are 4.24 times more likely to be diagnosed with bipolar disorder themselves than are offspring of non-bipolar parents.) The table also shows the percentage of offspring of parents with bipolar disorder who have each type of disorder.
Editor’s Note: These data emphasize the importance of vigilance for problems in children who are at increased risk for mental disorders because they have a family history of mental disorders. One way for parents to better track mood and behavioral symptoms is to join our Child Network.
Predictors of Bipolar Disorder in At-Risk Youth
A new longitudinal study of 391 youth at risk for bipolar disorder revealed some predictors of the disorder. The study by Danella M. Hafeman and colleagues was presented at the 2015 meeting of the Society of Biological Psychiatry. The participants were aged 6–18 and each had a parent with bipolar disorder. Over the course of the study, 40 developed an illness on the bipolar spectrum, including 21 who developed bipolar I or II. The participants were assessed for various descriptive characteristics and those who developed bipolar disorder were compared to those who developed major depressive disorder.
The most important predictors of bipolar disorder were parental assessment of internalizing symptoms of anxiety or depression, self-assessment of mood changeability, and self-assessment of hostility. A diagnosis of bipolar disorder not otherwise specified (BP-NOS) was the only predictor of a later diagnosis of bipolar I or II.
Editors Note: These data resemble findings from a 2015 study by David Axelson and colleagues in the American Journal of Psychiatry that used the same cohort of participants. The Axelson study indicated that a categorical diagnosis of a major psychiatric disorder occurred in 74% of the offspring of a bipolar parent compared to about 50% in a control group from the community. Depression, anxiety, attention deficit hyperactivity disorder (ADHD), and oppositional disorders were even more common than bipolar disorder in the at-risk population.
The presence of a major psychiatric diagnosis in about three-quarters of the offspring of a parent with bipolar disorder suggests the importance of early vigilance. One way to track symptoms of depression, anxiety, ADHD, oppositional behavior, and bipolar disorder is to join the Child Network, a secure online platform for rating children’s moods, medications, and side effects. These weekly ratings can be collected longitudinally and printed out to help parents and clinicians assess mood difficulties in their children.
Subthreshold Episodes of Mania Best Predictor of Bipolar Disorder in Children
Relatively little attention has been paid to the children of a parent with bipolar disorder, who are at risk not only for the onset of bipolar disorder, but also anxiety, depression, and multiple other disorders. These children deserve a special focus, as on average 74.2% will receive a major (Axis 1) psychiatric diagnosis within seven years.
New research published by David Axelson and colleagues in the American Journal of Psychiatry describes a longitudinal study comparing children who have a parent with bipolar disorder to demographically matched children in the general public. Offspring at high risk for bipolar disorder because they have a parent with the disorder had significantly higher rates of subthreshold mania or hypomania (13.3% versus 1.2%) or what is known as bipolar disorder not otherwise specified (BP-NOS); manic, mixed, or hypomanic episodes (9.2% versus 0.8%); major depressive episodes (32.0% versus 14.9%); and anxiety disorders (39.9% versus 21.8%) than offspring of parents without bipolar disorder. Subthreshold episodes of mania or hypomania (those that resemble but do not meet the full requirements for bipolar disorder in terms of duration) were the best predictor of later manic episodes. This finding was observed prospectively, meaning that patients who were diagnosed with manic episodes during a follow-up assessment were likely to have been diagnosed with a subthreshold manic or hypomanic episode during a previous assessment.
The study included 391 children (aged 6–18) of at least one bipolar parent, and compared these to 248 children of parents without bipolar disorder in the community. The participants took part in follow-up assessments every 2.5 years on average, for a total of about 6.8 years. Each follow-up assessment included retrospective analysis of symptoms that had occurred since the previous assessment.
In addition to having more subthreshold manic or hypomanic episodes; manic, mixed, or hypomanic episodes; and major depressive episodes, the high-risk children also showed more non-mood-related axis 1 disorders, including attention deficit hyperactivity disorder (ADHD), disruptive behavior disorders, and anxiety disorders than the children of parents without bipolar disorder. Axelson suggested that monitoring for these symptoms may help with early identification and treatment.
Children with a bipolar parent were diagnosed with bipolar spectrum disorders at rates of 23% compared to 3.2% in the comparison offspring. Mean age of onset of mania or hypomania in the high-risk offspring was 13.4 years. Of those offspring who had a manic episode, more than half had the episode before age 12, with the earliest occurring at age 8.1.
Compared to previous studies of children of parents with bipolar disorder, this study found that the mean age of onset of manic or hypomanic episodes was younger, possibly because other studies did not include young children. Another new finding was that major depressive episodes were risk factors for mania and hypomania but did not always precede the onset of mania or hypomania in the high-risk offspring.
Parents of children who are at high risk for developing bipolar spectrum disorders should be aware of the common precursors to mania—subthreshold manic or hypomanic symptoms and non-mood disorders—and make sure that clinicians assess for these symptoms and differentiate them from the symptoms of depression or other disorders.
Editor’s Note: In Axelson’s study, 74.2% of the offspring of a bipolar parent suffered a major (Axis I) psychiatric disorder. However, 48.4% of the offspring from the comparison group of community controls also had an Axis 1 psychiatric disorder. These high rates of illness and dysfunction indicate the importance of monitoring a variety of symptom areas and getting appropriate evaluation and treatment in the face of symptoms that are associated with impairment in both high risk children and in the general population.
One way of doing this is for parents to join our new Child Network, a study collecting information about how children at risk for bipolar disorder or with symptoms of bipolar disorder are being treated in the community and how well they are doing. Parents rate their children on a weekly basis for depression, anxiety, ADHD, oppositionality, and mania-like symptoms. Parents will be able to produce a longitudinal chart of their children’s symptoms and response to treatment, which may assist their child’s physician with early detection of illness and with treatment. See here for more information and to access informed consent documents.
ADHD and Bipolar Disorder Are Inherited Separately
While attention-deficit hyperactivity disorder (ADHD) is fairly common among people with bipolar disorder, the genetic risks of inheriting these two illnesses run separately in families. In a recent study of 465 people and 563 of their first-degree relatives by Susan Shur-Fen Gau and colleagues, people with bipolar I disorder were likely to have relatives with bipolar I disorder, and people with ADHD were likely to have relatives with ADHD, but ADHD did not increase risk of bipolar disorder and vice versa.
The researchers hypothesize that other reasons people might develop both disorders include developmental precursors to the illnesses, neurocognitive functioning, sleep problems, and personality traits such as impulsivity and disinhibition.
Editor’s Note: At a recent scientific meeting, Gau and her colleague Kathleen Merikangas said that people with bipolar disorder in the study were five times more likely to have relatives with bipolar disorder. Bipolar disorder and ADHD were comorbid in 37.8% of those with bipolar I disorder, 16.4% in bipolar II disorder, 14% in depression, and 1.1% in normal controls.
A Symposium on High Risk Studies: Offspring of Parents with Bipolar Disorder
In a symposium at the 2014 meeting of the International College of Neuropsychopharmacology, four researchers shared insights on children who are at higher risk for bipolar disorder because they have a parent with the disorder.
Researcher John Nurnberger has been studying 350 children of parents with bipolar disorder in the US and 141 control children of parents with no major psychiatric disorder, following the participants into adolescence. He found a major affective disorder in 23.4% of the children with parents who have bipolar disorder and 4.4% of the controls. Of the at-risk children, 8.5% had a bipolar diagnosis versus 0% of the controls.
Nurnberger found that disruptive behavior disorders preceded the onset of mood disorders, as did anxiety disorders. These diagnoses predicted the later onset of bipolar disorder in the at-risk children, but not in the controls. A mood disorder in early adolescence predicted a substance abuse disorder later in adolescence among those at risk.
In genome-wide association studies, the genes CACNA1C and ODZ4 are consistently associated with risk of bipolar disorder, but with a very small effect size. Therefore, Nurnberger used 33 different gene variants to generate a total risk score and found that this measure was modestly effective in identifying relative risk of developing bipolar disorder. He hopes that using this improved risk calculation along with family history and clinical variables will allow better prediction of the risk of bipolar onset in the near future.
Researcher Ann Duffy reported on her Canadian studies of children who have a parent with bipolar disorder and thus are at high risk for developing the disorder. In contrast to the studies of Nurnberger et al. and many others in American patients, she found almost no childhood onset of bipolar disorder before late adolescence or early adulthood. She found that anxiety disorders emerge first, followed by depression, and then only much later bipolar disorder. Bipolar disorder occurred with comorbid substance abuse disorders in only about 10-20% of cases in 1975, but substance abuse increased to 50% of bipolar cases in 2005. The incidence of comorbid substance disorder and the year at observation correlated strongly, indicating a trend toward increased substance abuse over the 30-year period.
Duffy found that having parents who were ill as opposed to recovered was associated with a more rapid onset of mood disorder in the offspring, usually in early adulthood. Duffy emphasized the need to intervene earlier in children of parents with bipolar disorder, but this is rarely done in clinical practice. Read more
Korean Study of Mental Disorders in Children of Bipolar Parents
Korea, like the US, has a moderate incidence of childhood-onset bipolar disorder among children who are at high risk because they have a parent with bipolar disorder. In a recent study by Young-Sun Cho et al. presented at the 2014 meeting of the International College of Neuropsychopharmacology (CINP), 59 out of 100 children with a parent who had been diagnosed with bipolar disorder met the criteria for a mental disorder themselves.
Mood disorders were most common. Of the 59 children with mental disorders, 22 were diagnosed with bipolar disorder, and 16 were diagnosed with a depressive disorder. Others included four with attention deficit hyperactivity disorder (ADHD), four with an anxiety disorder, two with disruptive behavior disorders, one with a tic disorder, one with an autistic disorder, and one with schizophrenia and an anxiety disorder.
Editor’s Note: In contrast to studies in Germany, Switzerland, the Netherlands, and Canada, where few children are diagnosed with bipolar disorders (even among those who are at high risk because of a family history of bipolar disorder), 22% of high-risk children in Korea were diagnosed with bipolar disorder. This is comparable to or higher than rates at which high-risk children in the US are diagnosed with bipolar disorder. Studies from both the Bipolar Collaborative Network (in which this editor Robert Post is an investigator) and researcher Boris Birmaher et al. found that parents with bipolar disorder often had a variety of other disorders, such as anxiety, alcohol abuse, or substance abuse. These other illnesses also increase the risk of early-onset bipolar disorder in offspring, and this may account for the higher incidence of early-onset bipolar disorder among high-risk children in the US.