Acetly-l-carnitine May Be Effective in Treatment-Resistant Depression
 Not all patients with unipolar depression respond to the currently available antidepressants. Acetyl-l-carnitine is a compound that enhances mitochondrial function and neuroplasticity and is effective in the treatment of peripheral neuropathy (damage to the peripheral nerves, which sometimes occurs in chemotherapy or diabetes). It is now being investigated as an antidepressant for patients who have not responded to typical antidepressants.
Not all patients with unipolar depression respond to the currently available antidepressants. Acetyl-l-carnitine is a compound that enhances mitochondrial function and neuroplasticity and is effective in the treatment of peripheral neuropathy (damage to the peripheral nerves, which sometimes occurs in chemotherapy or diabetes). It is now being investigated as an antidepressant for patients who have not responded to typical antidepressants.
According to a review of the treatment by S.M. Wang et al. published in the Journal of Psychiatric Research in 2014, acetyl-l-carnitine treated depression better than placebo did in four randomized clinical studies. It was better than placebo and equally as effective as the antidepressant fluoxetine and the atypical antipsychotic amisulpride in various studies of dysthymic disorder. It also improved depressive symptoms in people with fibromyalgia and minimal hepatic encephalopathy (liver damage). The usual dose of acetyl-l-carnitine is 1 to 2 grams/day.
Editor’s Note: The role acetyl-l-carnitine will play in treating people with treatment-resistant unipolar or bipolar depression remains to be better clarified.
The Nucleus Accumbens in Depression
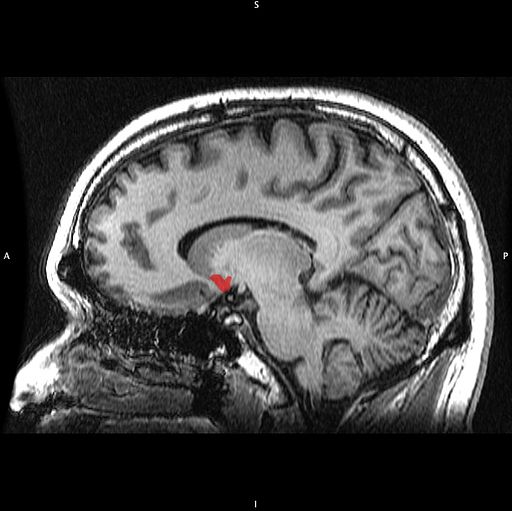
Brain-derived neurotrophic factor (BDNF) keeps neurons healthy and is critical for long-term memory and synapse formation. BDNF levels increase in the nucleus accumbens (the brain’s reward center) and decrease in the hippocampus during clinical depression and chronic cocaine use. In rodents, the same changes in BDNF levels occur during defeat stress (which resembles human depression).
Rodents who are repeatedly defeated by a larger rodent exhibit behaviors such as social withdrawal, lethargy, and decreased interest in sucrose. The increases in BDNF in the nucleus accumbens of these rodents could reflect the learning that takes place during the repeated defeat stress and the depression-like behaviors that follow it. Blocking the BDNF increases in the nucleus accumbens prevents these behaviors from developing.
Chadi Abdallah and other researchers at Yale University recently found that the left nucleus accumbens of patients with treatment-resistant depression is enlarged compared to normal controls, and the drug ketamine, which produces rapid-onset antidepressant effects, rapidly decreases the volume of the nucleus accumbens in the depressed patients. The mechanism by which it does so is unknown, but could reflect some suppression of the depressive learning.
Any relationship between the volume of the nucleus accumbens and its levels of BDNF is unknown, but ketamine’s effect on the size of this brain region could be linked to a decrease in the defeat-stress memories.
Rationale for Using Ketamine in Youth with Treatment-Resistant Depression
At the 2013 meeting of the American Academy of Child and Adolescent Psychiatry, Vilma Gabbay of the Mount Sinai School of Medicine reiterated the findings from the TORDIA (Treatment of SSRI-Resistant Depression in Adolescents) study that 20% of young people with depression remained resistant to treatment, childhood-onset depression was more likely to be recurrent and more difficult than adult-onset depression in the long run, and suicide was the second leading cause of death in 12- to 17-year-olds in 2010 according to a Centers for Disease Control report in May 2013. Anhedonia (a loss of pleasure in activities once enjoyed) was the most difficult symptom to treat in adolescents.
Gabbay carefully explained some of the rationales for using ketamine in young people with depression. The presence of inflammation is a poor prognosis factor, and ketamine has anti-inflammatory effects, decreasing levels of inflammatory markers CRP, TNF-alpha, and Il-6.Given that ketamine has been widely used as an anesthetic for surgical procedures, its safety in children has already been demonstrated. Ketamine did not appear to cause behavioral sensitization (that is, increased effect upon repetition) in a report by Cho et al. in 2005 that included 295 patients.
As noted previously, Papolos et al. reported in a 2012 article in the Journal of Affective Disorders that intranasal ketamine at doses of 50 to 120 mg was well-tolerated and had positive clinical effects in 6- to 19-year-olds with the fear of harm subtype of bipolar disorder that had been highly resistant to treatment with more conventional drugs.
Gabbay reluctantly endorsed further cautious controlled trials in children and adolescents, in light of ketamine’s suggested efficacy and good safety profile, which stands in contrast to its popular reputation as a party drug or “Special K.”
Editor’s Note: The discussant of the symposium, Neal Ryan of Western Psychiatric Institute and Clinic, added an exquisitely brief discussion suggesting that ketamine should ultimately be studied in combination with behavioral and psychotherapeutic procedures to see if its therapeutic effects could be enhanced. He made this suggestion based on the data that ketamine has important synaptic effects, increasing brain-derived neurotrophic factor (BDNF), which is important for healthy cells and long-term memory, and reverting thin dendritic spines caused by stress back to their normal mushroom shape. This editor (Robert Post) could not be more in agreement.
Intranasal Ketamine May Be an Alternative to IV in Refractory Depression
At the 2013 meeting of the American Academy of Child and Adolescent Psychiatry, Kyle Lapidus of Mount Sinai Hospital reviewed the literature from controlled studies on the efficacy of intravenous (IV) ketamine at a dosage of 0.5 mg/kg over a 40-minute infusion for adults with treatment-resistant depression (with consistent response rates of 50% or more), and suggested that intranasal ketamine may also be effective.
Ketamine is a strong blocker of the glutamate NMDA receptor. At high doses (6 to 12 mg/kg) it is an anesthetic, at slightly lower doses (3 to 4 mg/kg) it is psychotomimetic (causing psychotic symptoms) and is sometimes used as a drug of abuse, and at very low doses it is a rapidly acting antidepressant, often bringing about results within 2 hours. Antidepressant effects typically last 3 to 5 days, so the question of how to sustain these effects is a major one for the field.
Murrough et al. reported in Biological Psychiatry in 2012 that five subsequent infusions of ketamine sustained the initial antidepressant response and appeared to be well tolerated by the patients. Another NMDA antagonist, riluzole (used for the treatment of ALS or Lou Gehrig’s disease), did not sustain the acute effects of ketamine, and now lithium is being studied as a possible strategy for doing so.
The bioavailability of ketamine in the body depends on the way it is administered. Compared to IV administration, intramuscular (IM) administration is painful but results in 93% of the bioavailability of IV ketamine. Intranasal (IN) administration results in 25-50% of the bioavailability of IV administration, while oral administration results in only 16-20% of the bioavailability of IV administration, so Lapidus chose to study the IN route. He compared intranasal ketamine at doses of 50mg (administered in a mist ) to 0.5 ml of intranasal saline. Both were given in two infusions seven days apart. Lapidus observed good antidepressant effects and good tolerability. Papolos et al. had reported earlier that intranasal ketamine had good effects in a small open trial in treatment-resistant childhood onset bipolar disorder.
Editor’s Note: Further studies of the efficacy and tolerability of intranasal ketamine are eagerly awaited.
Acquired Lithium Resistance
Lithium is one of the most important treatments available for bipolar disorder. A small percentage of patients who initially respond well to lithium may develop resistance to the drug over time. Some develop tolerance to the drug’s therapeutic effects over a period of years, seen as a gradual breaking through of manic or depressive episodes that increase in severity or frequency. Others who are good long-term responders to lithium, but stop taking lithium and then suffer relapses, fail to respond as well as they had before. In a few instances, the drug no longer helps at all. This latter form of acquired lithium resistance is called lithium discontinuation-induced refractoriness.
In a review article published in the Journal of Affective Disorders in 2011, this editor (Robert Post) analyzed case series and case reports that depicted these two different types of acquired lithium resistance and reported that each must be addressed in a different way. In the case of tolerance development, a temporary break from lithium may theoretically restore its effectiveness, but the typical way to treat this situation is to add additional drugs with different mechanisms of action that are not affected by the tolerance.
In those who stop effective lithium treatment and experience relapses that are no longer responsive when lithium is re-instituted, it is not clear what the best treatment approaches are. Therefore the most conservative approach to preventive treatment with lithium is to avoid discontinuing the drug. This would appear to be a generally sound principle for the treatment of recurrent unipolar or bipolar illness. When things are going well, do not change the regimen; leave well-enough alone. Conversely, when treatment is not optimal, as in the case of loss of drug responsiveness via tolerance, a more aggressive exploration of treatment options would be warranted.
Patients should be aware of the multiple dangers of stopping effective treatment with lithium. These include: likely relapse, perhaps the necessity of hospitalization, an increased risk of suicide, and the loss of responsiveness to lithium that appears to occur in approximately 15% of patients who stop lithium when it is working effectively.
Ketamine Effective in ECT-Resistant Depression
 In an abstract presented at the Society of Biological Psychiatry meeting in May, Lobna Ibrahim and Carlos Zarate of the National Institute of Mental Health reported that intravenous infusions of ketamine were effective in a majority of patients with highly treatment-resistant depression, i.e. even those who had been unresponsive to a course of electroconvulsive therapy.
In an abstract presented at the Society of Biological Psychiatry meeting in May, Lobna Ibrahim and Carlos Zarate of the National Institute of Mental Health reported that intravenous infusions of ketamine were effective in a majority of patients with highly treatment-resistant depression, i.e. even those who had been unresponsive to a course of electroconvulsive therapy.
Editor’s note: Few treatments have been explored for this subgroup of highly treatment-resistant patients, although some have been referred for experimental protocols with intracranial deep brain stimulation (DBS) and others have been successfully treated by Mark George and colleagues at the Medical University of South Carolina with very high intensity rTMS over the left prefrontal cortex (at 130% of motor threshold, 10 Hz stimulation). Further study is needed to determine what follow-up procedures can be used to sustain an acute response to ketamine, rTMS, or ECT for the long term. Read more
Vitamins for Treatment-Resistant Childhood Bipolar Disorder?

Update (11/1/2010): According to Dr. Charles Popper of Massachusetts General Hospital and McLean Hospital, particular caution should be used when considering the combination of EMPowerplus with psychopharmacological medications. When used alone, the vitamin compound appears to be relatively safe. However, in combination with other drugs, Empowerplus appears to enhance the medications’ effects, both positive and adverse. So use of very low doses of the vitamin compound with gradual increases should be combined with appropriate decreases in doses of other medications.
Researcher Mary Fristad from Ohio State University completed a small, uncontrolled study of a novel treatment approach, the multi-vitamin and mineral preparation labeled EMPowerplus. Initial case reports from other researchers indicated that the compound led to remarkable and sustained effectiveness in children with bipolar disorder who were unresponsive to most other psychopharmacological approaches.
Fristad’s open study included ten children. Participants were slowly titrated to a minimum of 12 capsules/day with a maximum of 15 capsules/day.
Fristad and colleagues saw 37% improvement in depression and 45% improvement in mania in the entire group of patients who began treatment, while in those who completed the study, there was 71% improvement in depression and 58% improvement in mania. Side effects were benign, but the preparation needs to be administered judiciously in conjunction with a physician’s supervision.
Dr. Fristad hopes to conduct further double-blind, placebo-controlled trials of this compound, which also showed promising open results in case studies by Kaplan et al. in 2002 and 2004 and was written about by Charles Popper, a researcher at Massachusetts General Hospital, in 2001.
The EMPowerplus preparation is available at the web site http://truehope.com and costs approximately $100-200 per month, but is not recommended for use without careful supervision by a physician.
EDITOR’S NOTE: Controlled clinical trials to demonstrate efficacy have not yet been undertaken, partly due to lack of support from funding organizations and uncertainty about which of the many ingredients is active. Studies of pharmaceutical agents for treatment-resistant children without a cogent theoretical rationale are rarely a high priority despite the great need for effective treatment approaches.
Nonetheless, given initial promising results of the Fristad group and others, systematic clinical trials of this preparation are now clearly indicated.