Longer Periods of Untreated Depression Linked to More Brain Inflammation
 A 2018 study by researchers Elaine Setiawan, Sophia Attwells and colleagues reports that inflammation seems to increase with duration of untreated unipolar depression. This implies that depression may be a progressive illness, and later stage depression may require different treatments than early stage depression, such as those that directly target inflammation.
A 2018 study by researchers Elaine Setiawan, Sophia Attwells and colleagues reports that inflammation seems to increase with duration of untreated unipolar depression. This implies that depression may be a progressive illness, and later stage depression may require different treatments than early stage depression, such as those that directly target inflammation.
The study published in the journal The Lancet Psychiatry used positron emission tomography (PET scan) to examines levels of translocator protein in the brain. Higher levels of translocator protein indicate activation of microglia, the brain’s immune cells, which can respond to trauma or injury.
The study included 80 participants between the ages of 18 and 75. Ten had a history of more than 10 years of depression, ten had experienced fewer than 10 years of depression, and 30 comprised a healthy comparison group.
The best predictors of high levels of translocator protein were duration of untreated major depressive disorder, total illness duration, and duration of antidepressant exposure. These three factors explained about half of the variation in translocator protein levels. Those participants whose depression went untreated for 10 years or longer had inflammation levels 29–33% higher than those whose depression was untreated for 9 years or less.
Participants who had received antidepressant treatment appeared to avoid an average yearly increase in the extent of their microglial activation.
The study took place at Canada’s Centre for Addiction and Mental Health.
Editor’s Note: Since inflammation is a predictor of poorer response to antidepressants, these data add a further neurochemical rationale to the already strong clinical rationale for earlier and more sustained antidepressant treatment and prevention. Virtually all treatment guidelines suggest that after two or three prior unipolar depressions, patients should receive long-term (lifelong) antidepressant treatment.
There is now a large body of data, including a 2012 article by this editor Robert M. Post and colleagues in the Journal of Psychiatric Research that too many episodes can hurt the brain, and the current study adds to this perspective. Avoiding preventive treatment for too long may actually foster the development of more episodes and more treatment resistance. A good mantra is “prevent episodes, protect the brain.”
Consensus is now also building that comprehensive long-term treatment is indicated after a first manic episode. A 2013 article by Lars Kessing and colleagues in the British Journal of Psychiatry suggested that high quality initial treatment can improve the long-term course of illness. Moreover, a 2016 article by Jan-Marie Kozicky and colleagues and a 2017 article by Christine Demmo and colleagues, both in the journal Bipolar Disorders, suggest that after a first mania, cognition recovers over the next year only if no further episodes occur in that time.
Depression and Suicidal Thoughts Linked to Brain Inflammation
A 2017 article by Sophie E. Holmes and colleagues in the journal Biological Psychiatry reports that people with major unipolar depression, especially those with suicidal thoughts, have higher levels of the inflammatory marker translocator protein than do healthy individuals.
The participants with depression and suicidal thinking had high levels of translocator protein in the anterior cingulate cortex, which suggests that inflammation is affecting microglia.
Many studies have found links between different indicators of inflammation and mood disorders, leading researchers to speculate whether targeting the immune system could be an effective way to treat mood disorders. Patients with high levels of inflammation often fail to respond to typical treatments for depression.
Some previous research has found evidence of microglial activation in the brains of people who died from suicide.
The small study by Holmes and colleagues used positron-emission tomography, or PET scans, to observe evidence of translocator protein levels in the brain in 14 medication-free participants in a major depressive episode and 13 healthy volunteers. Those with depression, and particularly those with suicidal thoughts, showed more evidence of neuroinflammation.
Some Evidence of Brain Inflammation in Depression
 Many studies have found links between levels of inflammatory molecules in the blood and depression or depressive symptoms. There has been less research about inflammation in the brain and its possible role in depressive illness. Improvements in positron emission topography (PET) scan technology now allow for better brain imaging that can reveal when microglia are activated. (Microglia serve as the main immune responders in the central nervous system.)
Many studies have found links between levels of inflammatory molecules in the blood and depression or depressive symptoms. There has been less research about inflammation in the brain and its possible role in depressive illness. Improvements in positron emission topography (PET) scan technology now allow for better brain imaging that can reveal when microglia are activated. (Microglia serve as the main immune responders in the central nervous system.)
A study by researcher Jeffrey Meyer found evidence of microglial activation in several brain regions (including the prefrontal cortex, the anterior cingulate cortex, and the insula) in people in an episode of depression who were not receiving any treatments. Participants with more microglial activation in the anterior cingulate cortex and insula had more severe depression and lower body mass indexes.
Meyer, who presented this research at a scientific meeting in December, called it strong evidence for brain inflammation in depressive episodes, and suggested that treatments that target microglial activation would be promising for depression.
However, at the same meeting, researcher Erica Richards reported that she had not been able to replicate Meyer’s results. Her research, which included depressed participants both on and off medication and non-depressed participants, found that depressed participants did show more inflammation in the two brain regions she targeted, the anterior cingulate and the subgenual cortices, but this difference did not reach statistical significance, particularly when patients taking antidepressants were included in the calculations. Richards hopes that with a greater sample size, the data may show a significant difference in brain inflammation between depressed and non-depressed participants.
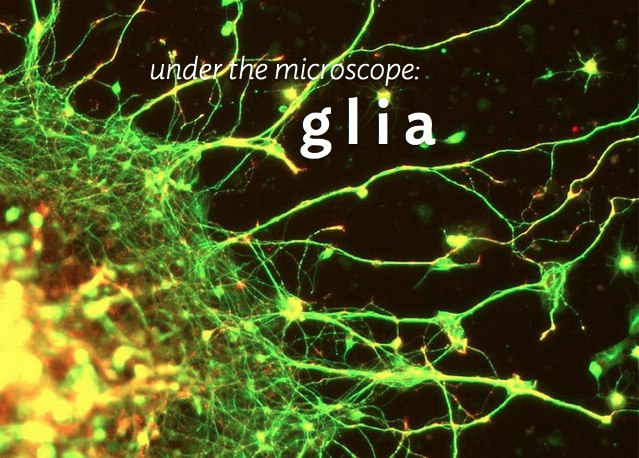
Glia Cells Prune Over-Abundant Neurons
The brain contains neurons, which transmit electrical impulses, and glia, which protect and support neurons. New evidence suggests that some types of glia also play a role in pruning back overabundant neurons that are produced as the brain develops in utero.
Researcher Beth Stevens reports that astrocytes secrete a protein called transforming growth factor beta (TGF-beta). TGF-beta is a cytokine, or regulating protein, that activates brain microglia to initiate a complement cascade (C1 to C3), a series of chemical changes that destroy unnecessary neurons and synapses.
The various proteins involved in a complement cascade are numbered. This complement cascade starts with C1q and is continued by C4, C2, and C3, which initiate phagocytosis (or eating up) of the axon terminals of the underutilized neurons, sparing those that are active.
Inflammation and other changes in glia could cause either deficient or excess pruning of neurons, which has been thought to occur in neuropsychiatric disorders such as autism or schizophrenia.