Brain Inflammation Found in Autopsy Studies of Teen and Adult Suicides
Suicide and depression have both been linked to elevated levels of inflammatory cytokines in the blood and cerebrospinal fluid. A recent study finds that these inflammatory markers are also elevated in the brains of teens and depressed adults who died from suicide.
In autopsy studies, researcher Ghanshyam N. Pandey measured levels of the inflammatory cytokines interleukin-1beta, interleukin 6, and TNF-alpha in the brains of teen suicide victims, and compared these to the brains of teens who died from other causes. Pandey also measured levels of interleukin-1beta, interleukin 6, interleukin 8, interleukin 10, interleukin 13, and TNF-alpha in the prefrontal cortex of depressed adult suicide victims and compared them to levels in adults who died of other causes.
There were abnormalities in the inflammatory markers in the brains of those who died from suicide compared to their matched controls. The suicide victims had higher levels of interleukin-1beta, interleukin 6, and TNF-alpha than the controls. Among the adults, levels of the anti-inflammatory cytokine interleukin 10 were low in the suicide victims while levels of Toll-like receptors (TLR3 and TLR4), which are involved in immune mechanisms, were high.
Brain inflammation has also been observed in positron emission tomography (PET) scans of depressed patients, where signs of microglial activation can be observed. Elevated inflammatory cytokines are also found in the blood of some people with bipolar disorder, depression, and schizophrenia.
Pandey presented this research at the 2016 meeting of the Society of Biological Psychiatry.
Repeated Sports Injuries Linked to Brain Inflammation
Professional football players face repeated mild traumatic brain injuries throughout their careers, and may face a variety of brain impairments, from depression to dementia, as a result.
A recent study by researcher Jennifer Coughlin and colleagues clarified how these impairments may be caused by repeated brain impacts. The researchers used positron emission tomography (PET) scans to observe the volume of translocator protein, a marker of brain injury and repair, in the brains of seven active or recently retired National Football League (NFL) players. Compared to healthy, athletic volunteers who were age-matched to the NFL players, the NFL players showed greater volume of translocator protein in several brain regions, including the left and right thalamus, the left and right temporal poles, and the brainstem.
It is not yet clear whether the increased volume of translocator protein is a sign of the brain’s attempts to repair itself, or whether it shows deterioration toward chronic traumatic encephalopathy. Translocator protein is also considered a marker of microglial activation, which occurs with inflammation.
High levels of translocator protein have also been seen in patients with depression and schizophrenia.
Some Evidence of Brain Inflammation in Depression
 Many studies have found links between levels of inflammatory molecules in the blood and depression or depressive symptoms. There has been less research about inflammation in the brain and its possible role in depressive illness. Improvements in positron emission topography (PET) scan technology now allow for better brain imaging that can reveal when microglia are activated. (Microglia serve as the main immune responders in the central nervous system.)
Many studies have found links between levels of inflammatory molecules in the blood and depression or depressive symptoms. There has been less research about inflammation in the brain and its possible role in depressive illness. Improvements in positron emission topography (PET) scan technology now allow for better brain imaging that can reveal when microglia are activated. (Microglia serve as the main immune responders in the central nervous system.)
A study by researcher Jeffrey Meyer found evidence of microglial activation in several brain regions (including the prefrontal cortex, the anterior cingulate cortex, and the insula) in people in an episode of depression who were not receiving any treatments. Participants with more microglial activation in the anterior cingulate cortex and insula had more severe depression and lower body mass indexes.
Meyer, who presented this research at a scientific meeting in December, called it strong evidence for brain inflammation in depressive episodes, and suggested that treatments that target microglial activation would be promising for depression.
However, at the same meeting, researcher Erica Richards reported that she had not been able to replicate Meyer’s results. Her research, which included depressed participants both on and off medication and non-depressed participants, found that depressed participants did show more inflammation in the two brain regions she targeted, the anterior cingulate and the subgenual cortices, but this difference did not reach statistical significance, particularly when patients taking antidepressants were included in the calculations. Richards hopes that with a greater sample size, the data may show a significant difference in brain inflammation between depressed and non-depressed participants.
Brain Inflammation in People at High Risk for Schizophrenia
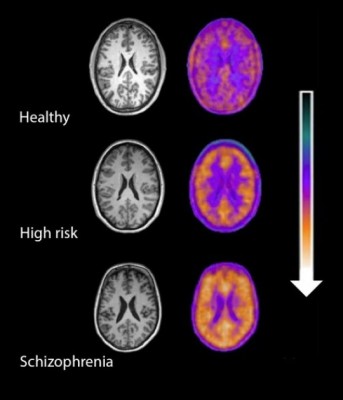
Microglial activity in the brains of people who are healthy, people at high risk for schizophrenia, and people who have been diagnosed with schizophrenia.
A 2016 study by Peter S. Bloomfield and colleagues in the American Journal of Psychiatry used PET scans to compare the activity of microglia, immune cells in the central nervous system, in healthy controls, people with schizophrenia, and those at high risk for the illness. It found that both people with schizophrenia and those at high risk had greater brain inflammation than the healthy controls.
The study was the first to show that microglial activity was elevated in people at high risk (who showed some preliminary symptoms of schizophrenia). The finding had a large effect size.
Microglial activity was also correlated with symptom severity in the high-risk participants. Increased microglial activity was not linked to depression, suggesting that it is specific to the development of psychosis.
These findings resemble those of other recent studies showing increased inflammation in people at high risk for psychosis.
The study suggests that increased microglial activity occurs before a first episode of psychosis. That means it could help identify people who may develop schizophrenia. The findings also suggest that anti-inflammatory treatment could theoretically be used to prevent psychosis.



