Measuring Inflammation in Neuropsychiatric Disorders May Shed Light on Treatment
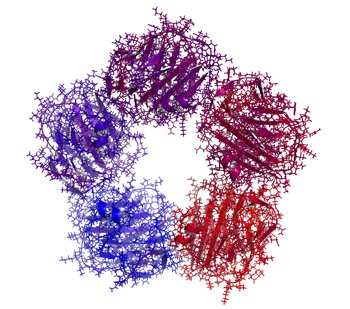
Meta-analyses have found links between elevated levels of inflammatory markers and many neuropsychiatric disorders, including depression, bipolar disorder, schizophrenia, post-traumatic stress disorder (PTSD) and traumatic brain injury. Multiple studies also show that those with elevated inflammatory markers such as interleukin-1, interleukin-6, tumor necrosis factor (TNF) alpha, and c-reactive protein (CRP) also respond less well to typical treatments than those with normal levels of these markers in the blood.
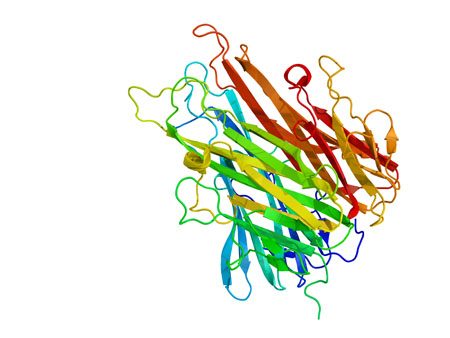
These links suggest that it could be useful to measure levels of these inflammatory markers in the blood of people who are responding poorly to medications. If one or more of these markers are elevated, it might be a sign that treatment with an anti-inflammatory agent could be helpful. Preliminary studies have shown that some neuropsychiatric disorders may improve after treatment with anti-inflammatory drugs such as aspirin, celecoxib (Celebrex), and the antibiotic minocycline, among others.
Arthritis Drug Celecoxib May Improve Bipolar Depression When Paired with Escitalopram
A new study suggests that for people with bipolar depression, the anti-inflammatory drug celecoxib (Celebrex), typically used to treat arthritis, can boost the effectiveness of the antidepressant escitalopram (Lexapro).
In the 8-week study by researcher Angelos Halaris and colleagues, adults with bipolar depression were randomly assigned to one of two groups. The first group received the selective-serotonin reuptake inhibitor (SSRI) antidepressant escitalopram plus celecoxib to target inflammation. The second group received just the antidepressant escitalopram and a placebo.
By the end of the study, 78% of the group taking the anti-arthritis drug had seen major improvement in their depression, with 63% reporting that it had lifted completely. Meanwhile in the placebo group, only 45% reported major improvement, and 10% reported remission.
The group that received celecoxib with their escitalopram also began seeing improvement within one week of beginning treatment, instead of after four to six weeks, which is typical of antidepressant treatment.
Researchers think depression creates an immune response leading to chronic inflammation, which can upset the balance of neurotransmitters in the brain and make antidepressants less effective. Halaris suggests that reducing this inflammation with a drug like celecoxib can make antidepressants more effective.
The research was presented at the Fifth International Congress on Psychiatry and the Neurosciences and has not yet been published.
Inflammatory Marker CRP Higher in Bipolar Disorder, Particularly Mania
Inflammation has been linked to mood disorders. A 2016 meta-analysis in the journal Lancet Psychiatry described the role of inflammatory marker C-reactive protein (CRP) in bipolar episodes. Researchers led by Brisa S. Fernandes identified 27 studies that measured CRP levels in a total of 2,161 patients with bipolar disorder and 81,932 healthy participants. The researchers determined that compared to healthy controls, people with bipolar disorder have higher levels of CRP. CRP levels were moderately elevated between episodes and during depression, and substantially elevated during episodes of mania.
Editor’s Note: This meta-analysis shows that CRP is linked to bipolar disorder, and the inflammatory burden is highest during mania. It remains to be seen whether anti-inflammatory treatments work best in patients with high CRP levels compared to normal CRP levels.
CRP is also a risk factor for cardiovascular disease, and lithium and other treatments for bipolar disorder probably lower CRP levels.
The same group of researchers previously showed that statins, drugs typically used to lower cholesterol, could help alleviate depression. Since statins have anti-inflammatory effects, they can probably reduce depression risk in addition to lowering cardiovascular risk, as initial studies suggest.
Other drugs with anti-inflammatory effects that may improve depression include the anti-arthritis drug celecoxib and the antibiotic minocycline. The amino acid N-acetylcysteine and omega-3 fatty acids also have anti-inflammatory effects and have been found to improve depression in some studies.
Anti-Inflammatory Treatments Improve Depression
Inflammation can interfere with the balance of neurotransmitters in the brain, making antidepressants less effective. Anti-inflammatory treatments (such as those used to treat rheumatoid arthritis) may help. In a 2016 meta-analysis published in the journal Molecular Psychiatry, researchers led by Nils Kappelmann analyzed the results of 20 clinical trials of chronic inflammatory conditions where depressive symptoms were also recorded. In a subset of 7 clinical trials that compared anti-inflammatory treatment to placebo, they found that anti-inflammatory treatment improved depressive symptoms significantly compared to placebo.
The anti-inflammatory drugs studied most often targeted the inflammatory marker tumor necrosis factor (TNF) alpha using an antibody. Some of the anti-inflammatory drugs that improved depressive symptoms were adalimumab, etanercept, infliximab, and tocilizumab.
The researchers also found that those participants with the most inflammation when they began treatment saw the largest improvement in their depression after taking anti-inflammatory treatments.
Kappelmann and colleagues suggest that inflammation may cause depression, and that anti-inflammatory drugs may be useful in the treatment of depression in people with high inflammation.
Preventative Treatment Should Begin After First Manic Episode
Evidence from multiple studies has indicated the importance of beginning preventative treatment, particularly with lithium, early in the course of bipolar disorder. A 2016 comprehensive literature review by researcher Katie Joyce and colleagues in the International Journal of Bipolar Disorders concluded that psychoeducation and medication are more effective in bipolar disorder when applied in earlier stages of the illness rather than later stages.
Several studies suggest that treatment for bipolar disorder should be started specifically after the first manic episode.
A 2014 study by researcher Lars Kessing and colleagues in the British Journal of Psychiatry examined 4,700 patients treated with lithium in Denmark. Kessing and colleagues found that those who started treatment after one manic episode were less likely to find lithium ineffective than those who started later.
Another study by researcher Michael Berk and colleagues presented at the International Society for Bipolar Disorders found that after a first manic episode, a year of treatment with lithium was much more effective on all measures of outcome, including mania and depression ratings, brain imaging, and neuropsychological functioning, than a year when patients were randomized to quetiapine (Seroquel).
Researcher Lakshmi Yatham and colleagues presented research at the International Society for Bipolar Disorders showing that patients recovered from the neuropsychological deficits associated with a first episode of mania if they were well treated and had no further episodes, while those who had new episodes did not return to their baseline capabilities. This suggests that early treatment that prevents future episodes helps maintain a healthy brain.
Kessing and colleagues previously reported in the British Journal of Psychiatry in 2013 that patients randomized to two years of treatment in an outpatient clinic specializing in mood disorders following a first hospitalization for mania had 40% fewer recurrences of bipolar episodes over the next six years than those who received treatment as usual. These data indicate that early treatment, which may include psychotherapy, medications, mood charting (i.e. keeping a daily record of symptoms) and illness education, can improve the long-term course of illness. Lithium is often a key component of such treatment.
Editor’s Note: This type of intensive, ongoing treatment is not the norm after a first manic hospitalization in the United States, but it should be. Given the new data on the impact of starting lithium after a first episode of mania, and lithium’s superiority over quetiapine in the year following a first episode, lithium treatment should be standard following a diagnosis of bipolar disorder.
In the past, sometimes doctors have recommended waiting until a patient has had multiple episodes of mania before beginning preventative treatment with lithium. This now appears to be a mistake.
Lithium protects against depressive as well as manic recurrences, and there is also evidence that it increases hippocampal and cortical volume, helping prevent cognitive deterioration in those with mild cognitive impairment. Lithium is also the most effective mood stabilizer for preventing suicide, and it increases the length of telomeres (caps on the end of DNA strands), thus preventing a wide range of medical and psychiatric illnesses. Lithium may need to be combined with other drugs to achieve a complete remission, but using it after a first mania is a good place to start.