Good Outcomes Among Patients with Major Depressive Disorder Treated with Transcranial Magnetic Stimulation in a Large Study

At the 2021 meeting of the Society of Biological Psychiatry (SOBP), researcher Harold Sackeim and colleagues reported on data collected from patients in clinical treatment for major depression who received transcranial magnetic stimulation (TMS) at 103 practice sites. A total of 5,010 depressed patients were included in the intent-to-treat sample, and 3,814 completed the study, meaning that they either reached remission or were treated at least 20 times and went through a final assessment. “Response (58–83%) and remission (28–62%) rates were notably high across self-report and clinician-administered assessments,” and women had better outcomes than men. Sackeim and colleagues concluded, “Strong efficacy and the low side effect and medical risk profile suggest that TMS be evaluated as a first-line treatment for [major depressive disorder].”
Accelerated Intermittent Theta-Burst Stimulation (aiTBS) Quickly Improved Treatment-Resistant Depression

At the 2021 meeting of the Society of Biological Psychiatry (SOBP), researcher Nolan Williams and colleagues described a sham-controlled trial of accelerated intermittent theta-burst stimulation (aiTBS) in patients with treatment-resistant depression. Theta burst stimulation is a specific protocol for rTMS, or repeated transcranial magnetic stimulation, a non-invasive form of brain stimulation. Magnets placed on a patient’s head provide bursts of high-frequency stimulation to the brain.
Participants in the study received 50 sessions over 5 days of either aiTBS or a sham procedure. Among those who received the real aiTBS treatment, 85.7% saw an improvement in their treatment-resistant depression, compared to only 26.7% of those in the sham group. AiTBS produced a rapid antidepressant response, which Williams and colleagues suggest could be useful for the treatment of patients in emergency rooms or inpatient settings.
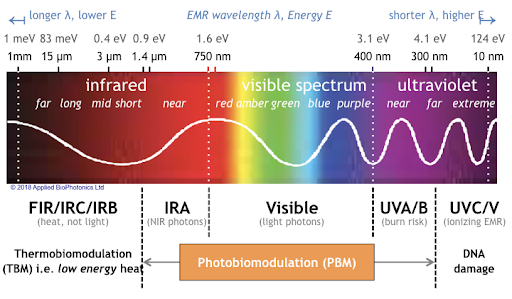
Transcranial Near-Infrared Light May Treat Brain Injury and Neurodegeneration
At the 2021 meeting of the Society of Biological Psychiatry, there was a symposium on treatment with near-infrared light chaired by researchers Paolo Cassano and Dan Iosifescu. The treatment is known as transcranial photobiomodulation (PBM) with near-infrared light. A device worn on the head delivers infrared light that penetrates the cerebral cortex and can modulate cortical excitability. It has a variety of effects including promoting neuroplasticity, improving oxygenation, and decreasing inflammation and oxidative stress.
A number of studies exploring the possibility that PBM could be used as a clinical treatment for conditions such as depression, brain injury, or dementia were presented at the symposium.
Researcher Lorelei Tucker discussed promising findings from an animal model in which rats with stroke or brain injuries showed improvement after being treated with PBM.
Cassano discussed studies aimed at refining which brain areas should be targeted with PBM and how much light should be delivered in order to improve depression. In double-blind, sham-controlled studies in people with major depression, targeting the dorsolateral prefrontal cortex with PBM improved their symptoms.
Researcher Benjamin Vakoc discussed a study of low-level light therapy (LLLT) using near-infrared light compared to a sham procedure in 68 people with moderate traumatic brain injury. The researchers used magnetic resonance imaging (MRI) to assess changes in white matter in the brain over time in people recovering from an acute brain injury. Patterns of changes in white matter were different for those who received LLLT compared to those who received the sham procedure.
Researcher Linda Chao described a very small study to determine whether PBM could improve symptoms of dementia. Four patients received typical dementia care while four others underwent home treatments with the commercially available Vielight Neuro Gamma device, which delivers PBM via both the scalp and an insert in the nose. After 12 weeks, the PBM group showed improvements in cognition and brain connectivity.

Editor’s Note: We will be watching the literature to follow advances in this promising novel method of neuromodulation.
Participation in Sports May Mitigate Genetic Risk for ADHD in School-Aged Children

At the 2021 meeting of the Society of Biological Psychiatry, researcher Keiko Kunitoki and colleagues reported that participation in sports decreased behavior abnormalities in 9- and 10-year-old children at genetic risk for attention deficit hyperactivity disorder (ADHD). Sports were associated with greater hippocampal volume, which was associated with fewer behavioral abnormalities. Kunitoki and colleagues concluded that “participation in team sports mitigated genomic risk for psychopathology at age 9–10 in part through increased hippocampal volume.”
Editor’s Note: These data are consistent with a program called the Vermont Family-Based Approach developed by researcher James Hudziak, who heads the Vermont Center for Children, Youth and Families at the University of Vermont. The program encourages families to practice different domains of wellness, such as music, mindfulness, exercise, and nutrition, among others. The idea is to support emotional and behavioral health, and to do so intensively in families where children show signs of mood and behavioral difficulties or are at risk for these difficulties.
Hudziak analyzed brain scans of 232 children aged 6 to 18 and reported that “practicing an instrument such as the piano or violin increased working memory, gray matter volume in the brain, and the ability to screen out irrelevant noise. Practicing mindfulness increased white matter volume and reduced anxiety and depression. Exercise also increased brain volume and neuropsychological abilities.”
In 2015, researcher Benjamin I. Goldstein reported that 20 minutes of vigorous exercise on a bike improved cognition and decreased hyperactivity in the medial prefrontal cortex in adolescents with and without bipolar disorder, and researcher Danella M. Hafeman reported that offspring of parents with bipolar disorder who exercised more had lower levels of anxiety.
To summarize, engaging in exercise, team sports, music, and meditation/mindfulness are beneficial for all children, and can be especially helpful for those at risk for depression or bipolar disorder. Children who are already symptomatic should additionally be offered something like family focused therapy (FFT), a multi-faceted approach developed by researcher David Miklowitz, in which families of young people at risk for bipolar disorder take part in therapy, learning together about the illness and practicing strategies for communication and coping.
Surface Area of Cortex Is Reduced After Multiple Manic Episodes
In a 2020 article in the journal Psychiatric Research: Neuroimaging, researcher Rashmin Achalia and colleagues described a study of structural magnetic resonance imaging (MRI) that compared 30 people with bipolar I disorder who had had one or several episodes of mania to healthy volunteers. Compared to the healthy volunteers, people with bipolar disorder had “significantly lower surface area in bilateral cuneus, right postcentral gyrus, and rostral middle frontal gyri; and lower cortical volume in the left middle temporal gyrus, right postcentral gyrus, and right cuneus.”
The surface area of the cortex in patients with bipolar I disorder who had had a single episode of mania resembled that of the healthy volunteers, while those who had had multiple manic episodes had less cortical surface area.
The data suggest that compared to healthy volunteers, people with bipolar disorder have major losses in brain surface area after multiple episodes that are not seen in first episode patients. In addition, the researchers found that both the number of episodes and the duration of illness was correlated with the degree of deficit in the thickness in the left superior frontal gyrus. These decreases in brain measures occurred after an average of only 5.6 years of illness.
Editor’s Note: These data once again emphasize the importance of preventing illness recurrence from the outset, meaning after the first episode. Preventing episodes may prevent the loss of brain surface and thickness.
Clinical data has also shown that multiple episodes are associated with personal pain and distress, dysfunction, social and economic losses, cognitive deficits, treatment resistance, and multiple medical and psychiatric comorbidities. These and other data indicate that treatment after a first episode must be more intensive, multimodal, and continuous and include expert psychopharmacological and psychosocial support, as well as family education and support. Intensive treatment like this can be life-saving. The current study also supports the mantra we have espoused: prevent episodes, protect the brain and the person.

