Inflammation Predicts Depression and Anxiety Four Years Later in Older Americans
A large study of retired Americans found that those with high levels of the inflammatory marker C-reactive protein in the blood had more depression and anxiety. Higher CRP also predicted severity of depression and anxiety four years later.
The study, by researchers Joy E. Lin and Aoife O’Donovan, included 18,603 people over age 50 from the Health and Retirement Study. It was presented at the 2016 meeting of the Society of Biological Psychiatry.
Lin and O’Donovan hope that treating or preventing inflammation may be the key to preventing symptoms of depression and anxiety.
Psychotherapy Improved Depression, Reduced Inflammation
A recent study shows that psychotherapy can not only improve depression symptoms, but may also reduce the inflammation that often accompanies them.
Researcher Jean Pierre Oses and colleagues randomly assigned participants with depression to receive Supportive-Expressive psychodynamic therapy, which is designed to help patients understand conflictual relationship patterns, or an alternative therapy. Among the 47 participants who received Supportive-Expressive therapy, depression improved significantly after 16 sessions, and blood levels of the inflammatory markers interleukin-6 and TNF alpha also dropped.
The research was presented at the 2016 meeting of the Society of Biological Psychiatry.
Kynurenine Pathway Suggests How Inflammation is Linked to Schizophrenia
The kynurenine pathway describes the steps that turn the amino acid tryptophan (the ingredient in turkey that might make you sleepy) into nicotinamide adenine dinucleotide. This pathway might be a connection between the immune system and neurotransmitters involved in schizophrenia.
A recent autopsy study by researcher Thomas Weickert and colleagues explored this link by determining that in the brains of people with schizophrenia and high levels of inflammation, messenger RNA for Kynurenine Aminotransferase II (KATII, a step on the kynurenine pathway) was elevated in the dorsolateral prefrontal cortex compared to the brains of people who died healthy and those with schizophrenia but low levels of inflammation.
The KATII mRNA levels also correlated with mRNA levels of inflammatory markers such as glial fibrillary acidic protein and interleukin-6.
Blood measures related to the kynurenine pathway also differentiated people with schizophrenia from healthy controls. People with schizophrenia had lower levels of tryptophan, kynurenine, and kynurenic acid in their blood. The low levels of kynurenic acid in the blood were correlated with deficits in working memory and smaller volume of the dorsolateral prefrontal cortex.
Weickert and colleagues suggest that blood levels of kynurenic acid might provide a measurable indicator of the degree to which people with schizophrenia are experiencing problems with executive functioning (planning and decision-making) and loss of brain volume.
Meta-Analysis Shows Inflammation is Common in Unipolar Depression, Bipolar Depression, and Schizophrenia
In a symposium at the 2016 meeting of the Society of Biological Psychiatry, Mark Hyman Rapaport described the results of his research group’s meta-analysis of studies comparing levels of inflammation in the blood of people with unipolar depression, bipolar depression, and schizophrenia. Rapaport and colleagues determined that people acutely ill with any of the three illnesses showed abnormally high levels of certain inflammatory proteins. These included: interleukin-1beta, interleukin-6, TNF alpha, and c-reactive protein. Those who were chronically ill showed elevations in interleukin-6.
These data are consistent with increasing evidence that inflammation also occurs in the brain. Brain inflammation can be observed by measuring translocator protein binding, a measure of brain microglial activation, using positron emission tomography (PET) scans.
Fluctuations in White Matter in Adolescents with Bipolar Disorder May Indicate Cardiovascular Risk
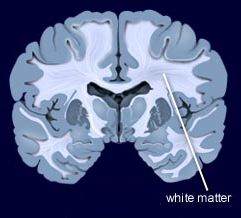 During functional magnetic resonance imaging (fMRI) of the brain, data on physiological fluctuations in white matter are collected. These fluctuations are caused by cardiac pulses, cerebrovascular dysfunction, and other factors. Increasing fluctuations have been linked to cognitive impairment with age.
During functional magnetic resonance imaging (fMRI) of the brain, data on physiological fluctuations in white matter are collected. These fluctuations are caused by cardiac pulses, cerebrovascular dysfunction, and other factors. Increasing fluctuations have been linked to cognitive impairment with age.
Vascular problems in adults with bipolar disorder have been linked to cerebrovascular disease, a group of conditions that affect bloodflow to the brain. In a recent study, researcher Arron W. S. Metcalfe and colleagues used data on physiological fluctuations in white matter (usually a nuisance variable) to assess the vascular health of teens with bipolar disorder. Compared to 32 age-, IQ-, and sex-matched controls, 32 adolescents with bipolar disorder had more fluctuations in white matter in three different clusters in the brain.
These white matter fluctuations are a possible early indicator of susceptibility to cerebrovascular disease in teens with bipolar disorder. Patients with depression and bipolar disorder are at increased risk for cardiovascular disease, so maintaining a good diet, exercising regularly, and assessing blood pressure, cholesterol, and lipid levels is recommended. See page __ where we describe research showing teens with bipolar disorder have stiffer artery walls.
Teens with Bipolar Disorder Have More Inflammation, Cardiovascular Risks
 Bipolar disorder has been linked to cardiovascular disease. New research by Jessica Hatch and colleagues shows that inflammation may be at the root of this connection. At the 2016 meeting of the Society of Biological Psychiatry, the researchers showed that teens with bipolar disorder have higher levels of inflammatory marker interleukin 6.
Bipolar disorder has been linked to cardiovascular disease. New research by Jessica Hatch and colleagues shows that inflammation may be at the root of this connection. At the 2016 meeting of the Society of Biological Psychiatry, the researchers showed that teens with bipolar disorder have higher levels of inflammatory marker interleukin 6.
Hatch and colleagues assessed the blood of 60 teens with bipolar I or II disorder and 20 healthy controls for a variety of biomarkers, including the inflammatory proteins interleukin 6, interleukin 10, and TNF alpha; VEGF, which is responsible for the production of new blood vessels; and brain-derived neurotrophic factor (BDNF), which protects neurons. The researchers also assessed the participants’ cardiovascular health, performing the carotid intima media thickness test to estimate how much plaque is in the arteries, and measuring how well the patients’ arteries dilate in response to changes in bloodflow.
Participants with bipolar disorder had higher levels of interleukin 6 than healthy controls, regardless of whether their bipolar illness was symptomatic. Low BDNF was linked to greater carotid intima thickness in participants with symptomatic bipolar disorder, and vascular measurements suggest a possible mechanism by which bipolar disorder increases cardiovascular risk.
Brain Inflammation Found in Autopsy Studies of Teen and Adult Suicides
Suicide and depression have both been linked to elevated levels of inflammatory cytokines in the blood and cerebrospinal fluid. A recent study finds that these inflammatory markers are also elevated in the brains of teens and depressed adults who died from suicide.
In autopsy studies, researcher Ghanshyam N. Pandey measured levels of the inflammatory cytokines interleukin-1beta, interleukin 6, and TNF-alpha in the brains of teen suicide victims, and compared these to the brains of teens who died from other causes. Pandey also measured levels of interleukin-1beta, interleukin 6, interleukin 8, interleukin 10, interleukin 13, and TNF-alpha in the prefrontal cortex of depressed adult suicide victims and compared them to levels in adults who died of other causes.
There were abnormalities in the inflammatory markers in the brains of those who died from suicide compared to their matched controls. The suicide victims had higher levels of interleukin-1beta, interleukin 6, and TNF-alpha than the controls. Among the adults, levels of the anti-inflammatory cytokine interleukin 10 were low in the suicide victims while levels of Toll-like receptors (TLR3 and TLR4), which are involved in immune mechanisms, were high.
Brain inflammation has also been observed in positron emission tomography (PET) scans of depressed patients, where signs of microglial activation can be observed. Elevated inflammatory cytokines are also found in the blood of some people with bipolar disorder, depression, and schizophrenia.
Pandey presented this research at the 2016 meeting of the Society of Biological Psychiatry.
Brain Volumes Affected by Type and Timing of Childhood Abuse
Maltreatment during childhood has been linked to brain changes and mental illness. In a study by researcher Carl M. Anderson and colleagues that was presented at the 2016 meeting of the Society of Biological Psychiatry, maltreatment at particular ages was statistically linked to deficits in the size of certain brain areas in young adulthood.
The brain areas under examination are critical for the regulation of emotion and behavior, and this research suggests that early experiences can stunt their development, perhaps through altered production of synapses or via the synaptic pruning process that occurs during preadolescence. The details, summarized below, are perhaps less important than the overall finding that maltreatment in childhood affects brain volume, and this effect varies based on the timing and type of maltreatment. Abuse and neglect earlier in life affected the left side of the brain, while later maltreatment affected the right side.
Severity of physical abuse at age 3 affected the volume of the ventromedial prefrontal cortex in women. Physical abuse at ages 3 and 8 in men affected left ventromedial prefrontal cortical volume, while later abuse at ages 7 and 12 predicted volume of the right side.
In women, dorsal anterior cingulate area on the left was predicted by physical abuse at age 5 and by emotional neglect at ages 7 and 11. Later emotional neglect at ages 15 and 16 and physical abuse by a peer at age 10 was associated with smaller right dorsal anterior cingulate. In men, smaller left dorsal anterior cingulate area was predicted by physical neglect at age 2 and emotional abuse by a peer and witnessing abuse of a sibling at ages 5 and 10, and right area by physical neglect at age 12.
Early Life Stress Affects Volume of the Hippocampus
New research shows that there are crucial periods of early life in which a stressful event can reduce hippocampal volume in adolescence. In a study presented at the 2016 meeting of the Society of Biological Psychiatry, Kathryn L. Humphreys and colleagues found that children who experienced a significant stressor before age 8 had smaller hippocampi in early adolescence than children who did not have a significant stressor early in life.
The severity of the stressors that occurred when children were between the ages of 0 and 2 predicted the volume of the hippocampus later in life. This was true to a lesser extent for stressful events that occurred between the ages of 3 and 5. No effect was seen for stressful events that took place between the ages of 6 and 8.
The period of sensitivity to stressful events between ages 0 and 2 and its effects on hippocampal volume could influence a variety of psychiatric outcomes in conditions such as depression and post-traumatic stress disorder (PTSD).
Amygdala Hyperactivity Linked to Family History of Depression
In new research presented at the 2016 meeting of the Society of Biological Psychiatry, researcher Tracy Barbour and colleagues revealed that youth with a family history of depression showed more amygdala activation in response to a threat than people without a family history of depression. This amygdala hyperactivity was linked to low resilience to stress and predicted worsening depressive symptoms over the following year.
In the study, 72 non-depressed youth were shown images of cars or human faces or cars that seemed to loom in a threatening way. Brain scans showed increased amygdala activity in participants with a family history of depression compared to those without such a history.
The amygdala is an almond-shaped part of the brain in the temporal lobe that has been linked to emotional reactions and memory, decision-making, and anxiety.









