Inflammatory marker CRP predicts worse course of adolescent bipolar disorder
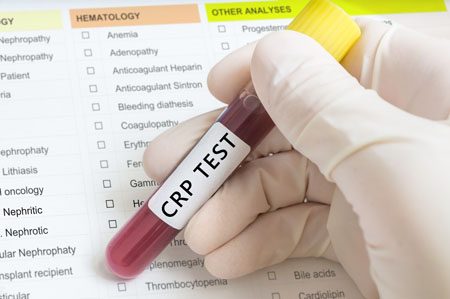
Sudhir Karthikeyan in Ben Goldstein’s lab in Toronto reported in Brain Behav Immun (2022) that in 79 adolescents the inflammatory marker CRP (C-Reactive Protein) was higher and the anti-inflammatory cytokine Il-10 was lower during the most ill periods compared to normal volunteers. “Moreover, higher CRP levels (p = 0.009) at intake predicted greater time to recovery from the index symptomatic episode.” They concluded that: “In the first repeated-measures study on this topic in adolescents with BD, we found evidence that CRP, an inexpensive and ubiquitous blood test, may be useful in predicting the prospective course of BD symptoms. “
Baseline Levels of CRP Could Help Predict Clinical Response to Different Treatments
C-reactive protein, or CRP, is a marker or inflammation that has been linked to depression and other illnesses. People with high levels of CRP respond differently to medications than people with lower CRP, so assessing CRP levels may help determine which medications are best to treat a given patient.
High baseline levels of CRP (3–5pg/ml) predict a poor response to selective serotonin reuptake inhibitor antidepressants (SSRIs) and to psychotherapy, and are associated with increased risk of recurrent depression, heart attack, and stroke.
However, high baseline CRP predicts a better response to the antidepressants nortriptyline and bupropion. High CRP is also associated with better antidepressant response to infliximab (a monoclonal antibody that inhibits the inflammatory cytokine TNF alpha), while low levels of CRP predict worsening depression upon taking infliximab.
High baseline CRP also predicts good antidepressant response to intravenous ketamine (which works rapidly to improve treatment-resistant depression), minocycline (an anti-inflammatory antibiotic that decreases microglial activation), L-methylfolate (a supplement that can treat folate deficiency), N-acetylcysteine (an antioxidant that can improve depression, pathological habits, and addictions), and omega-3 fatty acids (except in people with low levels of DHA).
High baseline CRP also predicts a good response to the antipsychotic drug lurasidone (marketed under the trade name Latuda) in bipolar depression. In people with high baseline CRP, lurasidone’s positive results have a huge effect size of 0.85, while in people with low CRP (<3pg/ml) the improvement on lurasidone has a smaller effect size (0.35).
In personal communications with this editor (Robert M. Post) in 2018, experts in the field (Charles L. Raison and Vladimir Maletic) agreed that assessing baseline CRP levels in a given patient could help determine optimal strategies to treat their depression and predict the patient’s responsiveness to different treatment approaches.
At a 2018 scientific meeting, researchers Cynthia Shannon, Thomas Weickert, and colleagues reported that high baseline levels of CRP were associated with symptom improvement in patients with schizophrenia when they were treated with the drug canakinumab (marketed under the trade name Ilaris). Canakinumab is a human monoclonal antibody that targets the inflammatory cytokine interleukin-1 beta (Il-1b). Il-1b is elevated in a subgroup of patients with depression, bipolar disorder, or schizophrenia, and CRP levels are an indication of the associated inflammation.
Il-6 Inhibitor Sirukumab May Improve Anhedonia, But Not General Depression
 At a 2018 scientific meeting, researcher Giacomo Salvadore and colleagues reported that the drug sirukumab, a monoclonal antibody that targets the inflammatory marker Il-6 and that was originally developed to treat rheumatoid arthritis, did not have a statistically significant effect on overall depression compared to placebo. However, by the twelfth week of treatment, sirukumab did have a significant effect on anhedonia (loss of interest or pleasure in activities that one previously enjoyed).
At a 2018 scientific meeting, researcher Giacomo Salvadore and colleagues reported that the drug sirukumab, a monoclonal antibody that targets the inflammatory marker Il-6 and that was originally developed to treat rheumatoid arthritis, did not have a statistically significant effect on overall depression compared to placebo. However, by the twelfth week of treatment, sirukumab did have a significant effect on anhedonia (loss of interest or pleasure in activities that one previously enjoyed).
The degree of improvement in anhedonia was significantly correlated with patients’ baseline levels of the inflammatory marker CRP. Since the inflammatory marker that sirukumab targets, Il-6, is one of those most often elevated in depression, it appears that more study of sirukumab would be warranted.
Inflammation Linked to Poor Sleep Quality and Worse Executive Functioning
At a recent scientific meeting, researcher Ellen E. Lee and colleagues reported that compared to healthy volunteers, people with bipolar disorder or schizophrenia had elevated levels of inflammatory markers, which were associated with poor sleep.
According to self-reports, people in the schizophrenia and bipolar disorder group had worse sleep quality than the control group. Those with schizophrenia or bipolar disorder also had significantly higher levels of the inflammatory markers CRP, IL-6, and TNF alpha compared to the healthy volunteers. Among people with bipolar disorder, executive functioning and sleep quality had a strong inverse association to levels of IL-6, such that lower sleep quality and worse executive functioning were associated with higher levels of IL-6. These findings suggest that sleep disturbance and inflammation may have negative consequences for cognitive functioning.
High Baseline Levels Of C-Reactive Protein Predict Better Response To Lurasidone in Bipolar Depression
In a study presented at the 2017 meeting of the International Society for Affective Disorders, Charlies L. Raison and colleagues examined whether baseline levels of the inflammatory marker C-reactive protein (CRP) affected antidepressant response to the antipsychotic drug lurasidone in bipolar depression. The participants were divided into three double-blind groups: one received 20–60mg/day of lurasidone, another received 80–120 mg/day of lurasidone, and the third received placebo over a period of six weeks. The effect was dramatic—in people with CRP levels above 5 mg/L at the beginning of the study, lurasidone (at either dosage level) had a very large effect size (d=0.85), while in people with baseline CRP levels below 5 mg/L the effect size was smaller (d=0.35).
Interestingly, 118 of the participants (24.5%) had CRP levels above 5mg/L at baseline, indicating a substantial amount of inflammation was present in a quarter of the bipolar depressed patients. Higher levels of CRP at baseline were correlated with better improvement on specific items on the Montgomery–Åsberg Depression Rating Scale (MADRS): “lassitude” (or lack of energy), “apparent sadness,” “reported sadness,” and “pessimistic thoughts.” Raison and colleagues concluded: “These findings suggest that the efficacy of lurasidone in patients with bipolar depression may in part be linked to the inflammatory status of patients prior to treatment. If confirmed in prospective investigations, [the results of a wide-range CRP assay] may prove useful as a predictive biomarker that could help optimize the use of lurasidone for the treatment of patients with bipolar depression.”
Editor’s Note: In many instances, high levels of CRP predict a poor response to treatment (such as to selective serotonin reuptake inhibitor antidepressants (SSRIs) in unipolar depression), so these findings are of considerable interest. They also suggest the untested possibility that lurasidone has anti-inflammatory effects, as those with high levels of inflammation at baseline often respond better to drugs with direct anti-inflammatory effects such as celecoxib (Celebrex) or the antioxidant N-acetylcysteine (NAC).
Inflammation is Associated with Antidepressant Treatment Resistance
Researcher Ebrahim Haroon and colleagues report in a 2018 issue of Psychoneuroendocrinology that people whose depression failed to respond to at least three different antidepressants in their current episode of depression had higher levels of inflammation than those who had fewer than three failed antidepressant trials.
The researchers found that patients who had not responded to antidepressants had higher levels of the inflammatory markers TNF-alpha, TNF-alpha receptor 2, and Il-6. The inflammatory marker CRP was also significantly elevated in these patients when statistical analyses that excluded body mass index (BMI) were used.
Haroon and colleagues reported that a third of all patients with major depressive disorder fail to respond to currently available antidepressant treatments, and that inflammation may be to blame because it interferes with the neurotransmitter systems that antidepressants target.
Editor’s Note: These data indirectly support the use of anti-inflammatory drugs to augment the effects of antidepressants in patients with treatment resistant depression. A caution that may be very important is to assess evidence of inflammation at baseline, as some data suggest that people with low CRP may, for example, do more poorly with a blocker of TNF-alpha, while people with high CRP at baseline (over 3 pg/ml) show good improvement.
Mysteries Remain in the Relationship Between Inflammation and Depression
At the 2017 meeting of the American College of Psychiatrists, researchers Charles L. Raison and Vladimir Maletic gave a plenary lecture on the role of inflammation in depression. Meta-analyses have confirmed that inflammatory markers including Il-1, Il-6, TNF alpha, and CRP are elevated in about 1/3 of depressed patients. However, Raison and Maletic made the point that anti-inflammatory medications are not for everyone. While patients with elevated levels of CRP at baseline responded to an anti–TNF alpha antibody, patients with low CRP values at baseline actually got worse.
Raison and Maletic cited three studies that have also linked CRP to differential response to traditional antidepressants. In unipolar depression, those with low CRP respond well to selective serotonin reuptake inhibitor (SSRI) antidepressants, while those with elevated blood levels of CRP seem to respond better to a dopamine-active antidepressant such as bupropion or a noradrenergic-active antidepressant such as nortriptyline or the serotonin norepinephrine reuptake inhibitor (SNRI) antidepressant duloxetine. Patients with high inflammation at baseline also seem to respond better to intravenous ketamine and oral doses of omega-3 fatty acids.
Studies of animals have suggested that inflammation throughout the body is implicated in depression. Studies in which rodents are repeatedly defeated by larger animals show that these animals have increased inflammation from lymphocites (a type of white blood cells) in the blood, and monocytes (another type of white blood cells) from the bone marrow and spleen. This inflammation can induce depression-like behaviors in the rodents, which is prevented if the inflammatory mechanisms are blocked. These data suggest that depression is not just in the brain—inflammation from all over the body plays an important role.
Read more
Inflammatory Marker CRP Higher in Bipolar Disorder, Particularly Mania
Inflammation has been linked to mood disorders. A 2016 meta-analysis in the journal Lancet Psychiatry described the role of inflammatory marker C-reactive protein (CRP) in bipolar episodes. Researchers led by Brisa S. Fernandes identified 27 studies that measured CRP levels in a total of 2,161 patients with bipolar disorder and 81,932 healthy participants. The researchers determined that compared to healthy controls, people with bipolar disorder have higher levels of CRP. CRP levels were moderately elevated between episodes and during depression, and substantially elevated during episodes of mania.
Editor’s Note: This meta-analysis shows that CRP is linked to bipolar disorder, and the inflammatory burden is highest during mania. It remains to be seen whether anti-inflammatory treatments work best in patients with high CRP levels compared to normal CRP levels.
CRP is also a risk factor for cardiovascular disease, and lithium and other treatments for bipolar disorder probably lower CRP levels.
The same group of researchers previously showed that statins, drugs typically used to lower cholesterol, could help alleviate depression. Since statins have anti-inflammatory effects, they can probably reduce depression risk in addition to lowering cardiovascular risk, as initial studies suggest.
Other drugs with anti-inflammatory effects that may improve depression include the anti-arthritis drug celecoxib and the antibiotic minocycline. The amino acid N-acetylcysteine and omega-3 fatty acids also have anti-inflammatory effects and have been found to improve depression in some studies.
Inflammation Predicts Depression and Anxiety Four Years Later in Older Americans
A large study of retired Americans found that those with high levels of the inflammatory marker C-reactive protein in the blood had more depression and anxiety. Higher CRP also predicted severity of depression and anxiety four years later.
The study, by researchers Joy E. Lin and Aoife O’Donovan, included 18,603 people over age 50 from the Health and Retirement Study. It was presented at the 2016 meeting of the Society of Biological Psychiatry.
Lin and O’Donovan hope that treating or preventing inflammation may be the key to preventing symptoms of depression and anxiety.
Meta-Analysis Shows Inflammation is Common in Unipolar Depression, Bipolar Depression, and Schizophrenia
In a symposium at the 2016 meeting of the Society of Biological Psychiatry, Mark Hyman Rapaport described the results of his research group’s meta-analysis of studies comparing levels of inflammation in the blood of people with unipolar depression, bipolar depression, and schizophrenia. Rapaport and colleagues determined that people acutely ill with any of the three illnesses showed abnormally high levels of certain inflammatory proteins. These included: interleukin-1beta, interleukin-6, TNF alpha, and c-reactive protein. Those who were chronically ill showed elevations in interleukin-6.
These data are consistent with increasing evidence that inflammation also occurs in the brain. Brain inflammation can be observed by measuring translocator protein binding, a measure of brain microglial activation, using positron emission tomography (PET) scans.