Combination of N-acetylcysteine and Risperidone Improves Irritability in Autistic Disorders More Than Placebo and Risperidone
In a 2013 study of 40 children and adolescents with autism spectrum disorders published by Ahmad Ghanizadeh and Ebrahim Moghimi-Sarani in the journal BMC Psychiatry, the combination of the over-the-counter nutritional supplement n-acetylcysteine (NAC) and the atypical antipsychotic risperidone alleviated irritability more than the combination of placebo and risperidone. Side effects were mild. The data extend 2012 observations by A.Y. Hardan et al. in which NAC improved irritability and stereotypy (repeated behavior) in autism more than placebo did.
The two studies taken together support the effectiveness of NAC prescribed either alone or in conjunction with an atypical antipsychotic for the treatment of autism.
Possible Heart Failure Risk with Pramipexole
We’ve written before about the drug pramipexole, which is typically used to treat Parkinson’s disease and restless legs, but can also improve depressed mood and cognition in those with bipolar disorder. The Federal Drug Administration (FDA) published a warning in 2012 that the drug may increase risk of heart failure, though more research is needed to confirm this link. In a review of existing studies, the FDA found that heart failure occurred more often in participants taking pramipexole than those taking placebo, but the finding did not reach statistical significance.
Acupuncture with Paroxetine Better Than Paroxetine Alone
In a six-week study published by S.S. Qu et al. in the Journal of Psychiatric Research in 2013, participants with depression who received manual or electrical acupuncture along with the selective serotonin reuptake inhibitor (SSRI) antidepressant paroxetine (Paxil) improved more than those participants taking paroxetine alone.
More patients taking paroxetine alone needed increased doses to deal with symptom aggravation.
Patients who had received electrical acupuncture continued to show improvement four weeks after the treatment ended.
Oral Scopolamine Promising for Depression
Intravenous scopolamine has shown promise as a rapid-acting antidepressant in studies by Carlos Zarate and colleagues at the National Institute of Mental Health (NIMH). Improvement on the drug can occur within 24 hours.
In a 6-week 2012 study, an oral preparation of scopolamine was more effective than placebo as an add-on medication to the selective serotonin reuptake intake (SSRI) antidepressant citalopram. Patients who received scopolamine and citalopram had higher rates of response and remission than those who received placebo and citalopram. The scopolamine group experienced more blurred vision and dizziness, which is to be expected from an anticholinergic drug, a drug that blocks the action of the neurotransmitter acetylcholine in the brain.
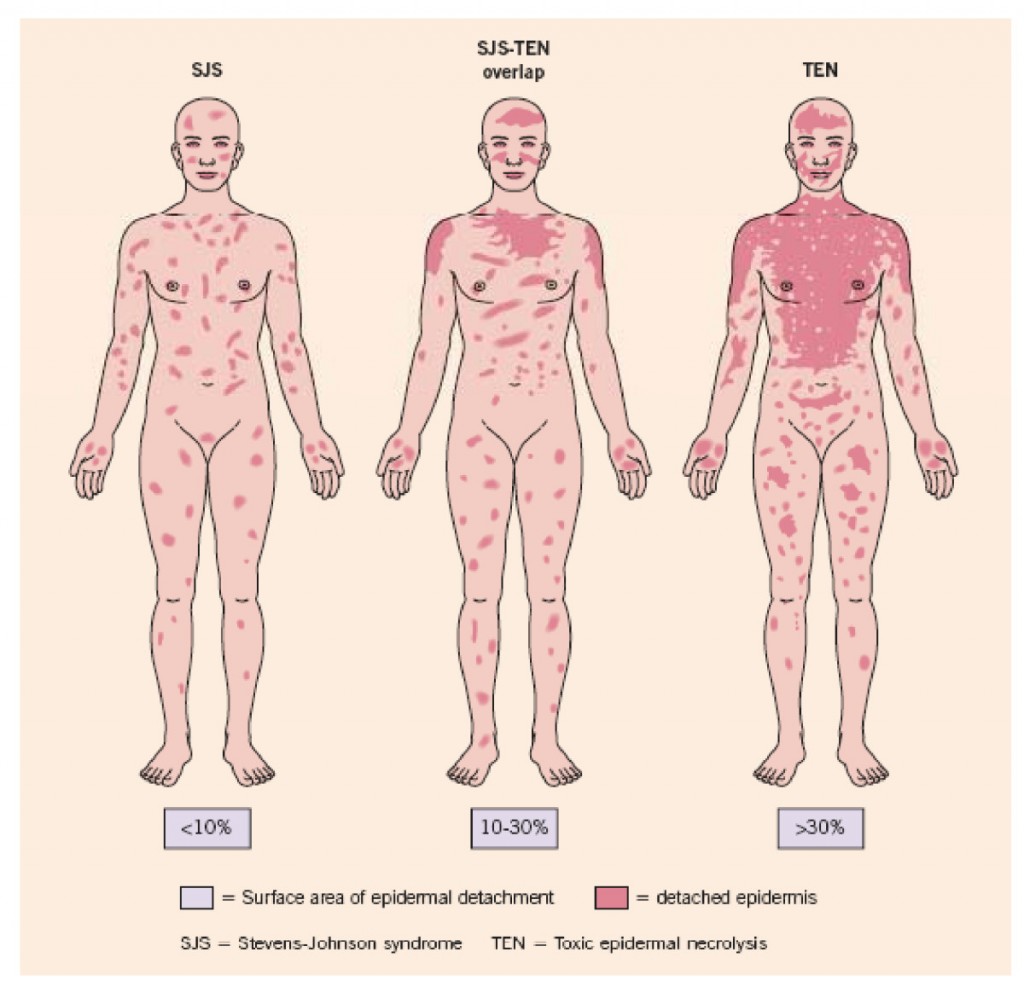
Genetic Test Predicts Risk of Severe Rash While Taking Carbamazepine
Carbamazepine (also known by its trade name Tegretol or, for extended release, Equetro) is one of the most widely used drugs for the treatment of epilepsy, and is relatively underutilized in the treatment of bipolar disorder. One of the reasons is fear of a rare serious rash or other side effects.
The risk of the serious rash ranges from about one in 5,000 to one in 10,000. Loss of white blood cells that fight infection (a condition called agranulocytosis) occurs in about one in 20,000 people taking carbamazepine, while a decrease in white blood cells, red blood cells, and platelets (aplastic anemia) occurs in about one in 100,000 patients.
There is no way of predicting who will develop the blood disorders in reaction to carbamazepine use. A patient should contact their doctor and get a white blood cell count if they develop some warning signs of these conditions, such as a fever or sore throat without other explanation or signs of bleeding or red spots under the skin (called petechiae) that could indicate low platelets.
Genetic Test for Risk of Rash
A genetic test is available that can help estimate the likelihood of the serious rash among certain populations. In those of Asian descent, particularly Han Chinese, Thai, Malaysian, and Indian populations, having a version of the gene HLA-B known as HLA-B*1502 is highly associated with developing the rash. (The odds ratio was 79.84 in a 2013 meta-analysis by Tangamornsuksan et al. in the journal JAMA Dermatology).
In those of northern European or Japanese descent, having a version of the gene HLA-A known as HLA-A*3101 is associated with the severe rash. (Odds ratio for developing the most severe rash was 25.93 in a study of Europeans published by McCormack et al. in the New England Journal of Medicine in 2011 and 10.8 in a study of Japanese published by Ozeki et al. in the journal Human Molecular Genetics in 2011). This HLA-A*3101 gene is present in about 2 to 5% of Europeans and 9% of Japanese.
A mild, non-serious rash with redness and itchiness occurs in about 5 to 10% of patients taking carbamazepine, and almost always goes away quickly upon stopping the drug. For patients taking carbamazepine who develop any rash, stopping the drug is the safest and most conservative thing to do. However, those who have taken the HLA test who know they do not have the risk genes and have only the benign rash might want to consider continuing to take the drug.
Benefits of Carbamazepine
There are a number of reasons why carbamazepine may be worthy of a treatment trial in patients with bipolar disorder who are not doing well on other agents. Carbamazepine works well in many patients with bipolar illness who have some of the common clinical predictors of a poor response to lithium. These include: having dysphoric (anxious, irritable) rather than euphoric mania, having an anxiety or substance disorder comorbidity, having had many prior episodes or rapid cycling (four or more episodes/year), not having distinct episodes with a period of wellness in between, having a sequential pattern of depression followed by mania followed by a well interval (D-M-I rather than M-D-I), having a schizoaffective disorder with delusions or hallucinations that persist after a manic or depressive episode has ended, and having no family history of mood disorders (especially bipolar disorder).
Some patients who do not respond to another anticonvulsant such as valproate do respond to carbamazepine. Patients with bipolar depression who have had a prior history of alcoholism may also do particularly well on carbamazepine. A benefit of the long-acting version of carbamazepine called Equetro is that it can be taken at bedtime and thus help with sleep and minimize daytime side effects.
Editor’s Note: Carbamazepine induces liver enzymes called CYP3A4 that increase the metabolism (breakdown) of carbamazepine and other drugs. Several drugs that inhibit 3A4 (such verapamil and erythromycin) prevent the breakdown of carbamazepine, causing blood levels of the drug to increase and produce side effects. If you are taking carbamazepine, tell your pharmacist so he or she can monitor any other drugs you are taking for potential interactions with carbamazepine.
Knowing about the rare skin and blood side effects of carbamazepine and some of the clinical predictors of a good response to the drug may be helpful in determining whether the potential benefits of carbamazepine outweigh the risks.
Biomarker Suggests Which Patients With Depression Respond to Cognitive Behavior Therapy Versus SSRI
Not every treatment for mood disorders works for every patient, and for the 60% of depressed patients whose first treatment is ineffective, this wrong guess can translate into months of suffering, wasted money, lost productivity, and risk of suicide. An important trend in treatment research is the search for biomarkers, that is, biological indicators that can predict which patients might be likely (or unlikely) to respond to a particular treatment. A 2013 study by McGrath et al. in the journal JAMA Psychiatry suggests that brain glucose metabolism is one such biomarker.
Patients with untreated major depressive disorder had their brain glucose metabolism measured and then were randomized to receive 12 weeks of treatment either with the SSRI antidepressant escitalopram oxalate (trade name Lexapro) or with cognitive behavior therapy. Low glucose metabolism in a part of the brain called the anterior insula (compared to the rest of the brain) predicted that patients would reach remission on cognitive behavior therapy and respond poorly to escitalopram, while high metabolism in the same area predicted the opposite, that patients would reach remission while taking escitalopram and respond poorly to cognitive behavior therapy.
Researchers will want to test this finding with patients over the long term, but the data from this study suggest that anterior insula glucose metabolism may be a successful biomarker that can guide initial treatment selection for patients with depression.
Micro-Nutrient Product Effective in Adult ADHD
EMPowerPlus is a nutritional supplement marketed by the company Truehope as a way of correcting nutritional deficiencies that contribute to depression, anxiety, bipolar disorder, and attention-deficit hyperactivity disorder (ADHD). In 2014 Rucklidge et al. published the first controlled study of EMPowerPlus in the British Journal of Psychiatry showing that the supplement was more effective than placebo in adults with untreated ADHD.
EMPowerplus contains 36 ingredients, including 14 vitamins, 16 minerals, 3 amino acids, and 3 antioxidants. Patients were randomized to receive either 15 EMPowerPlus pills per day or 15 placebos per day for 8 weeks, and those patients receiving the supplement were rated as more improved by the end of the study. Effect sizes were moderately robust and side effects did not differ.
Editor’s Note: Multiple uncontrolled studies have suggested the efficacy of EMPowerPlus in childhood mania and related conditions, but this is the first formal placebo-controlled study of the supplement in adults with ADHD. A study in children with ADHD is planned, but it would also be important to study this micronutrient formulation in childhood bipolar disorder, where there is some anecdotal evidence (from Charles Popper at McLean Hospital in Boston and Mary Fristad at the Ohio State University) of excellent responses in children with highly treatment-resistant bipolar illness.
Two Out of Three Studies of Armodafinil Have Failed in Bipolar Depression
At the US Psychiatric Congress in 2013, researcher T. Ketter reported on two recent studies of armodafinal (Neuvigil), which is approved for the treatment of narcolepsy. Doses of 150mg/day did not perform significantly better than placebo in the treatment of bipolar depression (in contrast to an earlier positive study).
Editor’s Note: It appears that this drug will not play a major role in the treatment of bipolar depression, as some had hoped.
Immune Response in Mania
While the reasons why one person develops bipolar disorder and another does not remain mysterious, the current thinking is that genes contribute some risk while immunological abnormalities contribute other risks. Researchers have identified certain antibodies whose levels spike during an episode of mania, as if the patient is having an immune reaction. These are referred to as biomarkers or inflammatory markers.
While various biomarkers for mania have been identified, until recently their effects had only been examined independently. A 2013 article by Dickerson et al. published in the journal PLOS ONE examined four biomarkers in combination. Each was a type of antibody: to the NR peptide of the NMDA receptor, to gliadin (a protein derived from gluten), to Toxoplasma gondii (a parasitic protozoan), and to Mason-Pfizer Monkey Virus. Measures of these four types of antibodies made up a combined inflammation score for participants in the study.
The study compared 57 patients presenting with a manic episode with 207 non-psychiatric controls and 330 patients who had had recent onset of psychosis, schizophrenia, or bipolar depression. The combined inflammation score of the mania group was significantly higher than the other groups at the time of hospital admission and at the time of evaluation several days later. It had returned to normal (i.e. not different from the other groups) at followup six months later, although those with the highest combined inflammation scores were at risk for re-hospitalization during that period.
The findings of this study suggest that hospitalization for mania is associated with immune activation, and the level of this activation predicts subsequent re-hospitalization. Treatments for mania that target this inflammatory response should be investigated.
Diabetes Drug Metformin May Impair Cognition, But Vitamin B12 May Help
Metformin, one of the most popular drugs to treat type 2 diabetes, interferes with uptake of vitamin B12, which can in turn lead to some neuronal dysfunction resulting in cognitive dysfunction. Several studies have sought to clarify this link, which may affect up to 30% of patients taking the drug.
Most recently, an Australian analysis of 1354 aging patients found that those with type 2 diabetes performed less well on tests of cognitive abilities, and those diabetic patients with low vitamin B12 levels (below 250 pmol/L) scored lower than those diabetic patients with adequate levels.
Because of the malabsorption problem caused by metformin, patients taking the drug may not be able to get enough B12 from a balanced diet alone and may need supplemental B12. Those who follow a vegetarian diet, have had bowel surgery, have certain complications with the stomach, or who take other medications that depress stomach acid may be at special risk.
Physicians should carefully monitor B12 levels in patients taking metformin, particularly those who have been taking the drug for more than 3 years or those who already suffer from some sort of cognitive impairment.