TDCS Effective in Bipolar Depression
 A 2017 study in the journal JAMA Psychiatry reports that transcranial direct current stimulation (tDCS) is an effective add-on treatment for bipolar depression. In the study by researcher Bernardo Sampaio-Junior and colleagues, 59 patients taking medication for bipolar disorder and experiencing a depressive episode were randomized to receive either 10 daily half-hour sessions of tDCS (and then one every two weeks) or an inactive sham stimulation.
A 2017 study in the journal JAMA Psychiatry reports that transcranial direct current stimulation (tDCS) is an effective add-on treatment for bipolar depression. In the study by researcher Bernardo Sampaio-Junior and colleagues, 59 patients taking medication for bipolar disorder and experiencing a depressive episode were randomized to receive either 10 daily half-hour sessions of tDCS (and then one every two weeks) or an inactive sham stimulation.
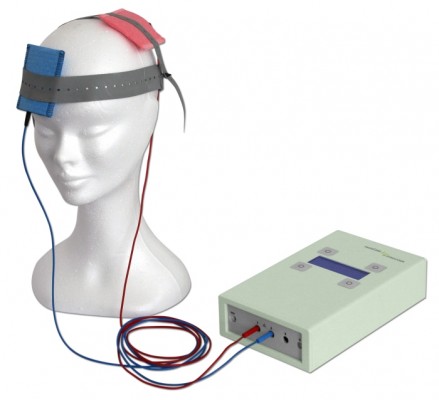
TDCS is a painless form of neurostimulation in which electrodes applied to the scalp provide a steady, low current of electricity that modulates neuron activity. Sampaio-Junior describes its low cost, portability and ease of use as some of its benefits. This is the first randomized, sham-controlled study of tDCS in bipolar disorder.
After six weeks of treatment, patients who received real tDCS treatment showed significantly more improvement in their depression than those who received the inactive sham stimulation. In the active group, 67.6% showed sustained response compared to 30.4% in the inactive group. TDCS was well tolerated, with skin redness at the application site the only side effect that was more common in the active group than in the sham group. Mood switching rates were similar across the two groups.
The research was completed as part of the Bipolar Depression Electrical Treatment Trial (BETTER) taking place in Brazil. The group of participants was 68% female with a mean age of 45.9 years. Sixty-one percent of participants had bipolar I disorder while the remainder had been diagnosed with bipolar II.
Continuing Lithium Treatment Does Not Increase Kidney Failure
 A risk of long-term lithium treatment is that it can cause kidney damage. However, a new study suggests that continuing lithium treatment after a diagnosis of chronic kidney disease does not necessarily increase the risk of irreversible end-stage kidney disease, which is defined as either the need for either chronic dialysis or a kidney transplant.
A risk of long-term lithium treatment is that it can cause kidney damage. However, a new study suggests that continuing lithium treatment after a diagnosis of chronic kidney disease does not necessarily increase the risk of irreversible end-stage kidney disease, which is defined as either the need for either chronic dialysis or a kidney transplant.
The 2017 study by researcher Lars Kessing and colleagues in the journal Acta Psychiatrica Scandinavica used Danish health databases to track data from all individuals who received a diagnosis of chronic kidney disease between 1995 and 2012 and also had a history of lithium treatment (754 patients) or anticonvulsant treatment (5,004 patients). Kessing and colleagues found that patients who continued taking lithium after an initial diagnosis of chronic kidney disease had decreased rates of end-stage kidney disease. This also held true for those who continued anticonvulsant treatment after a diagnosis of kidney disease.
One point of uncertainty was introduced by the finding that the subset of participants who were taking lithium specifically to treat bipolar disorder did have a higher rate of end-stage kidney disease. This was not true of the participants who were taking anticonvulsants to treat bipolar disorder.
Kessing and colleagues concluded that after an initial diagnosis of chronic kidney disease, continuing lithium did not necessarily increase end-stage kidney disease. Switching to an anticonvulsant, as is sometimes the practice after a kidney disease diagnosis, may not confer any benefit.
Lithium Treatment Lowers Suicide Rate in People with Bipolar Disorder
A large study that made use of a Swedish health database has shown that lithium reduces suicide rates in bipolar disorder. The study by researcher Jie Song and colleagues was published in the American Journal of Psychiatry in 2017.
The study included eight years of data from 51,535 people with bipolar disorder. During that time, there were 10,648 suicide-related events recorded, such as suicide attempts or completed suicides. The researchers compared suicide rates when patients were taking lithium to rates when they were off the drug, and found that lithium reduced attempted or completed suicide by 14%. Song and colleagues also looked at suicide rates for people taking valproate, and found that these were no better than when patients were off valproate, implying that treatment alone is not enough to reduce the suicide rate and the benefit is specific to lithium use.
Song and colleagues estimate that 12% of the suicide-related events among the patients included in the study might have been avoided if the patients had taken lithium for the entire study period. While there are other clinical considerations to make when selecting an appropriate treatment for a given patient, the researchers suggest that lithium treatment should be considered for patients with bipolar disorder who have expressed suicidal intentions or who are otherwise at risk for suicide.
In Danish Study, Higher Trace Levels of Lithium in Drinking Water in Certain Regions Do Not Seem to Prevent Bipolar Disorder
Previous studies have found that trace levels of lithium that occur naturally in the drinking water of certain regions are associated with lower rates suicide. Preliminary studies have also shown that lithium in drinking water is associated with lower dementia rates. The trace levels seen in drinking water are many hundreds of times lower than clinical doses of lithium prescribed for bipolar disorder, but they vary greatly according to locality.
A new study by researcher Lars Kessing and colleagues investigated whether chronic exposure to lithium in drinking water might protect against bipolar disorder, but found no evidence that this is the case in Denmark.
In an article published in the journal Bipolar Disorders in 2017, Kessing and colleagues describe findings from their analysis of data on 14,820 patients with a diagnosis of mania or bipolar disorder and (for each participant with bipolar disorder) 10 other age- and gender-matched control participants totaling 140,311. The researchers were able to look longitudinally at the participants’ exposure to trace levels of lithium in drinking water based on their municipalities of residence.
The investigators hoped to find evidence that greater exposure to lithium was associated with lower rates of bipolar disorder. Kessing and colleagues concluded that trace lithium levels higher than those in Denmark might be needed to find such a result.
Editor’s Note: Clinical studies of lithium treatment for children at high risk for bipolar disorder could help clarify whether even conventional therapeutic levels of lithium could reduce or delay the appearance of bipolar disorder.
Naturally Occurring Lithium in Texas Drinking Water Reduced Alzheimer’s Mortality Rates
Several studies have found that trace levels of lithium that naturally occur in the drinking water of certain regions are associated with reductions in dementia compared to regions with less lithium in the water. The latest such study found that higher trace levels of lithium in certain Texas counties were associated with less mortality from Alzheimer’s disease compared to Texas counties with lower levels of lithium in the water.
The research by Val Andrew Fajardo and colleagues was published in the Journal of Alzheimer’s Disease in 2017. Fajardo’s team obtained 6,180 water samples from 234 of Texas’ 254 counties. They also calculated that there was an increase in the Alzheimer’s mortality rate from the period 2000–2006 to the period 2009–2015. However, regions with higher trace levels of lithium were negatively correlated with this increase, suggesting that the lithium in the water had a protective effect on people in those counties.
The researchers controlled for gender, race, education, rural living, and air pollution. Physical inactivity, obesity, and type 2 diabetes seemed to be confounding factors. Obesity and type 2 diabetes were positively correlated with Alzheimer’s mortality and negatively correlated with lithium levels in drinking water, meaning that it is possible that lithium also protects against these conditions.
Lithium in Drinking Water May Reduce Dementia
New research suggests that higher trace levels of lithium in drinking water can reduce dementia rates in the general population. In a 2017 article in the Archives of General Psychiatry, researcher Lars Kessing and colleagues compared data on 73,731 patients in Denmark with a diagnosis of dementia to 733,653 control participants without this diagnosis between the years 1970 and 2013. They were able to match the data to recorded levels of trace lithium in the drinking water in participants’ municipalities of residence.
Lithium levels in the water ranged from 0.6 micrograms per liter to 30.7 micrograms per liter in 151 different locations throughout Denmark. Compared to those exposed to 2.0 to 5.0 micrograms of lithium per liter of water, those exposed to more than 15.0 micrograms per liter had a lower incidence rate of dementia. However, those exposed to 5.1 to 10.0 micrograms per liter had a higher incidence of dementia. The same relationship was also found between lithium exposure levels and both Alzheimer’s disease and vascular dementia.
The lithium levels in the water were approximately 10,000 to 300 times lower than typical clinical doses (typically 900–1500mg/day, which produce concentrations ranging from 0.6 to 1.2 meq/L in patients’ blood). The minute exposures to lithium in the drinking water occurred over decades in the Danish study, and suggest that there may be long-term positive effects to chronic lifetime exposure to very low lithium levels.
These data follow others regarding exposure to trace lithium. In 2011, researcher Orestes V. Forlenza and colleagues reported in the British Journal of Psychiatry that low dose lithium (150–600mg/day) over a period of one year decreased the progression of mild cognitive impairment compared to placebo, while researcher Marielza Andrade Nunes and colleagues reported in the journal Current Alzheimer’s Research in 2013 that an even smaller dose (0.3mg/day) over a period of 15 months slowed the progression of Alzheimer’s dementia. Thus, low or microscopic doses consumed over long periods could slow cognitive deterioration.
Depression and Suicidal Thoughts Linked to Brain Inflammation
A 2017 article by Sophie E. Holmes and colleagues in the journal Biological Psychiatry reports that people with major unipolar depression, especially those with suicidal thoughts, have higher levels of the inflammatory marker translocator protein than do healthy individuals.
The participants with depression and suicidal thinking had high levels of translocator protein in the anterior cingulate cortex, which suggests that inflammation is affecting microglia.
Many studies have found links between different indicators of inflammation and mood disorders, leading researchers to speculate whether targeting the immune system could be an effective way to treat mood disorders. Patients with high levels of inflammation often fail to respond to typical treatments for depression.
Some previous research has found evidence of microglial activation in the brains of people who died from suicide.
The small study by Holmes and colleagues used positron-emission tomography, or PET scans, to observe evidence of translocator protein levels in the brain in 14 medication-free participants in a major depressive episode and 13 healthy volunteers. Those with depression, and particularly those with suicidal thoughts, showed more evidence of neuroinflammation.
Link Clarified Between Gut Microbes and Emotions
A 2017 article in the journal Microbiome suggests that gene-regulating molecules called microRNAs in the brain may be the link between microbes in the gut and emotions.
The research by Alan E. Hoban and colleagues looked at mice raised in a sterile, microbe-free environment. These mice had fewer anxiety-like behaviors than mice raised among the usual bacteria, viruses, and fungi. This finding implies that the microbiome—the trillions of microbes that live in and around our bodies—affects brain functions. In this case, the affected regions were the prefrontal cortex and the amygdala, which both play a role in the detection and response to fearful stimuli. These regions showed alterations in the level of microRNAs present.
When Hoban and colleagues introduced microbes into the animal’s systems, some microRNAs did not bounce back, suggesting that there may be a crucial window early in life when the presence of microbes is needed for the brain to develop normally.
In general, this research shows that microRNAs are key to understanding the link between the microbiome and the brain.
Exercise May Protect Against Breast Cancer
 Epidemiological evidence suggests that exercise reduces breast cancer rates and rates of breast cancer recurrence. However, it is not well understood why this is true.
Epidemiological evidence suggests that exercise reduces breast cancer rates and rates of breast cancer recurrence. However, it is not well understood why this is true.
Exercise that is intense enough to increase the heartrate and induce heavy breathing can increase the hormone epinephrine in the blood. A 2017 article by researcher Christine Dethlefson and colleagues in the journal Cancer Research reported that this elevated level of epinephrine in the blood of breast cancer patients after one intense exercise session stopped their breast cancer cells from growing in vitro and reduced tumor growth by half.
Senior author Pernille Hojman told Reuters that while exercise could not be expected to replace anti-cancer treatments, it is a great supportive strategy that has the added benefits of increasing patients’ quality of life and sense of empowerment.
The study looked at human breast cancer tumor cells in test tubes, and the same type of tumor cells implanted into mice. Only 45 percent of the mice implanted with the cancer cells collected after vigorous exercise developed tumors, compared to 90 percent of the mice who received cancer cells collected before exercise or with no exercise.
Exercise May Improve Memory
 A recent study suggests that exercising vigorously 20 minutes per day may improve “interference memory,” a type of memory that involves reconciling new learning with information one already knows. (Sometimes older information “interferes” with new learning.) In a 2017 article in the Journal of Cognitive Neuroscience, researcher Jennifer Heisz and colleagues report that performance on a high-interference memory task improved when participants engaged in 20-minute daily sessions of interval training for six weeks.
A recent study suggests that exercising vigorously 20 minutes per day may improve “interference memory,” a type of memory that involves reconciling new learning with information one already knows. (Sometimes older information “interferes” with new learning.) In a 2017 article in the Journal of Cognitive Neuroscience, researcher Jennifer Heisz and colleagues report that performance on a high-interference memory task improved when participants engaged in 20-minute daily sessions of interval training for six weeks.
Heisz and colleagues compared three groups of students: one did interval training, another did both interval training and cognitive training, and a control group did no special training. Both exercise groups performed better on the high-interference memory task than the control group. Those who exercised also had higher levels of brain-derived neurotrophic factor (BDNF), which promotes the growth of new synapses and is crucial for long-term memory.
The researchers suggest that this finding could be useful to seniors facing memory deficits, since only six weeks of exercise improved memory performance. Interference memory tends to decline with age.
Previous research has linked aerobic exercise to better academic performance.







