Clozapine-Induced Myocarditis More Common Than Thought
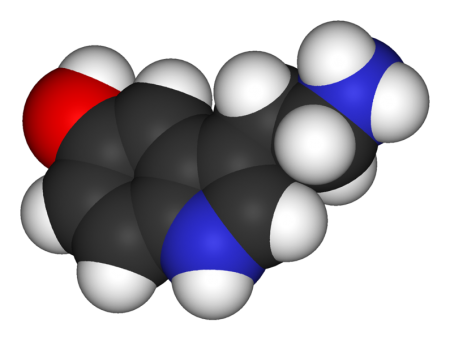
 New research indicates that myocarditis, inflammation of the middle layer of the heart wall, occurs in about 3% of patients who begin taking clozapine (Clozaril). Researcher Kathlyn J. Ronaldson and colleagues recently published research to this effect in the journal Acta Psychiatrica Scandinavica. Many cases of myocarditis, which can be fatal, begin with fever. Other symptoms include rapid or abnormal heart rhythms, shortness of breath, fluid retention, and fatigue. Because the illness resembles a viral infection, it may be misdiagnosed.
New research indicates that myocarditis, inflammation of the middle layer of the heart wall, occurs in about 3% of patients who begin taking clozapine (Clozaril). Researcher Kathlyn J. Ronaldson and colleagues recently published research to this effect in the journal Acta Psychiatrica Scandinavica. Many cases of myocarditis, which can be fatal, begin with fever. Other symptoms include rapid or abnormal heart rhythms, shortness of breath, fluid retention, and fatigue. Because the illness resembles a viral infection, it may be misdiagnosed.
In 2010 Ronaldson and colleagues reported in the Journal of Clinical Psychiatry that tachycardia (rapid resting heart rate) and elevated levels of a group of proteins knows as troponin in the blood are almost always present during the first 45 days of treatment in patients who develop myocarditis. The researchers found that the time to onset of myocarditis was 14 to 22 days in almost all cases. Eosinophilia (high levels of a certain type of white blood cell) may occur in the week after peak troponin levels, and high levels of the inflammatory protein CRP (above 100mg/L) occurred in 79% of cases.
Ronaldson and colleagues suggest that patients who are prescribed clozapine be monitored for myocarditis during the first four weeks of treatment, particularly during the third week.
Genetic Variation Predicts Which Type of Antidepressant Will Be Effective
 In a six-month study of Caucasian patients, normal variations in the gene that is responsible for brain-derived neurotrophic factor (BDNF) predicted whether patients would respond better to a selective serotonin reuptake inhibitor (SSRI) antidepressant versus a serotonin and norepinephrine reuptake inhibitor (SNRI) or a tricycle antidepressant. There are several common variants of the BDNF gene, depending on which types of amino acids appear in its coding—valine or methionine. Patients with the most common version, two valines (or Val66Val), responded better to SSRIs. About two-thirds of the population has this version of the gene, which functions most efficiently. The remaining third have at least one methionine in the BDNF gene. Patients with a Met variation responded better to SNRIs and tricyclic antidepressants.
In a six-month study of Caucasian patients, normal variations in the gene that is responsible for brain-derived neurotrophic factor (BDNF) predicted whether patients would respond better to a selective serotonin reuptake inhibitor (SSRI) antidepressant versus a serotonin and norepinephrine reuptake inhibitor (SNRI) or a tricycle antidepressant. There are several common variants of the BDNF gene, depending on which types of amino acids appear in its coding—valine or methionine. Patients with the most common version, two valines (or Val66Val), responded better to SSRIs. About two-thirds of the population has this version of the gene, which functions most efficiently. The remaining third have at least one methionine in the BDNF gene. Patients with a Met variation responded better to SNRIs and tricyclic antidepressants.
The study by R. Colle and colleagues was published in the Journal of Affective Disorders in 2015. Of the patients who were prescribed SSRIs, 68.1% of patients with the Val/Val version responded to the medication after three months, compared to 44% of the patients with a Met version. Of patients prescribed SNRIs or tricyclics, 60.9% of the Met patients reached remission by six months, compared to only 33.3% of the Val/Val patients.
Editor’s Note: In an earlier BNN we reported that according to research published by Gonzalo Laje and colleagues in the journal Biological Psychiatry in 2012, depressed patients with the better functioning Val66Val allele of BDNF respond best to ketamine, while those with the intermediate functioning Val66Met allele respond less well.
More Evidence N-Acetylcysteine Added to Risperidone Improves Irritability in Autism
We reported in 2014 that researchers Ahmad Ghanizadeh and Ebrahim Moghimi-Sarani had found that the over-the-counter nutritional supplement n-acetylcysteine (NAC) added to the atypical antipsychotic risperidone reduced irritability in autism more than placebo added to risperidone.
A randomized, double-blind, placebo-controlled clinical trial published by M. Nikoo and colleagues in Clinical Neuropharmacology in 2015 replicated these results. Forty children with autism disorders aged 4–12 years were randomized to receive either risperidone plus NAC or risperidone plus placebo. Risperidone doses were between 1 and 2 mg/day, and NAC doses were 600 to 900 mg/day. By the end of the 10-week study, those children who received NAC had significantly greater reductions in irritability and hyperactivity/noncompliance than those who received placebo.
Editor’s Note: Three placebo-controlled studies have supported the efficacy of NAC in autism. One 2012 study, by A.Y. Hardan in Biological Psychiatry, evaluated monotherapy with oral NAC. In the other two, NAC was added to treatment with risperidone.
Inability to Balance on One Leg May Indicate Stroke Risk
A balance test may indicate declining cognitive health and risk for stroke. Researchers led by Yasuharu Tabara had previously found that balancing on one leg became more difficult for people with age. Now the same team has found that this type of postural instability is associated with decreases in cognitive functioning and with risk of stroke. Fourteen hundred participants with an average age of 67 were challenged to balance on one leg for up to 60 seconds. They also completed computer surveys, magnetic resonance imaging (MRI) scans, and a procedure to measure the thickness of their carotid artery. Those who could not balance on one leg for 20 seconds or longer were more likely to have cerebral small vessel disease.
Editor’s Note: Whether exercise would reverse this vulnerability remains to be seen, but lots of other data suggest the benefit of regular (even light) exercise on general health.
No Evidence Chelation Therapy Can Treat Autism
Some children with autism have been subjected to chelation therapy, which is used to remove heavy metals from the blood after poisoning. The rationale for using this therapy in autism was the discredited theory that autism resulted from mercury poisoning. A recent review of research on chelation therapy for autism by the Cochrane Collaboration, a nonprofit health research organization, found only one randomized controlled trial of chelation therapy, which had a flawed methodology and also found no evidence of a reduction in autism symptoms. This means there is no evidence that chelation therapy, which can lead to kidney failure or death, has any effect on autism symptoms. Based on the lack of evidence that the therapy has benefits for children with autism spectrum disorders, its great expense, and the dangers it poses, chelation therapy should not be prescribed as a treatment for autism.
Deep Transcranial Magnetic Stimulation Safe and Effective in Major Depression
Repeated transcranial magnetic stimulation is a non-invasive procedure that has been approved for the treatment of severe depression since 2008. In rTMS treatment, a figure-8–shaped electromagnetic coil is placed against the forehead and magnetic pulses that can penetrate the scalp are converted into small electrical currents that stimulate neurons in the brain up to 1.5 cm deep. More recently, in 2013, the Federal Drug Administration approved a device with an H-shaped coil that delivers deep transcranial magnetic stimulation (dTMS). It can stimulate a wider area, and up to 8 cm deep.
Y. Levkovitz and colleagues have published the first double-blind randomized controlled multicenter trial of dTMS, reporting in the journal World Psychiatry that the intervention was effective and safe in patients who had not responded to antidepressant medication.
The study included 212 patients aged 22–68 years. All participants had failed to respond to one to four antidepressants or had not been able to tolerate the side effects of at least two antidepressants during their current episode of depression. The patients were randomized to receive either a sham treatment or 18 Hz dTMS over the prefrontal cortex acutely for four weeks and biweekly for 12 weeks for a total of 20 sessions.
The patients who received dTMS showed significantly greater improvement in symptoms than those who received the sham treatment, with a moderately large effect size of 0.76. Response and remission rates were also better in those who received dTMS. Response rates were 38.4% for the dTMS group versus 21.4% in the sham group. Remission rates were 32.6% for the dTMS group and 14.6% for the sham group. These difference in response remained stable during the three months of the study.
Side effects were minor except for a seizure that occurred when the protocol for the treatment was breached.
Inflammation Can Differentiate Apathy From Depression in Older Patients
In a new study by ESM Eurelings and colleague in the journal International Psychogeriatrics, the inflammatory marker C-reactive protein differentiated between older people with symptoms of apathy versus symptoms of depression. Higher levels of C-reactive protein were found in those with symptoms of apathy. The researchers concluded that apathy may be a manifestation of mild inflammation in elderly people.
Serotonin 5-HT7 Receptors: Why Should We Care About Them?
5-HT7 is a type of receptor activated by the neurotransmitter serotonin. Some of the most potent effects of lurasidone (Latuda), an atypical antipsychotic with antidepressant effects in bipolar depression, and vortioxetine (Brintellix), a unique antidepressant for unipolar depression that also has positive effects on cognition, occur through the blockade of 5-HT7 receptors. The atypical antipsychotics aripiprazole and sulpiride also act on 5-HT7 receptors.
Researcher Agnieszka Nikiforuk summarized the research to date on 5-HT7 receptors in the journal CNS Drugs in 2015.
The receptors play a role in regulating sleep and circadian rhythms, which may explain why drugs that target them can be helpful in depression. Drugs that target 5-HT7 receptors have also improved learning and memory.
One subject of research into 5-HT7 receptors is whether better results come from blocking the receptors or stimulating them.
Blockade of 5-HT7 receptors has improved depression-like symptoms in animals and enhances the effects of sub-therapeutic doses of antidepressants. In other animal studies, stimulation of the receptors has appeared promising for the prevention of age-related cognitive decline.
More Evidence Vortioxetine Improves Depression and Cognitive Function
 Vortioxetine (Brintellix) is a relatively new antidepressant that has a range of effects on serotonin receptors, making it different from selective serotonin reuptake inhibitors (SSRIs), which work only on the serotonin transporter. In multiple studies, it has treated not only depression but also cognitive dysfunction. In a new study led by Atul Mahableshwarkar and published in the journal Neuropsychopharmacology, 10–20 mg/day of vortioxetine reduced symptoms of depression more than placebo and improved performance on tests of cognitive ability more than placebo and another antidepressant, duloxetine.
Vortioxetine (Brintellix) is a relatively new antidepressant that has a range of effects on serotonin receptors, making it different from selective serotonin reuptake inhibitors (SSRIs), which work only on the serotonin transporter. In multiple studies, it has treated not only depression but also cognitive dysfunction. In a new study led by Atul Mahableshwarkar and published in the journal Neuropsychopharmacology, 10–20 mg/day of vortioxetine reduced symptoms of depression more than placebo and improved performance on tests of cognitive ability more than placebo and another antidepressant, duloxetine.
While depression is often accompanied by cognitive dysfunction, in this study vortioxetine seemed to directly treat the cognitive deficits rather than reducing them by alleviating the depression. The participants were aged 18–65.
Mental Illness Associated with 10 Years Lost Life Expectancy
Severe mental illness is one of the leading causes of death worldwide. Recently researchers led by E.R. Walker performed a meta-analysis of all cohort studies comparing people with mental illness to non-ill populations. They used five databases to find 203 eligible studies from 29 countries. Their findings, published in the journal JAMA Psychiatry in 2015, show that people with mental illness have a mortality rate 2.22 times higher than people without mental illness. People with mental illness lose a potential 10 years of life compared to those without severe mental disorders. The researchers estimated that 14.3% of deaths worldwide are attributable to mental illness.
Editor’s Note: Comorbid cardiovascular illness accounts for a large part of the disparity in life expectancy between people with and without mental illness. Those at risk for serious mental illness should pay close attention to their cardiovascular as well as psychiatric risk factors.