RTMS May Treat Cocaine Addictions
 In a pilot study, repeated transcranial magnetic stimulation (rTMS) reduced cocaine cravings and usage among people with cocaine addiction.
In a pilot study, repeated transcranial magnetic stimulation (rTMS) reduced cocaine cravings and usage among people with cocaine addiction.
RTMS is a non-invasive treatment in which a magnetic coil placed near the skull transmits electrical signals to the brain. It is an effective treatment for depression, and there is growing evidence that it may also be able to treat addictions.
Participants in the pilot study by researcher Antonello Bonci and colleagues received rTMS directed at their dorsolateral prefrontal cortex or pharmacological treatments (including medications to manage depression, anxiety, and sleep problems) over a 29-day study period. Among the rTMS recipients, 69% remained cocaine-free during the study period, compared to only 19% of those treated with medications. Those who received rTMS also reported fewer cravings.
There were few side effects among those who received rTMS, and there was a 100% compliance rate among the 32 participants, meaning they all showed up for each of their sessions.
Bonci and colleagues are working on a larger study that will compare rTMS treatment to a sham procedure rather than to a medication regime.
Diabetes Drug Pioglitazone May Improve Depression
 Researchers believe there is a link between diabetes and depression. Some drugs used to treat type II diabetes and its associated inflammatory symptoms have been found to improve depression as well. These include metformin, rosiglitazone, and pioglitazone. A recent study by Natalie Rasgon and colleagues explored the effects of pioglitazone treatment on people with insulin resistance, insulin sensitivity and/or pre-diabetes and ongoing depression. The researchers hoped to find that adding pioglitazone to the patients’ regular antidepressant regimen might improve depression by reducing inflammation.
Researchers believe there is a link between diabetes and depression. Some drugs used to treat type II diabetes and its associated inflammatory symptoms have been found to improve depression as well. These include metformin, rosiglitazone, and pioglitazone. A recent study by Natalie Rasgon and colleagues explored the effects of pioglitazone treatment on people with insulin resistance, insulin sensitivity and/or pre-diabetes and ongoing depression. The researchers hoped to find that adding pioglitazone to the patients’ regular antidepressant regimen might improve depression by reducing inflammation.
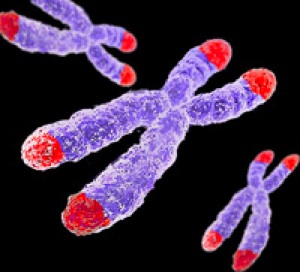
The study also touched on the role of telomere length in mental and metabolic disorders. Telomeres are repeated DNA sequences that sit at the end of chromosomes and protect them during cell replication. Telomeres get shorter with aging and with psychiatric illnesses. In the study, telomere length was used to predict whether patients’ depression would improve.
Rasgon and colleagues found that in those patients taking both pioglitazone and antidepressant treatments (compared to those who received a placebo in addition to their antidepressants), longer telomeres predicted better antidepressant response. This suggests that telomere length could be used as a biomarker—that is, measuring a patient’s telomere length could reveal whether that patient’s depression is likely to respond to an anti-inflammatory treatment such as pioglitazone. The research was presented at a 2015 scientific meeting.
In Rats, Dad’s Cocaine Use Affects Son’s Spatial Memory
Evidence is mounting that certain behaviors by parents can leave marks on their sperm or eggs that are passed on to their offspring in a process called epigenetics. In a recent study by researcher Mathieu Wimmer and colleagues, male rats that were exposed to cocaine for 60 days (the time it takes for sperm to develop fully) had male offspring who showed diminished short- and long-term spatial memory compared to the offspring of male rats that were not exposed to cocaine. Female offspring were not affected in this way.
The spatial tasks the offspring rats completed depended heavily on the hippocampus. Wimmer and colleagues believe that cocaine use in the fathers decreased the amount of a brain chemical called d-serine in the offspring. D-serine plays a role in memory formation and the brain’s ability to form synaptic connections. Injecting the offspring of rats who were exposed to cocaine with d-serine before the spatial memory tasks normalized the rats’ performance.
Yoga Therapy Improves Depression and Inflammation
Drug treatment for major depression can produce remission in 35–50% or patients. The others may need additional interventions, and some mind-body techniques have been successful. A recent randomized study by Anup Sharma and colleagues found that Sudarshan Kriya Yoga (SKY) decreased depression at one and two months when added to participants’ regular treatments. Participants who received the yoga treatment also showed reductions in inflammation in the blood, including lower levels of the inflammatory proteins TNF-alpha, IL-10, and CRP.
Cognitive Behavioral Therapy Improves Depression, PTSD by Improving Brain Connectivity
A recent study clarified how cognitive behavioral therapy improves symptoms of depression and post-traumatic stress disorder (PTSD). The participants were 62 adult women. One group had depression, one had PTSD, and the third was made up of healthy volunteers. None were taking medication at the time of the study. The researchers, led by Yvette Shelive, used functional magnetic resonance imaging (fMRI) to analyze participants’ amygdala connectivity.
At the start of the study, participants with depression or PTSD showed diminished connectivity between the amygdala and brain areas related to cognitive control, the process by which the brain can vary behavior and how it processes information in the moment based on current goals. The lack of connectivity reflected the severity of the participants’ depression. Twelve weeks of cognitive behavioral therapy improved mood and connectivity between the amygdala and these control regions, including the dorsolateral prefrontal cortex and the inferior frontal cortex. These regions also allow for executive functioning, which includes planning, implementation, and focus.
Mindfulness Therapy Improves Anxiety in Youth with a Bipolar Parent
Children of parents with bipolar disorder are prone to anxiety and emotional dysregulation, but treating these symptoms with antidepressants can provoke symptoms of mania. Thus, non-pharmacological treatements for anxiety and depression are needed. A recent study by Melissa DelBello found that twelve weeks of mindfulness-based cognitive therapy improved symptoms of anxiety and mood dysregulation in 20 youth with a bipolar parent. DelBello used functional magnetic resonance imaging (fMRI) to observe that the therapy increased activation of brain structures related to emotion and sensing. Amygdala activation differed between those with anxiety and those with mood dysregulation, suggesting that the therapy’s effect was on regions that modulate the amygdala, including prefrontal and insular regions, rather than on the amygdala itself.
Anti-Inflammatory Treatments Look Promising for Bipolar Depression
Inflammation has been linked to both unipolar and bipolar depression. New research shows that anti-inflammatory treatments may reduce bipolar depression, for which few treatments exist.
Researchers led by Jonathan Savitz divided people with bipolar depression into four groups. One group received two placebos, another received minocycline (a drug with neuroprotective and immune-modulating properties) plus a placebo, the third received aspirin plus a placebo, and the final group received both minocycline and aspirin. Of the 64 participants, those who took both minocycline and aspirin were most likely to respond to treatment and to enter remission. In people with body mass indexes (BMIs) above the median of 30, a sign of greater inflammation, 100% of those who received both anti-inflammatory drugs responded to treatment, compared to 36% of those who received aspirin alone, 33% of those who received minocycline alone, and 25% of those who received two placebos.
Dosages of the drugs were 100mg twice a day for minocycline and 81mg twice a day for aspirin. Savitz and colleagues believe that aspirin and minocycline must work particularly well together, and are modifying their study to more directly compare use of the two anti-inflammatory drugs together to the absence of anti-inflammatory treatments.






