Patients with Schizophrenia Have Short Telomeres, Atypical Antipsychotics Increased Telomere Length in Animals
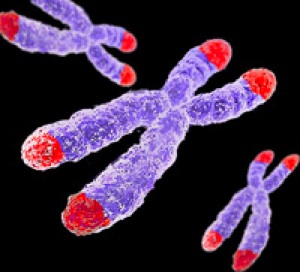 Telomeres sit at the end of DNA strands and shorten with each cell replication. A person’s percentage of short telomeres increases with aging. Telomeres also shorten with childhood adversity and as a function of number of depressive episodes.
Telomeres sit at the end of DNA strands and shorten with each cell replication. A person’s percentage of short telomeres increases with aging. Telomeres also shorten with childhood adversity and as a function of number of depressive episodes.
In a recent study, researcher Kazuya Torimi found that telomeres in white cells were shorter in 42 patients with schizophrenia compared to 56 healthy control participants.
Torimi also treated mice with various antipsychotics for 2-week periods. Treatment with atypical antipsychotics, such as risperidone, olanzapine and aripiprazole, but not typical antipsychotics like haloperidol, elongated telomere length in the hippocampus. This probably occurred through effects on serotonin.
Torimi suggests that atypical antipsychotics improve negative symptoms in part through the modulation of telomere length.
Editor’s Note: Lithium has been found to increase telomere length in patients with bipolar disorder, and appears to do this through a direct effect on telomerase, an enzyme responsible for adding to telomere length. Short telomeres are associated with a large number of medical and psychiatric illnesses.
Cariprazine for Mania Appears Safe and Well-Tolerated
At the 2014 meeting of the International College of Neuropsychopharmacology, researcher Lakshmi Latham presented a poster on three studies of the atypical atypical antipsychotic caripazine, a treatment that has not yet been approved by the Federal Drug Administration. We call it an atypical atypical because it is a partial agonist at dopamine D2 and D3 receptors, meaning it stimulates the receptors a little, but in the presence of high levels of dopamine it blocks excess activity by sitting on the receptor and preventing the actions of the excess dopamine. Aripiprazole is also a partial agonist at dopamine and serotonin 5HT1a receptors, but caripazine differs in that it has a particular affinity for the D3 receptor.
Previous analyses had revealed that cariprazine has good acute antimanic efficacy. All three studies described by Latham were randomized, double-blind, placebo-controlled three-week studies in patients with bipolar mania. In total the studies included 1065 patients, 442 of whom received placebo and 623 of whom received cariprazine.
Cariprazine doses from three studies were pooled, and ranged from 3-12 mg/day. Additional analyses evaluated the 3-6 and 9-12 mg/day groups specifically.
Approximately 70% of patients completed the study. The most common side effects included akathisia or restless legs (placebo, 5%; cariprazine, 20%), extrapyramidal disorder characterized by abnormal motor symptoms (5%, 13%), restlessness (2%, 6%) and vomiting (4%, 9%). The incidence of serious side effects was similar across the placebo and the treatment groups. Side effects that led to discontinuation of participation in the study occurred in 7% of placebo patients and 12% of cariprazine patients. Suicidal ideation was an infrequent side effect (placebo, 4; cariprazine, 2), and there were no suicide attempts.
Mean changes in weight were small (averaging 0.17kg in patients taking placebo and 0.54kg in those taking cariprazine), and the proportion of patients with 7% or higher increase in weight were similar across the two groups (both 2%). Mean changes in blood pressure and pulse were slightly greater with cariprazine and were related to dosage. Cariprazine was not associated with mean increases in electrocardiogram (EKG) parameters except for a slight increase in ventricular heart rate versus placebo (5.0 and 0.9 bpm, respectively). Mean changes in lipids and glucose were generally small and similar between groups. Levels of the hormone prolactin decreased in both groups.
Latham concluded that cariprazine treatment for three weeks was safe and well-tolerated.
Lithium Plus An Atypical Antipsychotic Was More Effective Than Valproate Plus An Atypical Antipsychotic In One Study, But Not Another
Evaristo Nieto et al. of Spain presented a poster about the naturalistic study of the efficacy of acute treatment of manic inpatients with lithium and valproate at the 2014 meeting of the International College of Neuropsychopharmacology. In the lithium group, all patients were treated with lithium and oral antipsychotics (N=85). In the valproate group, all were treated with valproate and oral antipsychotics (N=92). Outcome was measured using scores on scales for mania and for general functioning (the YMRS and the CGI-S). The atypical antipsychotic was typically olanzepine or risperidone.
Nieto et al. found that the mean change in CGI scores from baseline to the day of discharge was significantly higher in the lithium group (-2.84 versus -2.6), and concluded that, “Although it is used in more severe cases, treatment of manic inpatients with lithium associated with antipsychotics is more effective than treatment with valproate associated with antipsychotics.”
However, W.M. Bank et al. came to the opposite conclusion in a Korean study. Bank et al. “compared the 1-year rehospitalization rates of first-episode bipolar manic patients?who were discharged while being treated with lithium or valproate in combination with an?atypical antipsychotic….The rehospitalization rate was 17.3% during the 1-year follow-up period.”
Bank et al. found significantly higher rates of rehospitalization in the lithium (23.1%) compared to the?valproate (13.3%) group using the Kaplan-Meier formula for estimations.
Memory Tips for Bipolar Disorder
 Like cancer patients undergoing chemotherapy, patients with bipolar disorder often have memory problems, particularly if they have had many prior episodes. Some memory tips from CancerCare’s Chemobrain Information Series may also help patients with bipolar disorder remember things better and keep their memory sharp. Here are some of their tips:
Like cancer patients undergoing chemotherapy, patients with bipolar disorder often have memory problems, particularly if they have had many prior episodes. Some memory tips from CancerCare’s Chemobrain Information Series may also help patients with bipolar disorder remember things better and keep their memory sharp. Here are some of their tips:
Make lists. Carry a notepad with you, or use a smartphone to keep track of errands, shopping lists, daily tasks, and when you should take your medications.
Use a paper or electronic day planner or a personal organizer to keep track of appointments and special days like birthdays or anniversaries.
Use a wall calendar and hang it in a place that you will see it multiple times per day.
Carry a notebook and record everything you need to remember, including to-do lists; the dates, times, and addresses of appointments; important telephone numbers; and the names of people you meet and a brief description of them. You can also use the notebook to keep track of medical information: your medication schedule, any symptoms or side effects you are having, or questions to ask your doctor. You can also do this using an app like What’s My M3 or by downloading a personal mood charting calendar from our website.
Leave yourself a voicemail message to remember something important. When you listen to it later, write down the information.
Organize your home or office. Keep things in familiar places so you always know where to find them.
Avoid distractions. Find a quiet, uncluttered place to work or think where you can focus your attention for longer.
Have conversations in quiet places. This will help you concentrate better on what the other person is saying.
Repeat information aloud, and write down important points. If someone gives you information about an appointment, you might repeat the time, date, and location of the appointment out loud while righting it down.
Keep your mind active. You can use crossword puzzles, word or math games, or attend events about topics that interest you.
When writing, proofread. Double-check whether you’ve used the correct words and spellings.
Train yourself to focus through mindfulness. For example, if you keep misplacing your keys, pay extra attention each time you set down your keys. You may say aloud, “I’m putting my keys down on the counter.” Hearing the auditory cue can boost your memory.
Exercise, eat well, and get plenty of rest and sleep. These habits will help your memory work best.
Tell your loved ones that you are having memory problems, so that they’ll understand that you may forget things you may normally be able to remember. They can help you or encourage you.
Childhood adversity, epigenetics, and hippocampal volume
At the 2014 meeting of the International College of Neuropsychopharmacology, researcher Booij reported that in humans, there is an interaction between adversity experienced during childhood, and an epigenetic variation in the short form of the serotonin transporter (5HT-T ss, or SLC6A4), which can influence hippocampal volume during depression.
Epigenetics refers to environmental influences on the way genes are transcribed. The impact of life experiences such as stress is not registered in DNA sequences, but can influence the structure of DNA or tightness of its packaging. Early life experiences, particularly psychosocial stress, can lead to the accumulation of methyl groups on DNA (a process called methylation), which generally constricts DNA’s ability to start transcription (turning on) of genes and the synthesis of the proteins the genes encode. DNA is tightly wound around proteins called histones, which can also be methylated or acetylated based on events in the environment. When histones are acetylated, meaning that acetyl groups are attached to them, DNA is wound around them more loosely, facilitating gene transcription (i.e. the reading out of the DNA code into messenger RNA, which then arranges amino acids in order to construct proteins). Conversely, histone methylation usually tightens the winding of DNA and represses transcription.
Booij followed 33 children who had experienced some form of adversity at a young age until they were 15 or 16, examining methylation of the serotonin transporter in their T cells and monocytes compared to 36 children who had not experienced adversity during childhood. He found that in children who had experienced abuse in childhood, the degree of that abuse was correlated with methylation of the serotonin transporter and was inversely related to the volume of the hippocampus, as measured using magnetic resonance imaging (MRI). Thus, child abuse yields lasting epigenetic effects (methylation of the serotonin transporter) and has anatomical consequences in teenagers, as seen in smaller hippocampi. These data parallel converse findings by Joan Luby et al. published in the journal PNAS in 2012, in which increased maternal warmth directed toward a child aged 4-7 was associated with increased volume of the hippocampus several years later.
Korean Study of Mental Disorders in Children of Bipolar Parents
Korea, like the US, has a moderate incidence of childhood-onset bipolar disorder among children who are at high risk because they have a parent with bipolar disorder. In a recent study by Young-Sun Cho et al. presented at the 2014 meeting of the International College of Neuropsychopharmacology (CINP), 59 out of 100 children with a parent who had been diagnosed with bipolar disorder met the criteria for a mental disorder themselves.
Mood disorders were most common. Of the 59 children with mental disorders, 22 were diagnosed with bipolar disorder, and 16 were diagnosed with a depressive disorder. Others included four with attention deficit hyperactivity disorder (ADHD), four with an anxiety disorder, two with disruptive behavior disorders, one with a tic disorder, one with an autistic disorder, and one with schizophrenia and an anxiety disorder.
Editor’s Note: In contrast to studies in Germany, Switzerland, the Netherlands, and Canada, where few children are diagnosed with bipolar disorders (even among those who are at high risk because of a family history of bipolar disorder), 22% of high-risk children in Korea were diagnosed with bipolar disorder. This is comparable to or higher than rates at which high-risk children in the US are diagnosed with bipolar disorder. Studies from both the Bipolar Collaborative Network (in which this editor Robert Post is an investigator) and researcher Boris Birmaher et al. found that parents with bipolar disorder often had a variety of other disorders, such as anxiety, alcohol abuse, or substance abuse. These other illnesses also increase the risk of early-onset bipolar disorder in offspring, and this may account for the higher incidence of early-onset bipolar disorder among high-risk children in the US.
Folate Supplementation May Delay Onset of Depression in Those at High Risk
Low levels of folate, also known as folic acid or vitamin B9, have been associated with depressive symptoms in the general population. A 2014 article by A.L. Sharpley et al. in the Journal of Affective Disorders explored whether folate has protective effects. Teens and young adults (ages 14–24) at high risk for mood disorders due to a family history of these illnesses were randomly assigned to receive either folate supplements (2.5 mg daily) or placebo for up to three months. While there were no significant differences in the percentage of young people in each group who went on to be diagnosed with a mood disorder, in the folate group there was a delayed onset of illness in those who went on to become unwell.
FDA Warning About Antidepressants Followed by Drop in Use, and Increase in Suicide Attempts
A decade ago the Federal Drug Administration (FDA) released several warnings that children, adolescents (ages 10–17), and young adults (ages 18-29) taking antidepressants were at increased risk for suicidal ideation and behavior. A recent study found that following these warnings, antidepressant use among adolescents, young adults, and adults dropped, and psychotropic drug poisonings (a validated measure of suicide attempts) increased among adolescents and young adults. Numbers of completed suicides did not change for any age group.
The decision to place the warnings on antidepressant packaging was somewhat controversial because it was based on studies that were not necessarily designed to measure suicide risk. The relationship between depression, medication, and suicide is complicated. Medication can improve mood, but patients may seek out medication because of pre-existing suicidal thoughts, and the medication may not reduce these in young people.
The reduction in antidepressant use that occurred after the warnings was accompanied by a drop in depression diagnoses in children and adults. Studies have suggested that the decreases in antidepressant were not accompanied by increases in other treatments, such as psychotherapy or atypical antipsychotics, among young people. Increased monitoring of patients was called for in the FDA’s box warning, but did not take place.
The study of the aftermath of the FDA warnings, published by Christine Y. Lu et al. in a 2014 article in the journal BMJ, used data from 11 insurance networks throughout the US. The researchers used an interrupted time series study design, which is used to show whether a policy causes an abrupt change in the expected slope of study outcomes. Data covered the pre-warning period (first quarter of 2000 to third quarter of 2003), the warning “phase-in” period (last quarter of 2003 to last quarter of 2004) and the post-warning period (first quarter of 2005 to last quarter of 2010). The study cohorts included around 1.1 million adolescents, 1.4 million young adults, and 5 millions adults per quarter.
Among adolescents, the previously upward trend in antidepressant use declined by 31.0% in the second year after the warnings, and psychotropic drug poisonings increased by 21.7% (a figure that was statistically significant for males). Poisonings by any drug increased by 13.9% in the second year after the warnings. After 2008, the downward trend in antidepressant use reversed, indicating that either the initial effects of the warning had worn off or that modifications to the warnings in May 2007, which encouraged patients and doctors to consider the risk of antidepressants alongside the risk of leaving mood disorders untreated, led to increased use.
Among young adults, the upward trend in antidepressant use declined by 24.3% in the second year after the warnings, and psychotropic drug poisonings increased by 33.7%, a statistically significant change for both male and female patients.
Among adults, to whom the warnings were not directed, antidepressant use decreased by 14.5% in the second year after the warnings.
The study by Yu et al. is the first to show that suicide attempts actually increased after the FDA warnings. The authors suggest that the increase in suicide attempts might be a consequence of undertreating mood disorders, since antidepressant use dropped simultaneously. The warnings and related media attention may have led to these unintended consequences, since media reports can sometimes be oversimplified.
Clarifying the role of melatonin receptors in sleep
The antidepressant agomelatine (which is available in many countries, but not the US) and the anti-insomnia drug ramelteon (Rozerem) both act as agonists at melatonin M1 and M2 receptors. New research is clarifying the role of these receptors in sleep.
In new research from Stefano Comai et al., mice who were genetically altered to have no M1 receptor (MT1KO knockout mice) showed a decrease in rapid eye movement (REM) sleep, which is linked to dreaming, and an increase in slow wave sleep. Mice who were missing the M2 receptor (MT2KO knockout mice) showed a decrease in slow wave sleep. The effects of knocking out a particular gene like M1 or M2 end up being opposite to the effect of stimulating the corresponding receptor.
The researchers concluded that MT1 receptors are responsible for REM sleep (increasing it while decreasing slow wave sleep), and MT2 receptors are responsible for slow wave non-REM sleep.
The new information about these melatonin receptors may explain why oral melatonin supplements can make a patient fall asleep faster, but do not affect the duration of non-REM sleep. The authors suggest that targeting MT2 receptors could lead to longer sleep by increasing slow wave sleep, potentially helping patients with insomnia.
Diabetes May Contribute to Low Hippocampal Volume in Bipolar Disorder
Type 2 diabetes can damage the brain, particularly by reducing volume of the hippocampus, and frequently occurs in patients with bipolar disorder. A recent study of patients with bipolar disorder and abnormal glucose metabolism showed that patients with bipolar disorder who also had insulin resistance, glucose intolerance, or type 2 diabetes had smaller hippocampi than both patients with bipolar disorder and normal glucose function and normal control participants without a psychiatric disorder. In those with bipolar disorder and glucose abnormalities, age was associated with lower hippocampal volume to a greater extent than in bipolar patients with normal glucose function.
In the study, published by Tomas Hajek et al. in the journal Neuropsychopharmacology, not only did diabetes or prediabetes reduce the size of the hippocampus, but also reduced gray matter in the cerebral cortex, including the insula.
The researchers hope that treating diabetes, or possibly even its initial symptoms, more effectively may prevent these gray matter losses and slow brain aging in patients with bipolar disorder.









