Long COVID ‘Brain Fog’ Confounds Doctors, but New Research Offers Hope
James C. Jackson, PsyD, a licensed psychologist specializing in neuropsychology and rehabilitation, at Vanderbilt University School of Medicine and author of a new book, Clearing the Fog: From Surviving to Thriving With Long COVID ? A Practical Guide, reports in Medscape July, 2023 : “There’s not a lot of imprecision in the term (brain fog) because it might mean different things to different patients,”
Jackson, who began treating [a patient] in February 2023, said that it makes more sense to call brain fog a brain impairment or an acquired brain injury (ABI) because it doesn’t occur gradually. COVID damages the brain and causes injury. For those with long COVID who were previously in the intensive care unit and may have undergone ventilation, hypoxic brain injury may result from the lack of oxygen to the brain.
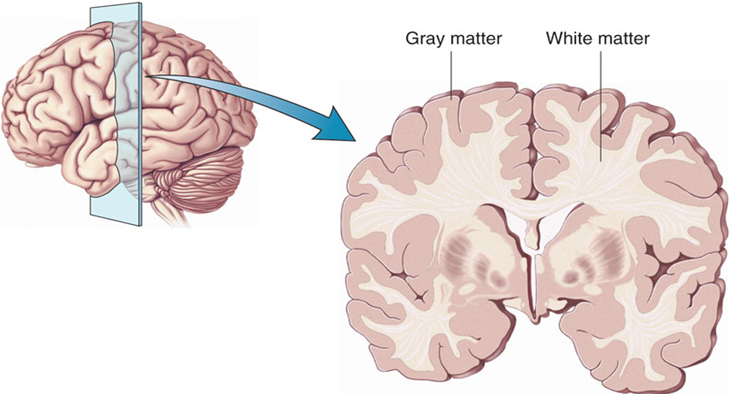
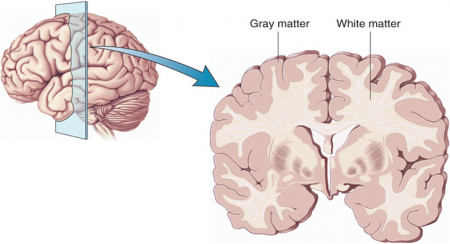
An April 2022 study published in the journal Nature found strong evidence that SARS-CoV-2 infection may cause brain-related abnormalities, for example, a reduction in gray matter in certain parts of the brain, including the prefrontal cortex, hypothalamus, and amygdala.
Additionally, white matter, which is found deeper in the brain and is responsible for the exchange of information between different parts of the brain, may also be at risk of damage as a result of the virus, according to a November 2022 study published in the journal SN Comprehensive Clinical Medicine.“
Thus, new data suggest that long COVID is associated with inflammation and both reduced volume of several brain structures and decreases in white matter. These data suggest several novel approaches to therapy that require further study. One is low dose lithium which both increases gray matter volume and white matter integrity. Lithium also has some antiviral properties. This could be combined with anti-inflammatories that could be bought over the counter such as N-acetylcysteine (NAC), acetyl-L-carnitine, and celecoxib.
Note of caution. This is only an untested hypothesis and would need to be discussed with one’s physician before any of these options are considered.
Transcranial Direct Current Stimulation (tDCS) Induces Gray-Matter Increases in Depression
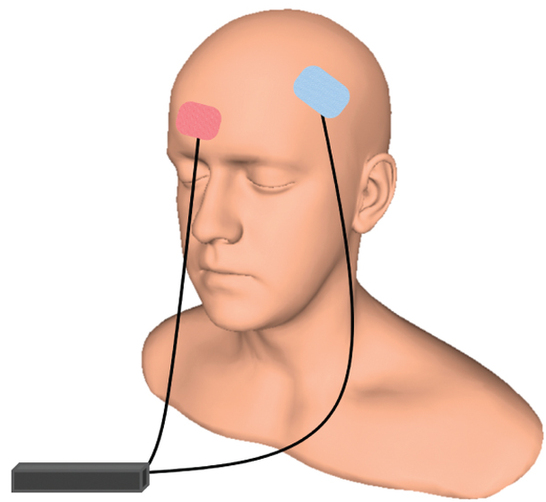
At the 2021 meeting of the Society of Biological Psychiatry (SOBP), researcher Mayank Jog and colleagues described a study of transcranial direct current stimulation (tDCS) in 59 patients with moderate depression. The patients received either tDCS sessions that delivered electrical current at 2mA for 20 minutes or a same-length sham stimulation delivered using a double-blind stimulator, for a total of 12 sessions over 12 consecutive working days. Jog and colleagues found that compared to the sham stimulation, tDCS induced increases in gray matter volume in the left dorsolateral prefrontal cortex (DLPFC) target area, with a statistically large effect size (Cohen’s d = 1.3). The researchers plan to follow up this study that found structural changes to the brain after tDCS with more research on the antidepressant effects of the treatment.
Lithium Reverses Thinning of the Cortex That Occurs in Bipolar Disorder
In a 2018 article in the journal Molecular Psychiatry, researcher Derrek P. Hibar reported findings from the largest study to date of cortical gray matter thickness. Researchers in the ENIGMA Bipolar Disorder Working Group, which comprises 28 international research groups, contributed brain magnetic resonance imaging (MRI) from 1837 adults with bipolar disorder and 2582 healthy control participants.
Hibar and colleagues in the working group found that in adults with bipolar disorder, cortical gray matter was thinner in the frontal, temporal, and parietal regions of both brain hemispheres. They also found that bipolar disorder had the strongest effect on three regions in the left hemisphere: the pars opercularis, the fusiform gyrus, and the rostral middle frontal cortex.
Those who had had bipolar disorder longer (after accounting for age at the time of the MRI) had less cortical thickness in the frontal, medial parietal, and occipital regions.
A history of psychosis was associated with reduced surface area.
The researchers reported the effects of various drug treatment types on cortical thickness and surface area. In adults and adolescents, lithium was associated with improvements in cortical thickness, and the researchers hypothesized that lithium’s protective effect on gray matter was responsible for this finding. Antipsychotics were associated with decreased cortical thickness.
In people taking anticonvulsant treatments, the thinnest parts of the cortex were the areas responsibly for visual processing. Visual deficits are sometimes reported in people taking anticonvulsive treatments.
Different Types of Trauma Affect Brain Volume Differently
Post-traumatic stress disorder (PTSD) has been associated with decreased volume of gray matter in the cortex. Research by Linghui Meng and colleagues has revealed that the specific types of trauma that precede PTSD affect gray matter volume differently.
At the 2016 meeting of the Society for Neuroscience, Meng reported that PTSD from accidents, natural disasters, and combat led to different patterns of gray matter loss. PTSD from accidents was associated with gray matter reductions in the bilateral anterior cingulate cortex (ACC) and medial prefrontal cortex (mPFC). PTSD from natural disasters was linked to gray matter reductions in the mPFC and ACC, plus the amygdala and left hippocampus. PTSD from combat reduced gray matter volume in the left striatum, the left insula, and the left middle temporal gyrus.
Meng and colleagues also found that severity of PTSD was linked to the severity of gray matter reductions in the bilateral ACC and the mPFC.
In a 2016 article in the journal Scientific Reports, Meng and colleagues reported that single-incident traumas were associated with gray matter loss in the bilateral mPFC, the ACC, insula, striatum, left hippocampus, and the amygdala, while prolonged or recurrent traumas were linked to gray matter loss in the left insula, striatum, amygdala, and middle temporal gyrus.
Brain Scans Differentiate Suicidal from Non-Suicidal Patients with Bipolar Disorder
 People with bipolar disorder are at high risk for suicidal behavior beginning in adolescence and young adulthood. A 2017 study by Jennifer A. Y. Johnston and colleagues in the American Journal of Psychiatry uses several brain-scanning techniques to identify neurobiological features associated with suicidal behavior in people with bipolar disorder compared to people with bipolar disorder who have never attempted suicide. Clarifying which neural systems are involved in suicidal behavior may allow for better prevention efforts.
People with bipolar disorder are at high risk for suicidal behavior beginning in adolescence and young adulthood. A 2017 study by Jennifer A. Y. Johnston and colleagues in the American Journal of Psychiatry uses several brain-scanning techniques to identify neurobiological features associated with suicidal behavior in people with bipolar disorder compared to people with bipolar disorder who have never attempted suicide. Clarifying which neural systems are involved in suicidal behavior may allow for better prevention efforts.
The study included 26 participants who had attempted suicide and 42 who had not. Johnston and colleagues used structural, diffusion tensor, and functional magnetic resonance imaging (MRI) techniques to identify differences in the brains of attempters and non-attempters.
Compared to those who had never attempted suicide, those who had exhibited reductions in gray matter volume in the orbitofrontal cortex, hippocampus, and cerebellum. They also had reduced white matter integrity in the uncinate fasciculus, ventral frontal, and right cerebellum regions. In addition, attempters had reduced functional connectivity between the amygdala and the left ventral and right rostral prefrontal cortex. Better right rostral prefrontal connectivity was associated with less suicidal ideation, while better connectivity of the left ventral prefrontal area was linked to less lethal suicide attempts.
Marker of Heart Failure May Predict Brain Deterioration
 A protein released into the blood in response to heart failure may be able to predict brain deterioration before clinical symptoms appear. The protein, N-terminal pro-B-type natriuretic peptide (NT-proBNP), is released when cardiac walls are under stress. High levels of NT-proBNP in the blood are a sign of heart disease. A 2016 Dutch study indicated that high levels of NT-proBNP in the blood are also linked to smaller brain volume, particularly small gray matter volume, and to poorer organization of the brain’s white matter. The study by researcher Hazel I. Zonneveld and colleagues, published in the journal Neuroradiology, assessed heart and brain health in 2,397 middle-aged and elderly people with no diagnosed heart or cognitive problems.
A protein released into the blood in response to heart failure may be able to predict brain deterioration before clinical symptoms appear. The protein, N-terminal pro-B-type natriuretic peptide (NT-proBNP), is released when cardiac walls are under stress. High levels of NT-proBNP in the blood are a sign of heart disease. A 2016 Dutch study indicated that high levels of NT-proBNP in the blood are also linked to smaller brain volume, particularly small gray matter volume, and to poorer organization of the brain’s white matter. The study by researcher Hazel I. Zonneveld and colleagues, published in the journal Neuroradiology, assessed heart and brain health in 2,397 middle-aged and elderly people with no diagnosed heart or cognitive problems.
Researchers are working to clarify the relationship between cardiac dysfunction and preliminary brain disease, but researcher Meike Vernooij says it is likely cardiac dysfunction comes first and leads to brain damage. Measuring biomarkers such as NT-proBNP may help identify brain diseases such as stroke and dementia earlier and allow for earlier treatment and lifestyle changes that can slow or reverse the course of disease.
Low Vitamin D Linked to Small Hippocampus & Schizophrenia
Low levels of vitamin D have been linked to schizophrenia in several studies. In one, infants with low vitamin D were more likely to develop schizophrenia in adulthood, but supplementation reduced this risk. A 2015 article by Venkataram Shivakumar and colleagues in the journal Psychiatry Research: Neuroimaging found that among patients with schizophrenia who were not currently taking (or in some cases, had never taken) antipsychotic medication, low levels of vitamin D were linked to smaller gray matter volume in the right hippocampus, an area involved in schizophrenia.
Vitamin D has neuroprotective effects and is important to normal brain development and function. Vitamin D is essential to the production of brain-derived neurotrophic factor (BDNF), a protein that is important for learning and memory, and vitamin D also reduces oxidative stress. BDNF deficiency and oxidative stress have both been linked to schizophrenia, and they both can cause abnormalities in the hippocampus.
Schizophrenia: The Importance of Catching It Early
By the time psychosis appears in someone with schizophrenia, biological changes associated with the illness may have already been present for years. A 2015 article by R.S. Kahn and I.E. Sommer in the journal Molecular Psychiatry describes some of these abnormalities and how treatments might better target them.
One such change is in brain volume. At the time of diagnosis, schizophrenia patients have a lower intracranial volume on average than healthy people. Brain growth stops around age 13, suggesting that reduced brain growth in people with schizophrenia occurs before that age.
At diagnosis, patients with schizophrenia show decrements in both white and grey matter in the brain. Grey matter volume tends to decrease further in these patients over time, while white matter volume remains stable or can even increase.
Overproduction of dopamine in the striatum is another abnormality seen in the brains of schizophrenia patients at the time of diagnosis.
Possibly years before the dopamine abnormalities are observed, underfunctioning of the NMDA receptor and low-grade brain inflammation occur. These may be linked to cognitive impairment and negative symptoms of schizophrenia such as social withdrawal or apathy, suggesting that there is an at-risk period before psychosis appears when these symptoms can be identified and addressed. Psychosocial treatments such as individual, group, or family psychotherapy and omega-3 fatty acid supplementation have both been shown to decrease the rate of conversion from early symptoms to full-blown psychosis.
Using antipsychotic drugs to treat the dopamine abnormalities is generally successful in patients in their first episode of schizophrenia. Use of atypical antipsychotics is associated with less brain volume loss than use of the older typical antipsychotics. Treatments to correct the NMDA receptor abnormalities and brain inflammation, however, are only modestly effective. (Though there are data to support the effectiveness of the antioxidant n-acetylcysteine (NAC) on negative symptoms compared to placebo.) Kahn and Sommer suggest that applying treatments when cognitive and social function begin to be impaired (rather than waiting until psychosis appears) could make them more effective.
The authors also suggest that more postmortem brain analyses, neuroimaging studies, animal studies, and studies of treatments’ effects on brain abnormalities are all needed to clarify the causes of the early brain changes that occur in schizophrenia and identify ways of treating and preventing them.
RTMS for Depression Increases Volume of Specific Brain Regions
Repeated transcranial magnetic stimulation (rTMS) is a treatment for depression in which magnets placed near the skull stimulate electrical impulses in the brain. In a poster presented at the 2015 meeting of the Society of Biological Psychiatry, Martin Lan and colleagues presented results of the first study of structural changes in the brain following rTMS.
In the study, 27 patients in an episode of major depression underwent magnetic resonance brain scans before and after receiving rTMS treatment over their left prefrontal cortices. Lan and colleagues reported that several cortical regions related to cognitive appraisal, the subjective experience of emotion, and self-referential processing increased in volume following rTMS treatment: the anterior cingulate, the cingulate body, the precuneous, right insula, and gray matter in the medial frontal gyrus. The increases ranged from 5.3% to 15.7%, and no regions decreased in volume. More than 92% of the participants showed increased gray matter in all of these regions.
The brain changes were not correlated with antidepressant response to rTMS, but suggest a possible mechanism by which rTMS is effective in some people. Lan and colleagues concluded that rTMS likely had neuroplastic effects in areas of the brain that are important for emotion regulation.
Atypical Antipsychotics May Slow Loss of Gray Matter in Schizophrenia
Progressive losses in gray matter have been observed in the cortex of people with schizophrenia, and those at high risk for the illness. In the past, studies have shown that the amount of antipsychotics a patient is exposed to is correlated with the extent of their deficits in gray matter, suggesting that antipsychotic treatment could exacerbate gray matter loss.
A new meta-analysis by Antotonio Vita and colleagues in the journal Biological Psychiatry shows that first-generation antipsychotics were associated with greater losses in gray matter compared with atypical antipsychotics, which seemed to slow the loss of gray matter.
The meta-analysis analyzed data from 18 longitudinal studies comparing a total of 1155 patients with schizophrenia to 911 healthy control participants. Magnetic resonance imaging (MRI) scans showed that over time, patients with schizophrenia lost more cortical gray matter volume. The patients’ cumulative intake of any kind of antipsychotic between MRI scans was associated with gray matter losses. But when Vita and colleagues drilled down to find differences between patients taking first-generation antipsychotics and those taking second-generation atypical antipsychotics, they found that patients with higher average daily intake of first-generation antipsychotics had greater losses in gray matter, while patients with higher average daily intake of atypical antipsychotics had less progressive losses in gray matter.
This study is the first to compare the effects of first-generation antipsychotics, which were developed in the 1960s, with those of atypical antipsychotics, which came into frequent use in the late 1980s, on cortical gray matter loss in schizophrenia. While first-generation antipsychotics are associated with the side effect of tardive dyskinesia, involuntary movements of the face and jaw, atypical antipsychotics are most commonly associated with weight gain.
Three studies have randomly assigned patients with schizophrenia to receive either first-generation or atypical antipsychotics. In these studies as well, second-generation antipsychotics were associated with smaller losses in gray matter.
The authors speculate that either second-generation antipsychotics may have neuroprotective effects, or first-generation antipsychotics may have neurotoxic effects. They also suggest that first-generation antipsychotics may not have the capacity to interfere with the natural progression of schizophrenia in terms of gray matter losses.
Future studies may investigate differences between specific antipsychotic medications’ effects on gray matter volume. Vita and colleagues reported that in the analysis, the atypical antipsychotic clozapine was associated with the least loss of gray matter of any medication in the included studies.
Editor’s Note: This study is important because it adds to findings questioning the conclusions of a large National Institute of Mental Health–sponsored study known as CATIE and a meta-analysis by John Geddes published in the journal BMJ in 2000, in which he wrote that “There is no clear evidence that atypical antipsychotics are more effective or better tolerated than conventional (first generation) antipsychotics.” Read more