Atypical Antipsychotics May Slow Loss of Gray Matter in Schizophrenia
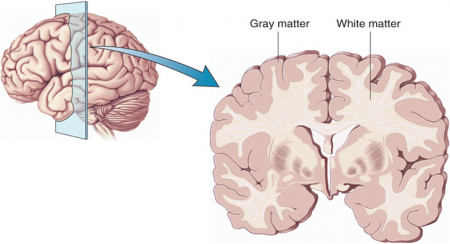
Progressive losses in gray matter have been observed in the cortex of people with schizophrenia, and those at high risk for the illness. In the past, studies have shown that the amount of antipsychotics a patient is exposed to is correlated with the extent of their deficits in gray matter, suggesting that antipsychotic treatment could exacerbate gray matter loss.
A new meta-analysis by Antotonio Vita and colleagues in the journal Biological Psychiatry shows that first-generation antipsychotics were associated with greater losses in gray matter compared with atypical antipsychotics, which seemed to slow the loss of gray matter.
The meta-analysis analyzed data from 18 longitudinal studies comparing a total of 1155 patients with schizophrenia to 911 healthy control participants. Magnetic resonance imaging (MRI) scans showed that over time, patients with schizophrenia lost more cortical gray matter volume. The patients’ cumulative intake of any kind of antipsychotic between MRI scans was associated with gray matter losses. But when Vita and colleagues drilled down to find differences between patients taking first-generation antipsychotics and those taking second-generation atypical antipsychotics, they found that patients with higher average daily intake of first-generation antipsychotics had greater losses in gray matter, while patients with higher average daily intake of atypical antipsychotics had less progressive losses in gray matter.
This study is the first to compare the effects of first-generation antipsychotics, which were developed in the 1960s, with those of atypical antipsychotics, which came into frequent use in the late 1980s, on cortical gray matter loss in schizophrenia. While first-generation antipsychotics are associated with the side effect of tardive dyskinesia, involuntary movements of the face and jaw, atypical antipsychotics are most commonly associated with weight gain.
Three studies have randomly assigned patients with schizophrenia to receive either first-generation or atypical antipsychotics. In these studies as well, second-generation antipsychotics were associated with smaller losses in gray matter.
The authors speculate that either second-generation antipsychotics may have neuroprotective effects, or first-generation antipsychotics may have neurotoxic effects. They also suggest that first-generation antipsychotics may not have the capacity to interfere with the natural progression of schizophrenia in terms of gray matter losses.
Future studies may investigate differences between specific antipsychotic medications’ effects on gray matter volume. Vita and colleagues reported that in the analysis, the atypical antipsychotic clozapine was associated with the least loss of gray matter of any medication in the included studies.
Editor’s Note: This study is important because it adds to findings questioning the conclusions of a large National Institute of Mental Health–sponsored study known as CATIE and a meta-analysis by John Geddes published in the journal BMJ in 2000, in which he wrote that “There is no clear evidence that atypical antipsychotics are more effective or better tolerated than conventional (first generation) antipsychotics.”
People taking first-generation antipsychotics exhibit more extrapyramidal side effects (which include muscle spasms, restlessness, or rigidity) and have a higher incidence of tardive dyskinesia. Patients with bipolar disorder are even more prone to tardive dyskinesia than patients with schizophrenia; some 20–30% of people with bipolar disorder exposed to first-generation antipsychotics get this side effect.
First-generation antipsychotics can exacerbate bipolar depression, while two atypical antipsychotics, quetiapine and lurasidone, have actually been approved by the Federal Drug Administration (FDA) for the treatment of bipolar depression.
Now the meta-analysis by Vita and colleagues suggests that the different classes of antipsychotics have a differential effect on gray matter loss in schizophrenia. This would be consistent with findings that some atypical antipsychotics, such as quetiapine and lurasidone, increase the neuroprotective factor BDNF in the hippocampus and prevent stress from decreasing BDNF, while the first-generation antipsychotic haloperidol exacerbates the effects of stress, further decreasing BDNF in the hippocampus.
For all of these reasons, the atypical antipsychotics now appear to be preferable to first-generation antipsychotics for patients with bipolar disorder, and perhaps also for those with schizophrenia.
(A note about potential conflict of interest. This editor, Robert M. Post, sometimes serves as a paid speaker for the drug companies AstraZeneca, which makes quetiapine; Sunovion, which produces lurasidone; and Validus, which makes the long-acting carbamazepine drug Equetro. His opinion (expressed in the BNN and elsewhere) that the atypical antipsychotics are preferable to older antipsychotics predated his paid work for these companies.
New data suggesting that atypical antipsychotics are better than first-generation antipsychotics in terms of efficacy in bipolar depression, incidence of tardive dyskinesia, effect on BDNF, and now gray matter loss in schizophrenia have emerged since these speaking engagements began.)