A Question for Physicians
Do you know how to treat a patient with a persistent horrendous side effect to a single dose of the SSRI Lexapro 20mg?
A patient wrote me, asking if I know any physicians who have seen this syndrome and know how to treat it.
After a single dose: “Sleep is ruined, Can’t nap or wake up sick feeling, Constant feeling like I am in agony, Can’t focus / concentrate, Can’t regulate body temperature, loss of appetite and libido, Memory issues, Extreme fatigue, Unintentional a weight loss, Muscles usually twitching somewhere, and Abnormal breathing”.
If you have seen this type of reaction and/or know how to treat it, please send your email to Scott Mclean at sdmclean@shaw.ca and a cc to me (the Editor of this newsletter) at Robert.postmd@gmail.com. The patient has given his informed consent for this email to be posted on www.bipolarnews.org.
Dextromethorphan potentiates the anti-depressant effects of SSRIs
Maji et al reported in Psychiatry Research (2024) that dextromethorphan 30mg compared to placebo potentiated the antidepressant effects of SSRIs on all measures and had few side effects. It is FDA-approved to potentiate bupropion.
Now it looks like a more general property.
Psilocybin Bests SSRI for Major Depression in First Long-Term Comparison
“MILAN — Psilocybin leads to a better overall outcome in the treatment of moderate to severe major depressive disorder (MDD) than the selective serotonin reuptake inhibitor (SSRI) escitalopram, results of the first long-term comparison of the two treatments suggest.
“This is the first work to compare the long-term effects of these two drugs in the context of overall well-being, not just freedom from depression,” study investigator Tommaso Barba, PhD, candidate Imperial College London, London, England, said in a press release. “Psilocybin outperformed escitalopram in several measures of well-being, meaning in life, work, and social functioning.”
Findings from the 6-month follow-up study of a phase 2 double-blind, randomized, controlled trial were presented on September 22 at the 37th European College of Neuropsychopharmacology (ECNP) Congress and published simultaneously in The Lancet eClinicalMedicine….The initial single-center study included 59 adults with MDD (mean age, 41 years) who were randomized to receive either psilocybin or escitalopram over a 6-week period. The psilocybin arm (n = 30) received two 25-mg oral doses of psilocybin therapy (PT), and the escitalopram arm (n = 29) received 10-20 mg of daily escitalopram plus two (placebo-like) 1-mg doses of psilocybin (ET). Both groups received psychological support….The researchers conclude that while a short course of SSRIs combined with intensive therapeutic support (around 20 hours) “might be enough to induce sustained antidepressant effects,” patients treated with psilocybin showed greater improvements in general functioning, connectedness, and meaning in life.
Although not reassessed in the follow-up, the initial study showed that adverse events, particularly sexual functioning, favored psilocybin, said Barba.”
Family History of Alcohol Dependence Predicts Antidepressant Response to an NMDA Antagonist
LE Phelps reported in Biol. Psy (2009) that subjects with a family history of alcohol dependence showed significantly greater improvement in MADRS scores compared with subjects who had no family history of alcohol dependence.
They concluded that a family history of alcohol dependence appears to predict a rapid initial antidepressant response to the NMDA receptor antagonist ketamine.
Intramuscular versus Intravenous Ketamine for the Management of Treatment-Resistant Depression and Suicidal Ideation
Cristina Albott of the University of Minnesota Medical School reported relatively similar efficacy of intramuscular versus intravenous ketamine for the management of treatment-resistant depression and suicidal ideation in outpatient settings.
“Intramuscular (IM) delivery represents an underexplored and promising route of administration given its high bioavailability and low cost….Sixty-six patients underwent a series of 7 to 9 IV (n=35) or IM (n=31) administrations of 0.5mg/kg ketamine during a 21-28 day period. Both IV and IM showed similar magnitudes of improvement in depression, but surprisingly only the IM route was associated in a significant improvement in suicidal ideation in a within subjects change.”
“No adverse events occurred throughout the treatment series for either administration route…. This clinical case series provides preliminary support for the effectiveness and safety of IM compared to IV ketamine in TRD. “
LITHIUM IS VASTLY UNDER-UTILIZED IN BIPOLAR DISORDER LEADING TO PREMATURE DEATH AND DISABILITY: WE WANT YOU TO HELP REVERSE THIS ANOMALOUS TREND
We are looking for people who have had a good course of illness with lithium included in their treatment regimen to help spread the word that lithium works extremely well and its side effects are erroneously overestimated.
We are hoping that you, as a good responder to lithium, will start a positive chain letter to fellow patients, family members, and friends suggesting that earlier and greater use of lithium would be overwhelmingly likely to improve the lives of many individuals with bipolar illness.
Why do we need you? It is because every expert in the treatment of bipolar illness of whom I am aware of has long advocated for greater and earlier use of lithium, but with little success. Lithium is widely recognized as a first line and treatment of choice for bipolar disorder, yet its use remains miniscule. In the US somewhere between only 10 to 27% of bipolar patients are given lithium. This has tragic consequences.
Treatment outcomes of the illness remain poor with vast numbers of patients experiencing pain, disability, memory loss, and loss of many years of life expectancy from suicide, cardiovascular disease, and many other psychiatric and medical disabilities. Compared to the general population, people with bipolar illness lose between 10-15 years of life expectancy. A new study by Carvalho et al (Psychother Psychosom, 2024) of more than 50,000 patients with a first episode of mania compared to more than 250,000 matched controls have a significantly higher rate of all cause mortality and a 10 fold increase of suicide. Those treated with lithium have a significantly lower rate of both all cause mortality and of suicide.
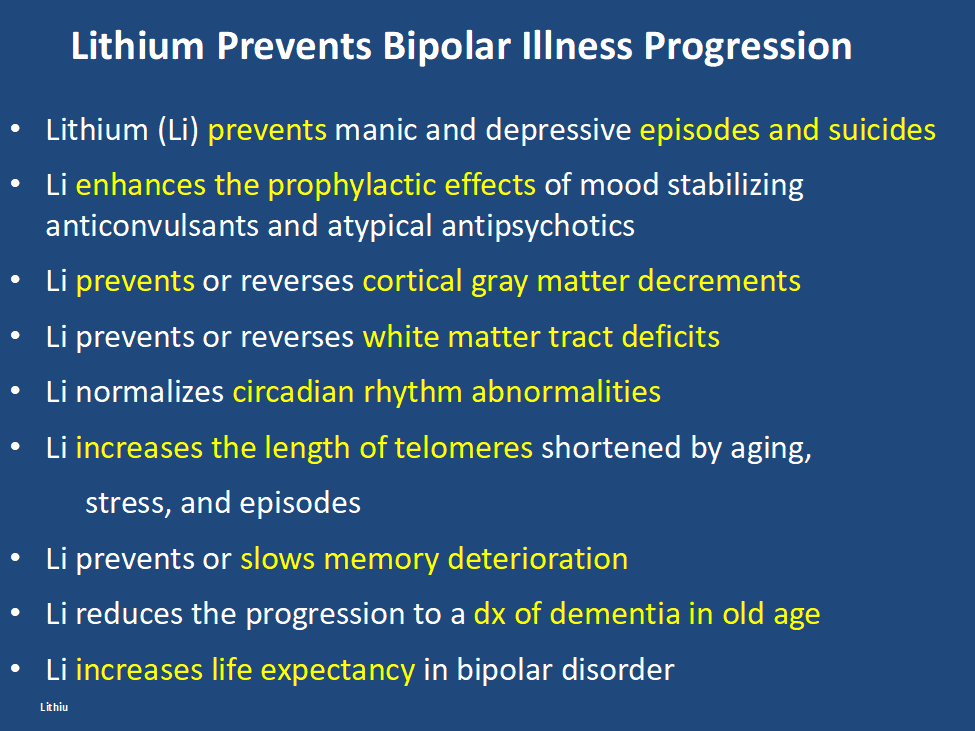
In addition, lithium has many other assets, besides the treatment of mania, of which most people are unaware and the liabilities of its side effects profile are over estimated. Some of the positive’s of lithium are listed below. Please print this ‘list of assets of lithium out and give it to everyone who might be interested. Patients with bipolar disorder should also print it out for their treating physicians, particularly if they do not as yet have lithium in their treatment regimen.
At the same time lithium’s side effects are over emphasized. The biggest concern is that lithium causes end stage kidney dysfunction eventually leading to dialysis. This is likely based on findings that individuals with bipolar disorder have an increase in most medical illnesses including chronic kidney disease compared to the general population. However, two very large trans-national studies of bipolar patients in Denmark and in Israel have found that bipolar patients treated with lithium are no more likely to get end stage renal disease than those treated with anticonvulsants such as valproate (Depakote). Lithium does cause low thyroid function in 15-25% of patients, but this is easily corrected with replacement of thyroid hormone. Many other side effects of lithium such as tremor can be managed by using lower doses.
Bottom line: Lithium gets a bad rap.
Please tell everyone you know about the new data on lithium’s relative safety and its many assets including reducing all cause mortality and suicide and restoring many years of lost life expectancy. 14 of 15 studies indicate that if lithium is started early in course of bipolar disorder it is more effective than starting it after many episodes or rapid cycling have occurred. It also works well in youngsters with bipolar disorder and better in comparison to other treatments (Hafeman et al 2020). In addition, after a first mania, patients randomized to a year of treatment with lithium do better on all outcome measures than those given a year on quetiapine (Seroquel) including manic and depressive severity, functioning, cognition, and normality of brain imaging (Berk et al 2017).
One more conceptual breakthrough: Lithium is literally the original salt of the earth. It was generated just 20 minutes after the big bang origin of the universe and is considered an essential element. Common table salt, sodium chloride, emerged only many millions of years after the big bang. Also in six studies across multiple countries, higher minute levels of lithium in the drinking water have been shown to reduce the incidence of suicide in the general population. A very low dose of lithium 150-300mg/day has also been shown to reduce the progression of mild cognitive impairment in otherwise well elderly volunteers.
Do a good thing for other people. Relay this new view of lithium to everyone you can think of in hope that they will help get the word out to many others and improve the life, functioning, and longevity of those with bipolar disorder.
Suggest and promulgate a new mantra:
“LITHIUM PREVENTS EPISODES OF BIPOLAR ILLNESS, AND PROTECTS THE BRAIN AND BODY”
GLP-1s Might Decrease the Incidence of Depression and Anxiety
Lisa O’Mary of WebMD wrote: “People taking a popular type of drug for weight loss or to manage diabetes have a lower likelihood of being newly diagnosed with depression or anxiety, according to an analysis of millions of people’s health records.
The findings were published this week by researchers from the electronic health record company Epic. Researchers looked for new diagnoses of depression or anxiety among people who started taking drugs from a class called GLP-1 agonists that can help manage blood sugar or treat obesity by mimicking hormone levels in the body that can affect appetite and blood sugar. Many people who take the drugs experience significant weight loss.
The researchers found that people with diabetes who started taking most versions of GLP-1 agonists were between 11% and 65% less likely to be newly diagnosed with depression than people with diabetes who didn’t take one of the drugs. The greatest reduction in likelihood of a new depression diagnosis was observed among people taking tirzepatide, which is sold under the brand names Mounjaro and Zepbound.”
Antidepressant Use and Risk of Manic Episodes in Children and Adolescents With Unipolar Depression
Suvi Virtanen, PhD; et al in JAMA Psychiatry. September 27, 2023. report a low risk of switching in youngsters with unipolar depression. However, the odds ratio for a switch were significantly elevated when there was concomitant use of anticonvulsants and antipsychotics, and there was a four fold increased risk if a parent had bipolar disorder. Thus one should be particularly careful about treating depression with antidepressants (AD) when there is a positive parental history of bipolar disorder and one should think of other options, such as lamotrigine, an atypical with good AD effects, or lithium.
NEW DATA ON EXTENDING THE EFFFECTS OF IV KETAMINE: Implications for countering the effects of stigma.
John Krystal of Yale U. in an article in Proceedings of the National Academy of Sci. (2023) gave new information about the anatomical and physiological effects of ketamine and about how to extend its effects. Ketamine in animals acutely (in a matter of hours) increases spines, synapses, and dendrites and physiological connectivity in neurons in the prefrontal cortex. Data now support these findings in humans with depression, but AD effects of ketamine tend to dissipate over a period of 3 to 5 days and require repeated infusions to maintain the improvement. Synaptic density can be measured with SV2A and this can be enhanced with a Navitor Pharmaceuticals drug acting on mTORC1. Surprisingly low doses of rapamycin, an inhibitor of mTOR1, extends the duration of AD effects of ketamine, increasing the response rate at 2 weeks of 13% to 41%. Ketamine restores only the spines that have been reduced in depression and rapamycin is thought to extend the duration of the restored spines. It may do this by increasing the neurotropic effects of microglia. The tripartite synapse of pre and post synaptic neurons and astrocytes, may now be better described as the tetrapartite synapse with the inclusion of microglial.
Adding psychotherapy to the effects of ketamine in PTSD increases and extends efficacy.
AD effects of ketamine can be extended with cognitive behavioral therapy. Thus, ketamine increases synaptic efficacy, synaptic density, glutamate homeostasis, and experience-dependent neuroplasticity. Extending the persistence of these effects by various chemical and psychotherapeutic mechanisms may give new ways of enhancing and prolonging the therapeutic effects of this rapidly acting agent.
Interestingly, Kaye at Yale U. reports that in contrast to transient effects of ketamine, the AD effects of therapy-assisted psilocybin appear to be very long lasting and the associated increases in spines persist for longer than 37 days. Another psychedelic MDMA that is effective in PTSD causes large increases in spines, although they are less persistent and are gone by 34 days.
Editors Note: As we have previously highlighted in the BNN, these data on ketamine and other psychedelics reversing the anatomical and physiological deficits in prefrontal neurons of depressed animals and humans (spines, dendrites, synapses and intercellular communication), give a new view of the real, reliable, and replicable neurological defects accompanying depression. The rapid correction of these neural abnormalities in conjunction with the rapid induction of antidepressant effects are not only paradigm shifting from a treatment perspective, but have major implications for the assertion that there is a neurobiological basis of depression and its treatment.
As such, these data should do much to counter the continuing stigma too often accompanying the term “mental” illness that it is somehow not as real as other medical and neurological conditions, and as it is often asserted that “it is just all in one’s head.” This picks up on the unfortunate associations and definitions of “mental” as imaginary, all in the mind, and evanescent and that mental illness can readily be countered with effort and will power such as “pulling oneself up by the bootstraps,” (the latter of which is in itself a logical impossibility.)A Case Report: Good Effect of Psilocybin Even with No Psychedelic Effects
Highlights from the International Society for Bipolar Disorders Conference Posters and Presentations, Chicago, June 22-25, 2023
Marisa Leon-Carlyle reported on a 43 yr. old man with chronic treatment refractory depression who was given psilocybin 25mg (a 5HT2A agonist) at 8:00 AM after receiving trazodone 200mg HS (which should be enough to block 80% of 5HT2A receptors). He had an excellent antidepressant response, was able to feel emotion and new love for his wife, and finally felt that doing one’s best is good enough. Obviously further systematic study is needed.

