Transcranial Direct Current Stimulation Plus Zoloft Has Better Antidepressant Effects Than Either Treatment Alone
 Transcranial direct current stimulation (tDCS), in which a barely perceptible level of electrical current is applied directly from one side of a patient’s scalp to the other, is a promising treatment for patients with tought-to-treat depression. A 2013 study by Brunoni et al. in JAMA Psychiatry examined whether combined treatment using tDCS and the selective-serotonin reuptake inhibitor (SSRI) antidepressant sertraline (Zoloft) would be a safe and effective treatment for unipolar depression. The combination was better than either treatment alone and better than placebo.
Transcranial direct current stimulation (tDCS), in which a barely perceptible level of electrical current is applied directly from one side of a patient’s scalp to the other, is a promising treatment for patients with tought-to-treat depression. A 2013 study by Brunoni et al. in JAMA Psychiatry examined whether combined treatment using tDCS and the selective-serotonin reuptake inhibitor (SSRI) antidepressant sertraline (Zoloft) would be a safe and effective treatment for unipolar depression. The combination was better than either treatment alone and better than placebo.
The six-week study used what is called a 2×2 factorial design, in which 120 patients with unipolar depression received either 50 mg/day of sertraline or placebo and also received either real tDCS or a sham procedure. The tDCS was administered in twelve 30-minute sessions, one per day Monday through Friday during the first two weeks, followed by one every other week. TDCS consists of an anodal (positive) and cathodal (negative) current placed at particular positions on the head. This study used 2 microamps of anodal left/cathodal right prefrontal stimulation for the tDCS treatment.
While the combination of sertraline and tDCS was significantly better than all three other treatment options (sertraline plus sham procedure, placebo plus tDCS, and placebo plus sham procedure), sertraline by itself and tDCS by itself resulted in similar efficacies. However, TDCS by itself was also significantly better than placebo, while sertraline by itself was not.
Side effects among the different treatment options were similar, except those who received tDCS had more scalp redness. There were seven instances of patients developing mania or hypomania during the study, five of which occurred in the combined tDCS and sertraline treatment group, higher than the 1–2% rate that would be expected in a study of unipolar depression.
Second RTMS Device Approved for Treatment-Resistant Depression
In 2008, the Federal Drug Administration approved the Neuronetics company’s Neuro-Star system for delivering repeated transcranial magnetic stimulation to patients with treatment-resistant depression. In rTMS treatment, an electromagnetic coil is placed against the forehead and magnetic pulses that can penetrate the scalp are converted into small electrical currents that stimulate neurons in the brain. Now the FDA has approved a second device manufactured by Brainsway Ltd.
In 2012, Brainsway released data from their double-blind, multicenter controlled trials of the device. After five weeks of treatment, 30.4% of the patients who received the rTMS treatment achieved remission of their depression, twice the rate of remission among the patients who received a sham procedure instead.
Editor’s Note: These data showing slightly higher response rates than seen in two trials by Neuronetics confirm the efficacy of rTMS in patients whose depression persists after one or more trials with antidepressant medications. The efficacy of rTMS in those patients who have failed to respond to multiple antidepressant medications remains to be further defined, as do the optimal stimulation parameters to achieve the best results in this difficult-to-treat sub-group of patients.
Residue from Nuclear Bomb Testing Shows That Contrary to Earlier Reports, Neurogenesis Occurs in the Brains of Adults
 In 2013 we reported that according to Pasco Rakic, professor of neuroanatomy at Yale University, neurogenesis (the production of new neurons) occurs only in rodents, and not in any significant amount in the brains of adult primates. However, a new carbon-dating procedure shows that the adult human brain does actually continue to create new neurons.
In 2013 we reported that according to Pasco Rakic, professor of neuroanatomy at Yale University, neurogenesis (the production of new neurons) occurs only in rodents, and not in any significant amount in the brains of adult primates. However, a new carbon-dating procedure shows that the adult human brain does actually continue to create new neurons.
According to an article by Spalding et al. published more recently in the journal Cell, such neuroplasticity occurs to a much greater degree than previously thought. The authors base their research on levels of carbon isotope 14 (14C) that were released into the atmosphere during aboveground nuclear bomb tests between 1945 and 1963. Dividing cells require carbon, so the 14C released into the atmosphere during the era of nuclear testing made its way into the cells of people who were alive at the time. Levels of 14C that were incorporated into the DNA of dividing cells correlate with levels of 14C in the atmosphere at the time the cells divided, and since carbon levels have declined at a predictable rate since the nuclear tests, measuring the 14C in cells can show how old they are.
Spalding et al. show that neurogenesis in humans occurs only in the hippocampus. They found evidence that a subpopulation of hippocampal neurons continually renews itself at a rate of about 700 new neurons per day, while other hippocampal cells are non-renewing. The annual turnover rate of about 1.75% is the same for men and women and declines slightly with age.
The researchers were able to determine that the renewing cells play an important role in certain types of brain function. Long-term potentiation, the process by which learning and memory can occur, depends heavily on new cells produced in the part of the hippocampus knows as the dentate gyrus.
Neurosteroid Allopregnanolone May Improve Bipolar Depression
Sherman Brown of the University of Texas Southwestern reports that the neurosteroid allopregnanolone has positive effects in bipolar depression. Patients in Brown’s study received doses of 100mg capsules twice daily during the first week, then one capsule in the morning and two capsules in the evening during the second week, and two capsules in the morning and three capsules in the evening during the third week.
Neurosteroids can change the excitability of neurons through their interactions with the neurotransmitters that carry signals from neurons across synapses. Among the various types of neurotransmitters, GABA plays an inhibitory role, while glutamate is responsible for excitability. Allopregnanolone, which is naturally produced in the body, has positive effects on GABA receptors and inhibitory effects on glutamate NMDA receptors, so that it increases the balance of inhibition (GABA) over excitation (glutamate).
How Inflammation Increases Glutamate Overexcitation And Neurotoxicity
Research has shown a link between inflammation and mental illness. Inflammation leads to a series of chemical changes that can overexcite neurons and interfere with the protection of neurons.
Inflammation increases the production of indoleamine-pyrrole 2,3-dioxygenase (IDO), an enzyme that breaks down the amino acid tryptophan into kynurenic acid and quinolinic acid. They in turn increase glutamate, the main excitatory neurotransmitter, and decrease brain-derived neurotrophic factor (BDNF), which keeps neurons healthy.
Kynurenic acid stimulates microglia, which clean up the central nervous system as a form of immune defense, to produce inflammatory cytokine proteins.
Quinolinic acid directly stimulates glutamate receptors and encourages glutamate release from astrocytes. Quinolinic acid also blocks glutamate removal that would normally occur through reuptake into the astrocytes, leading to more stimulation of extrasynaptic glutamate receptors and decreases in BDNF.
Quinolinic acid’s effects are opposite to those of the antidepressant ketamine, which blocks glutamate NMDA receptors and increases BDNF. When people are given interferon protein for the treatment of cancers, quinolinic acid increases in cerebrospinal fluid, inducing depression. The severity of depression induced is correlated with the patient’s levels of quinolinic acid.
It appears that ketamine has indirect anti-inflammatory effects through its ability to block glutamate receptors and increase BDNF.
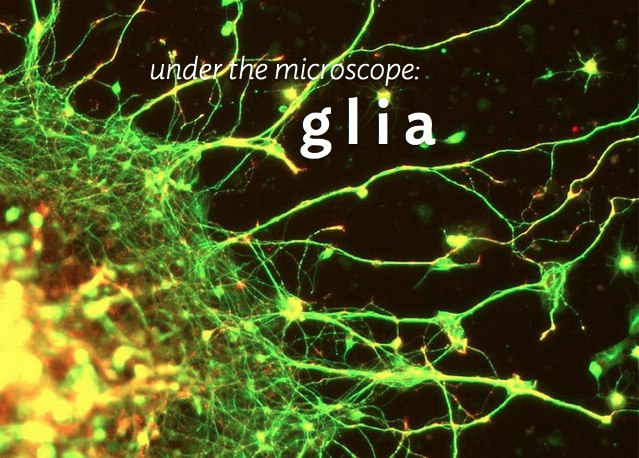
Glia Cells Prune Over-Abundant Neurons
The brain contains neurons, which transmit electrical impulses, and glia, which protect and support neurons. New evidence suggests that some types of glia also play a role in pruning back overabundant neurons that are produced as the brain develops in utero.
Researcher Beth Stevens reports that astrocytes secrete a protein called transforming growth factor beta (TGF-beta). TGF-beta is a cytokine, or regulating protein, that activates brain microglia to initiate a complement cascade (C1 to C3), a series of chemical changes that destroy unnecessary neurons and synapses.
The various proteins involved in a complement cascade are numbered. This complement cascade starts with C1q and is continued by C4, C2, and C3, which initiate phagocytosis (or eating up) of the axon terminals of the underutilized neurons, sparing those that are active.
Inflammation and other changes in glia could cause either deficient or excess pruning of neurons, which has been thought to occur in neuropsychiatric disorders such as autism or schizophrenia.
Buspirone and Melatonin Together May Treat Unipolar Depression
The combination of the anti-anxiety drug buspirone (trade name Buspar) and melatonin, a hormone that regulates cycles of sleep and waking, may be effective for depression. Researcher Maurizio Fava and other researchers at Massachusetts General Hospital report that low-dose buspirone (e.g. 15 mg/day) combined with a 3 mg dose of melatonin produced significant antidepressant effects in a six-week study of patients with unipolar depression.
While buspirone is not a potent antidepressant at low doses, the combination of buspirone and melatonin exerted significant effects, leading to better antidepressant response than did either placebo or 15 mg of buspirone alone. Another benefit of the combination is that the low dose of buspirone minimizes side effects.
Buspirone is a serotonin 5HT1A receptor partial agonist, meaning that it produces weak activity at this serotonin receptor, but does not allow it to get overstimulated.
Epigenetic Regulation of Social Attachment: Genes May Dictate Partner Preference
Prairie voles, which form monogamous bonds for life, are often studied as a source of information about social attachment. New findings indicate that these mating choices are regulated by epigenetics.
Epigenetics refers to changes in genes that do not affect the inherited sequence of DNA, but affect how easily the DNA is transcribed to produce proteins. Environmental events such as stress or exposure to chemicals can bring about epigenetic changes by adding or subtracting acetyl or methyl groups from strands of DNA or the histones around which it is wound.
When prairie voles mate naturally, levels of oxytocin, often thought of as the “bonding hormone,” increase in the reward area of the brain, the nucleus accumbens. When voles are given a drug that increases histone acetylation, their behavior mimics natural partner preference. The drug, known as a histone deacetylase (HDAC) inhibitor, blocks the removal of acetyl groups, and researchers Wang et al. reported in the journal Nature Neuroscience in 2013 that oxytocin levels increase in the nucleus accumbens. The voles receive the drug and mate for life, suggesting that social bonding is epigenetically regulated.
Similar epigenetic alterations may play a role in human social bonding and vulnerability to depression. Depressed mothers and their offspring have low levels of oxytocin in their blood, and maternal depression is a risk factor for depression in the offspring, as reported by Apter-Levy et al. in the American Journal of Psychiatry in 2013.
Editor’s Note: Perhaps depressed moms who show reduced physical and verbal interactions with their newborns should receive special training in holding, cuddling, cooing, and other social bonding activities that could increase their infants’ oxytocin levels and potentially also decrease their own anxiety and depression.
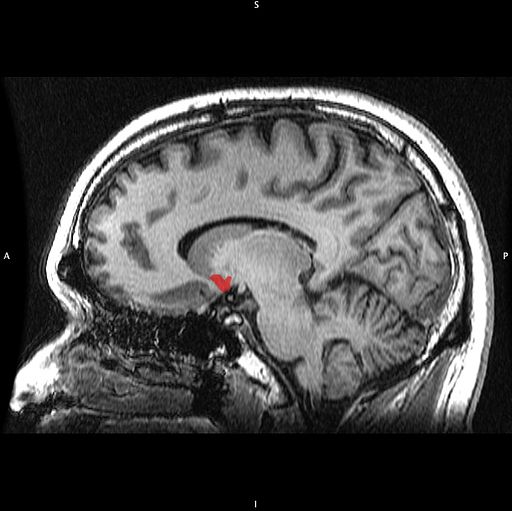
The Nucleus Accumbens in Depression
Brain-derived neurotrophic factor (BDNF) keeps neurons healthy and is critical for long-term memory and synapse formation. BDNF levels increase in the nucleus accumbens (the brain’s reward center) and decrease in the hippocampus during clinical depression and chronic cocaine use. In rodents, the same changes in BDNF levels occur during defeat stress (which resembles human depression).
Rodents who are repeatedly defeated by a larger rodent exhibit behaviors such as social withdrawal, lethargy, and decreased interest in sucrose. The increases in BDNF in the nucleus accumbens of these rodents could reflect the learning that takes place during the repeated defeat stress and the depression-like behaviors that follow it. Blocking the BDNF increases in the nucleus accumbens prevents these behaviors from developing.
Chadi Abdallah and other researchers at Yale University recently found that the left nucleus accumbens of patients with treatment-resistant depression is enlarged compared to normal controls, and the drug ketamine, which produces rapid-onset antidepressant effects, rapidly decreases the volume of the nucleus accumbens in the depressed patients. The mechanism by which it does so is unknown, but could reflect some suppression of the depressive learning.
Any relationship between the volume of the nucleus accumbens and its levels of BDNF is unknown, but ketamine’s effect on the size of this brain region could be linked to a decrease in the defeat-stress memories.
Blockade of Kappa Opiate Receptors Blocks Proneness to Relapse in Addiction
George Koob, the new director of the National Institute for Alcohol Abuse and Alcoholism (NIAAA), showed that animals with extended access to self-administered abuse substances like cocaine or morphine will escalate the amount of drug they self-administer. When the drug is no longer available starting after a delay of one to two weeks, the number of times they press a lever in the presence of a cue previously associated with drug availability progressively increases over a period of one to two months (even through no drug is available). This is called incubation and reflects a measure of “craving” or relapse potential.
This incubation effect, or increasing degree of craving for a drug, is also seen clinically in people who are heavy drug users and then achieve abstinence or are incarcerated and have a period of forced abstinence. As the duration of abstinence increases, they experience an increased proneness to relapse.
Dynorphin is a psychomimetic opiate peptide that is produced in the brain and causes anxiety and dysphoria when it is given to humans. While opiates like morphine and heroin that produce euphoria and antipain effects act at a mu opiate receptor, dynorphin acts at a kappa opiate receptor. Chronic cocaine use gradually increases levels of dynorphin in the brains of addicts and also increases kappa receptors, thus converting what is often initially a euphoric drug experience into an anxiety-producing and dysphoric one.
If kappa receptors are blocked, the incubation effects during abstinence described above do not occur, and presumably addicts would be less relapse-prone. No kappa antagonist is currently available for human use, but if one combines buprenorphine (a mixed opiate agonist/antagonist) with naloxone or naltrexone (which selectively block the mu opiate receptors), one would in effect have a kappa receptor antagonist. Koob showed that this drug combination could prevent the incubation effects in abstinent animals. Further study might lead to advances in the treatment of addition in humans.