Surface Area of Cortex Is Reduced After Multiple Manic Episodes
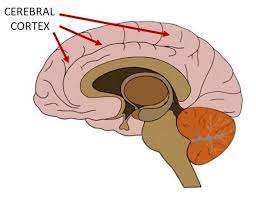
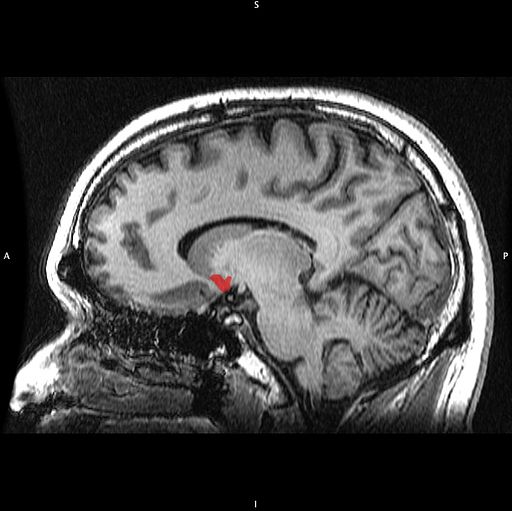
In a 2020 article in the journal Psychiatric Research: Neuroimaging, researcher Rashmin Achalia and colleagues described a study of structural magnetic resonance imaging (MRI) that compared 30 people with bipolar I disorder who had had one or several episodes of mania to healthy volunteers. Compared to the healthy volunteers, people with bipolar disorder had “significantly lower surface area in bilateral cuneus, right postcentral gyrus, and rostral middle frontal gyri; and lower cortical volume in the left middle temporal gyrus, right postcentral gyrus, and right cuneus.”
The surface area of the cortex in patients with bipolar I disorder who had had a single episode of mania resembled that of the healthy volunteers, while those who had had multiple manic episodes had less cortical surface area.
The data suggest that compared to healthy volunteers, people with bipolar disorder have major losses in brain surface area after multiple episodes that are not seen in first episode patients. In addition, the researchers found that both the number of episodes and the duration of illness was correlated with the degree of deficit in the thickness in the left superior frontal gyrus. These decreases in brain measures occurred after an average of only 5.6 years of illness.
Editor’s Note: These data once again emphasize the importance of preventing illness recurrence from the outset, meaning after the first episode. Preventing episodes may prevent the loss of brain surface and thickness.
Clinical data has also shown that multiple episodes are associated with personal pain and distress, dysfunction, social and economic losses, cognitive deficits, treatment resistance, and multiple medical and psychiatric comorbidities. These and other data indicate that treatment after a first episode must be more intensive, multimodal, and continuous and include expert psychopharmacological and psychosocial support, as well as family education and support. Intensive treatment like this can be life-saving. The current study also supports the mantra we have espoused: prevent episodes, protect the brain and the person.
Cannabis May Produce More Brain Changes in Teens with Bipolar Disorder than in Healthy Teens
At the 2019 meeting of the International Society for Bipolar Disorders, researcher Benjamin Goldstein of Sunnybrook Research Institute in Toronto reported that adolescents with bipolar disorder who smoked marijuana had greater deficits in certain brain areas than did adolescents who did not have bipolar disorder. The areas affected included the dorsal lateral and rostral middle frontal cortex, and middle cortex. Goldstein concluded, “Adolescents with [bipolar disorder] may be particularly sensitive to the neurostructural effects of cannabis.”
Marijuana in general causes adverse changes in brain structure and cognition and vulnerability to paranoia and psychosis. Heavy use in adolescence is associated with an increased incidence of the onset of bipolar disorder and schizophrenia. The Goldstein data suggest several possible causal mechanisms. Those with bipolar disorder may already have brain abnormalities that are exacerbated by marijuana use. Alternatively, marijuana and bipolar disorder together may impact brain structure more than either factor alone would.
Obesity Associated with Inflammation and Brain Abnormalities
At the 2019 meeting of the International Society for Bipolar Disorders, researcher David J. Bond reviewed the data on the multiple adverse effects of obesity in patients with bipolar disorder. These include increased cardiovascular risk, poorer response to treatment, brain abnormalities, and decreased cognitive function, which is correlated with the degree of overweight.
Editor’s Note: These data emphasize the importance of starting a nutritious diet early in life and sustaining it through adulthood, avoiding the drugs most associated with weight gain such as clozapine and olanzapine, and facilitating weight loss with drugs. There are several treatments that can aid in weight loss. One is the diabetes treatment metformin, starting at a high dose of 500mg twice daily, and increasing to 1000mg twice daily if tolerated. The anticonvulsants topiramate or zonisamide also promote weight loss. The most effective option is a combination of the antidepressant bupropion sustained release (at a dose of 150–300mg) plus the anti–substance abuse drug naltrexone (50mg). This combination was associated with a loss of 10% of body weight over 12 weeks in women with diabetes.
Blood and Now Brain Inflammation Linked to Depression
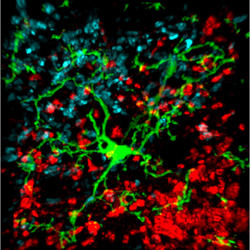 There is growing evidence of a link between inflammation of depression. At the 2015 meeting of the Society of Biological Psychiatry, researcher Jeff Meyer summarized past studies on inflammatory markers. These are measurements, for example of certain proteins in the blood, that indicate the presence of inflammation in the body.
There is growing evidence of a link between inflammation of depression. At the 2015 meeting of the Society of Biological Psychiatry, researcher Jeff Meyer summarized past studies on inflammatory markers. These are measurements, for example of certain proteins in the blood, that indicate the presence of inflammation in the body.
Common inflammatory markers that have been linked to depression include IL-6, TNF-alpha, and c-reactive protein. At the meeting, Meyer reviewed the findings on each of these. Twelve studies showed that IL-6 levels are elevated in the blood of patients with depression. Four studies had non-significant results of link between IL-6 and depression, and Meyer found no studies indicating that IL-6 levels were lower in those with depression. Similarly, for TNF-alpha, Meyer found 11 studies linking elevated TNF-alpha with depression, four with non-significant results, and none showing a negative relationship between TNF-alpha and depression. For c-reactive protein, six studies showed that c-reactive protein was elevated in people with depression, six had non-significant results, and none indicated that c-reactive protein was lower in depressed patients.
Most studies that have linked inflammation to depression have done so by measuring inflammatory markers in the blood. It is more difficult to measure inflammation in the brain of living people, but Meyer has taken advantage of new developments in positron emission tomography (PET) scans to measure translocator protein binding, which illustrates when microglia are activated. Microglial activation is a sign of inflammation. Translocator protein binding was elevated by about 30% in the prefrontal cortex, anterior cingulate cortex, and insula in study participants who showed symptoms of a major depressive episode compared to healthy control participants. The implication is that the depressed people with elevated translocator protein binding have more brain inflammation, probably via microglial activation.
The antibiotic minocycline reduces microglial activation. It would be interesting to see if minocycline might have antidepressant effects in people with depression symptoms and elevated translocator protein binding.
RTMS Can Increase Amygdala Connectivity
 Regulation of the amygdala (the brain’s emotional center), particularly through its interaction with the ventral anterior cingulate cortex, has been implicated in the experience of fear in animals, and anxiety and depression in humans. Connectivity between the two structures is critical for emotion modulation. Repeated transcranial magnetic stimulation (rTMS) is a method of stimulating outer regions of the brain with magnets. Researchers Desmond Oathes and Amit Etkin are investigating whether rTMS can also be used to influence these deeper brain areas, or their interaction with each other.
Regulation of the amygdala (the brain’s emotional center), particularly through its interaction with the ventral anterior cingulate cortex, has been implicated in the experience of fear in animals, and anxiety and depression in humans. Connectivity between the two structures is critical for emotion modulation. Repeated transcranial magnetic stimulation (rTMS) is a method of stimulating outer regions of the brain with magnets. Researchers Desmond Oathes and Amit Etkin are investigating whether rTMS can also be used to influence these deeper brain areas, or their interaction with each other.
The researchers’ study used single-pulse probe TMS delivered at a rate of 0.4 Hz at 120% of each participant’s motor threshold, targeted at the anterior or posterior medial frontal gyrus on either side of the brain. The researchers also used functional magnetic resonance imaging (fMRI) of the whole brain to observe connectivity between different sections.
RTMS to the right side of the medial frontal gyrus increased connectivity between the amygdala and the ventral anterior cingulate cortex more than stimulation to the left side. Stimulation of the posterior portion of the medial frontal gyrus increased connectivity more than stimulation of the anterior portion.
Editor’s Note: These data indicate that rTMS can alter brain activity in these deeper regions and can influence inter-regional connectivity. This is important because abnormalities in the connectivity of brain regions have increasingly been found in patients with mood disorders. Oathes and Etkin hope that these findings can be applied to others and that rTMS can be used to correct patterns of regional connectivity in the brain in order to improve emotion regulation.
The Nucleus Accumbens in Depression
Brain-derived neurotrophic factor (BDNF) keeps neurons healthy and is critical for long-term memory and synapse formation. BDNF levels increase in the nucleus accumbens (the brain’s reward center) and decrease in the hippocampus during clinical depression and chronic cocaine use. In rodents, the same changes in BDNF levels occur during defeat stress (which resembles human depression).
Rodents who are repeatedly defeated by a larger rodent exhibit behaviors such as social withdrawal, lethargy, and decreased interest in sucrose. The increases in BDNF in the nucleus accumbens of these rodents could reflect the learning that takes place during the repeated defeat stress and the depression-like behaviors that follow it. Blocking the BDNF increases in the nucleus accumbens prevents these behaviors from developing.
Chadi Abdallah and other researchers at Yale University recently found that the left nucleus accumbens of patients with treatment-resistant depression is enlarged compared to normal controls, and the drug ketamine, which produces rapid-onset antidepressant effects, rapidly decreases the volume of the nucleus accumbens in the depressed patients. The mechanism by which it does so is unknown, but could reflect some suppression of the depressive learning.
Any relationship between the volume of the nucleus accumbens and its levels of BDNF is unknown, but ketamine’s effect on the size of this brain region could be linked to a decrease in the defeat-stress memories.
Youth at High Risk for Bipolar Disorder Show White Matter Tract Abnormalities
 At a recent scientific conference, researcher Donna Roybal presented research showing that children at high risk of developing bipolar disorder due to a positive family history of the illness had some abnormalities in important white matter tracts in the brain. Prior to illness onset, there was increased fractional anisotropy (FA), a sign of white matter integrity, but following the onset of full-blown bipolar illness there were decreases in FA.
At a recent scientific conference, researcher Donna Roybal presented research showing that children at high risk of developing bipolar disorder due to a positive family history of the illness had some abnormalities in important white matter tracts in the brain. Prior to illness onset, there was increased fractional anisotropy (FA), a sign of white matter integrity, but following the onset of full-blown bipolar illness there were decreases in FA.
Roybal postulated that these findings show an increased connectivity of brain areas prior to illness onset, but some erosion of the white matter tracts with illness progression.
Editor’s Note: It will be critical to replicate these findings in order to better define who is at highest risk for bipolar disorder so that attempts at prevention can be explored.
Adolescent Obesity Connected to Brain Impairment
As childhood obesity has increased over the past several decades, the metabolic syndrome has also become more prevalent among children and adolescents. The metabolic syndrome consists of five measures related to obesity: elevations in fasting glucose levels or insulin resistance, a high proportion of LDL (“bad” cholesterol) to HDL (“good” cholesterol), elevated triglycerides, hypertension, and abdominal obesity or high waist circumference. A patient with three of these abnormalities would be diagnosed with the metabolic syndrome.
In adults, the metabolic syndrome has been associated with neurocognitive impairments. Researchers decided to look at adolescents with the metabolic syndrome to determine whether these brain effects are a result of long-term metabolic impairment or whether they can take place after short-term periods of poor metabolism as well. In a study published by Yau et al. in the journal Pediatrics last year, 49 adolescents with the metabolic syndrome were compared to 62 adolescents without the syndrome who had been matched for similar age, socioeconomic status, school grade, gender, and ethnicity.
The adolescents with the metabolic syndrome had lower scores on tests of math, spelling, attention, and mental flexibility, as well as a trend for lower overall intelligence. In brain measures such as hippocampal volume, amount of brain cerebrospinal fluid, and microstructural integrity in white matter tracts, the seriousness of the metabolic syndrome correlated with the level of abnormality on these measures.
Editor’s Note: It seems as though even short-term problems with metabolism can lead to brain impairments like lower cognitive performance and decreased integrity of brain structures. These effects are even seen before vascular disease and type 2 diabetes are manifest.
It is doubly important, in terms of both cardiovascular and neurobiological risks, to look out for one’s medical and psychiatric health. Reducing the abnormal components of the metabolic syndrome should produce benefits for both the cardiovascular system and the central nervous system.
Almost 40% of patients with bipolar illness in the US have the metabolic syndrome, so considerable effort will be required to improve this public health crisis.
Adolescent Brain Particularly Susceptible to Decline in IQ from Marijuana Use
 A decades-long study in New Zealand suggests that people who use marijuana persistently during adolescence lose 8 IQ points by adulthood compared to their peers who never use marijuana. Quitting or reducing cannabis use after adolescence did not restore the intellectual abilities in those who used it persistently in their youth. This is the first study of its kind that controlled for differences in functioning that existed before adolescence.
A decades-long study in New Zealand suggests that people who use marijuana persistently during adolescence lose 8 IQ points by adulthood compared to their peers who never use marijuana. Quitting or reducing cannabis use after adolescence did not restore the intellectual abilities in those who used it persistently in their youth. This is the first study of its kind that controlled for differences in functioning that existed before adolescence.
Participants took part in neuropsychological testing at the age of 13, prior to any cannabis use, and then were periodically interviewed about their use of the drug (at the ages of 18, 21, 26, 32, and 38). At age 38 they underwent IQ testing again.
Although persistent cannabis users tended to have fewer years of education, the lack of education was not responsible for the difference in adult IQ.
Those participants who only began using cannabis persistently in adulthood did not see a decline in IQ, suggesting that the adolescent brain is particularly susceptible to damage from cannabis use.
White Matter Abnormalities in the Brain Predict Onset of Psychosis
 At the 2012 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP), Carrie E. Bearden presented data from a study that predicted conversion to psychosis in at-risk youth (those who have prodromal symptoms or a particular genetic mutation that leads to psychosis) by observing white matter abnormalities.
At the 2012 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP), Carrie E. Bearden presented data from a study that predicted conversion to psychosis in at-risk youth (those who have prodromal symptoms or a particular genetic mutation that leads to psychosis) by observing white matter abnormalities.
Bearden found that the degree of white matter abnormality seen during magnetic resonance imaging (MRI) was proportional to the degree of cognitive deficit in patients who subsequently developed a first episode of psychosis. The white matter abnormalities were seen particularly in the superior longitudinal fasciculus (SLF) and were associated with increased severity of symptomatology. The overall degree of white matter alteration was also significantly related to clinical outcome 15 months later.
Editor’s Note: The SLF is a major neuronal conduit between prefrontal cortical systems, which are responsible for cognition and planning, and the parietal cortex, which is responsible for spatial abilities. Disruption of this fiber track has been related to difficulties in social cognition and “theory of mind” concepts, like inferring what others might be thinking.