Tricyclic Antidepressants Linked to Cardiovascular Disease
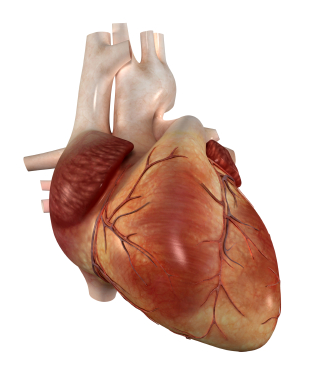 Research from 2010 shows that tricyclic antidepressants (TCAs) are linked to 35% greater risk for cardiovascular disease, while selective serotonin reuptake inhibitors (SSRIs) were not shown to confer any extra cardiovascular risks.
Research from 2010 shows that tricyclic antidepressants (TCAs) are linked to 35% greater risk for cardiovascular disease, while selective serotonin reuptake inhibitors (SSRIs) were not shown to confer any extra cardiovascular risks.
Editor’s Note: This is another one of many reasons to use second generation antidepressants such as the SSRIs and bupropion instead of the first generation tricyclics. The TCAs have more side effects, are more dangerous in overdose, are not indicated for children or adolescents, and are more likely to cause switches into mania in individuals with bipolar disorder than the newer ADs.
Aspirin May Help Reduce Schizophrenia Symptoms
An article by Laan et al. published in the Journal of Clinical Psychiatry in 2010 suggested that aspirin may reduce symptoms of schizophrenia spetrum disorders in patients being treated with antipsychotics.
Aspirin is an anti-inflammatory drug. We’ve written before about the possible use of aspirin in bipolar disorder and about the role of inflammation in mental illness.
Among Bipolar Patients, Women Spend More Time Depressed Than Men Do
An article by Lori Altshuler et al. (including this editor Robert M. Post) published in the American Journal of Psychiatry in 2010 presents research that among bipolar patients studied over a period of 7 years, women spent more time than men depressed. Women had higher rates of rapid cycling and of anxiety disorders, both of which were associated to higher rates of depression.
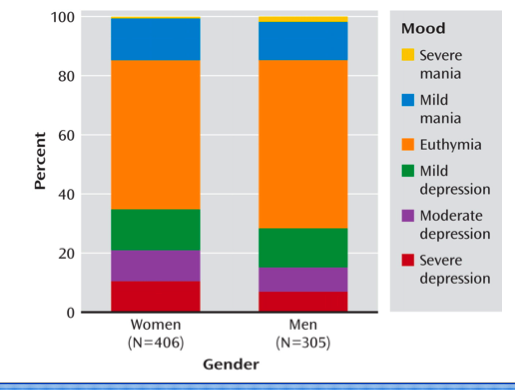
Proportion of Time Spent Ill During Clinical Visits for Women and Men With Bipolar I or II Disorder (N=711)aaWomen and men, 35.6% compared with 28.7% of visits depressed; 50.4% compared with 56.9% of visits euthymic; 14.1% compared with 14.4% of visits hypomanic or manic.
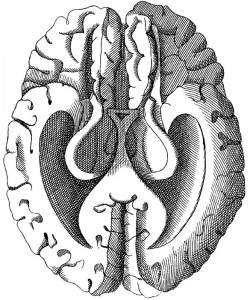
Exercise Good for Learning and Memory in Children and the Elderly
Another article in the Telegraph today suggests that aerobic exercise can increase the size of the hippocampus in elderly people and lead to improvements in memory, attention, and ability to multi-task. Children who were more fit were also better at multitasking. Art Kramer of the Beckman Institute for Advanced Science and Technology at the University of Illinois said,
“It is aerobic exercise that is important so by starting off doing just 15 minutes a day and working up to 45 minutes to an hour of continuous working we can see some real improvements in cognition after six months to a year.
“We have been able to do a lot of neuroimaging work alongside our studies in the elderly and show that brain networks and structures also change with exercise.
More Support for the Connection Between Exercise and Cognition
We recently wrote about a study that suggested exercise may improve cognition function in depression. In today’s New York Times, an article suggests that in mice, exercise expanded the brain’s capacity to store energy, a process known as supercompensation.
While a brain with more fuel reserves is potentially a brain that can sustain and direct movement longer, it also “may be a key mechanism underlying exercise-enhanced cognitive function,” says Hideaki Soya, a professor of exercise biochemistry at the University of Tsukuba and senior author of the studies, since supercompensation occurs most strikingly in the parts of the brain that allow us better to think and to remember. As a result, Dr. Soya says, “it is tempting to suggest that increased storage and utility of brain glycogen in the cortex and hippocampus might be involved in the development” of a better, sharper brain.
Sleep Apnea Common Among Rapid Cyclers
Kellen and colleagues presented a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, in which they reported that 21% of patients with rapid cycling bipolar disorder have confirmed sleep apnea. Since many patients who screened positive for sleep apnea on the study’s sleep questionnaire did not undergo follow-up sleep studies to confirm the diagnosis, it is estimated that up to 40% of rapid cycling patients may, in fact, have sleep apnea.
Editor’s note: Given such a high incidence of sleep apnea among rapid cycling bipolar patients, it would be prudent for patients and clinicians to be alert to the possibility of sleep apnea and follow up with appropriate sleep studies. Sleep apnea can cause daytime fatigue, cognitive dysfunction, and treatment resistance, so its identification and treatment with continuous positive airway pressure (CPAP) may be enormously beneficial to a substantial number of rapid cycling bipolar patients. A just-published article by Sukys-Claudino in Sleep Medicine presents findings that compared to placebo, the anti-Alzheimer’s drug donepezil (Aricept) started at 5mg/day for 2 weeks and then increased to 10 mg given twice a day (20 mg/day total) helped all measures of sleep apnea including daytime sleepiness.
Clinical hints that a patient may be suffering from sleep apnea include loud snoring, long pauses between breaths, and non-restorative sleep. The likelihood of sleep apnea increases with age and with overweight or obesity.
Common Genetic Variation Linked to Response to Antidepressants
 Brain-derived neurotrophic factor (BDNF) protects neurons and is important for long-term learning and memory. There are several genetic variations in BDNF depending on which amino acid—valine or methionine—falls at a particular position when the proBDNF protein is being made. Most people have the val-66-val allele, some have the val-66-met, and a few have the met-66-met allele.
Brain-derived neurotrophic factor (BDNF) protects neurons and is important for long-term learning and memory. There are several genetic variations in BDNF depending on which amino acid—valine or methionine—falls at a particular position when the proBDNF protein is being made. Most people have the val-66-val allele, some have the val-66-met, and a few have the met-66-met allele.
Researcher Jessica C. Levenson, working with David Kupfer and Ellen Frank at the University of Pittsburgh, reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011 that patients with unipolar depression who have the val-66-val allele of proBDNF have better clinical responsiveness to antidepressants than those with the slightly less common variant, val-66-met.
Editor’s note: The val-66-val allele is more effective in enhancing synaptic plasticity and is more easily transported from the nucleus to the dendrites of neurons (where it is necessary for learning and memory) than the val-66-met allele or the least effective met-66-met variant.
These findings are intriguing because antidepressant treatments tend to increase BDNF, regardless of their mechanisms of action. Moreover, BDNF levels are low in patients with depression, usually in direct relationship to the severity of depression. Thus, the ability of antidepressants to increase BDNF may lead to a more effective treatment response in those with the better functioning val-66-val allele of BDNF. This remains to be further documented, but the study provides a preliminary example of how genotyping may eventually be able to help predict individual clinical response to a given treatment and thus foster the development of personalized medicine.
Neurological Biomarkers May Eventually Predict Response to Antidepressants
 T.L. Lauriat reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011 that low baseline levels of the neurotransmitter GABA in the brains of depressed patients were associated with greater response to antidepressants. GABA was measured using magnetic resonance spectroscopy (MRS).
T.L. Lauriat reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011 that low baseline levels of the neurotransmitter GABA in the brains of depressed patients were associated with greater response to antidepressants. GABA was measured using magnetic resonance spectroscopy (MRS).
These data raise the possibility that easily observed neurobiological markers, such as levels of GABA or the neurotransmitter glutamate, may ultimately be helpful in predicting clinical response to particular treatments.
Biomarker Panel May Help Diagnose Major Depressive Disorder
It is hoped that measuring biochemical substances in blood will help in the diagnosis of mood disorders and help direct patients to the most effective therapeutic regimens. J.L. Billbielo reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011 that investigators from Ridge Diagnostics in North Carolina were using this type of biomarker panel in an attempt to provide a predictive algorithm for a diagnosis of major depressive disorder. The panel of 10 assays was derived from a larger screening set and included: alpha 1 antitrypsin (Alpha 1AT), brain-derived neurotrophic factor (BDNF), cortisol, epidermal growth factor (EGF), resistin, and soluble tumor necrosis factor receptor II (sTNFR2). The research group found that this optimized algorithm distinguished depressed subjects from normal controls with a sensitivity of approximately 90% and a sensitivity of 84%.
Editor’s note: This assay is available commercially and appears to represent an interesting panel of potential neurobiological markers of depression, including neurotrophic factors, endocrine stress hormones, and inflammatory markers. While its diagnostic utility is somewhat doubtful and must be further demonstrated, this editor hopes that similar panels could ultimately predict individual clinical response to a given treatment. For example, patients with high levels of inflammatory markers might respond better to treatments aimed at suppressing inflammation. Read more
Antioxidants May Be Deficient in Patients with Bipolar Disorder, NAC May Help
In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Guy Goodwin and colleagues reported that relative to controls, blood from patients with bipolar disorder contained more total glutathione, a potent antioxidant, and a higher ratio of oxidized to reduced glutathione. Measurements of blood glutathione could eventually serve as a biomarker, suggesting when a diagnosis of bipolar disorder is likely.
Editor’s note: Glutathione is one of the major antioxidants in humans. Oxidized glutathione is a less active form, so the higher levels of oxidized glutathione compared to reduced glutathione in patients with bipolar disorder suggests they may have a relative deficiency of the active form. These data are consistent with reports that patients in manic and depressive phases of bipolar disorder have increased oxidative stress and free radicals that impair cellular functioning.
Together, these results highlight the potential utility of treatments that increase antioxidant activity. One option is N-acetylcysteine (NAC), which the body converts into glutathione. As previously noted in the BNN, Michael Berk reported in Biological Psychiatry in 2008 that NAC (1000 mg twice a day) appears to exert greater antidepressant effects over a period of 24 weeks than placebo when added into previously ineffective regimens in patients with bipolar disorder.
In another poster at the conference, Magalhaes and colleagues reported on NAC treatment for a subgroup of the bipolar patients in the study by Berk who were in a major depressive episode at the time of the study. They found that NAC had highly significant acute antidepressant effects of large magnitude in this subgroup of patients.
The glutathione data by Goodwin et al. provide a further rationale for consideration of the use of NAC in bipolar disorder, particularly in the acute and longer-term treatment of the depressive phases. As we reported in BNN Issue 1 from 2010, NAC also exerts positive effects in many illnesses that commonly occur comorbidly with bipolar disorder. These include cocaine and heroin addiction, gambling addiction, obsessive compulsive disorder (as an adjunct to selective serotonin reuptake inhibitors (SSRIs)), and trichotillomania (compulsive hair-pulling).