Early Antidepressant Use is Associated with Rapid Cycling Bipolar Disorder
Highlights from Posters Presented at the Society of Biological Psychiatry Meeting, April 27-29, 2023 in San Diego
A.C. Courtes and Jair Soares reported that “Antidepressants were prescribed as the first psychiatry medication in 74/114 (65%) of BD patients.” This and alcohol use disorder were independent predictors of rapid cycling.
Link Between Childhood Trauma and Difficult Course of Bipolar Disorder Clarified
A collaboration between Norwegian and French researchers led by Bruno Etain has clarified the pathway by which childhood trauma is linked to worse outcomes among people with bipolar disorder. The researchers, who presented their work in a poster at the 2015 meeting of the Society of Biological Psychiatry, replicated earlier findings by this editor (Robert Post) that patients who experienced trauma as a child had a more adverse course of bipolar disorder. Etain and colleagues found a link between childhood trauma and an earlier age of onset of bipolar disorder, rapid cycling, suicide attempts, and cannabis misuse.
The researchers identified more than 550 patients with bipolar disorder, who answered questionnaires about their history of bipolar disorder and childhood trauma. Their DNA was also analyzed, and the researchers found that the effect of childhood trauma on age of onset was mediated by the presence of common genetic variants in proteins related to stress (the serotonin transporter) and immune function (Toll-like receptors). They also found that the traits of mood lability (or moodiness) and impulsivity mediated the effects of trauma on clinical outcomes.
The lasting epigenetic effects of child maltreatment and adversity noted in the above abstract are consistent with a large literature showing more epigenetic effects in these individuals than in controls. While genetics are important, the impact of the environment is also substantial.
Lamotrigine Not Helpful as Add-on to Lithium and Valproate in Rapid Cycling Bipolar Disorder
 A 2012 study by Kemp et al. in the journal Bipolar Disorders found that lamotrigine added to combination treatment with lithium and valproate was no more effective than placebo in patients with rapid cycling bipolar disorder. Only 14% (19 out of 133) of rapid cycling patients stabilized upon initial treatment with the open combination of lithium and valproate, a startlingly low rate. In the next phase of the study, 49 patients who were not stabilized were given adjunctive treatment with either lamotrigine (n=23) or placebo (n=26) on a double-blind basis, but no significant difference was observed.
A 2012 study by Kemp et al. in the journal Bipolar Disorders found that lamotrigine added to combination treatment with lithium and valproate was no more effective than placebo in patients with rapid cycling bipolar disorder. Only 14% (19 out of 133) of rapid cycling patients stabilized upon initial treatment with the open combination of lithium and valproate, a startlingly low rate. In the next phase of the study, 49 patients who were not stabilized were given adjunctive treatment with either lamotrigine (n=23) or placebo (n=26) on a double-blind basis, but no significant difference was observed.
Editor’s Note: This study has two pieces of not-so-good news. The first is that it was so difficult to stabilize these patients with rapid cycling bipolar disorder. The second is that the add-on of lamotrigine, which is highly effective in the prevention of depressions in bipolar disorder, was in this case no more effective than placebo.
This study again demonstrates that rapid cycling bipolar disorder is difficult to treat, and even the use of three proven mood stabilizers in combination is not always effective. Many doctors would recommend an atypical antipsychotic as the next clinical option.
The Unfolding Story of Poor Response to Antidepressants in Bipolar Depression
The role of the traditional antidepressants in the treatment of depression in bipolar illness remains controversial. Despite mounting evidence that they are not efficacious in the treatment of bipolar depression, they are still among the most widely used treatments for that condition. At the first biennial conference of the International Society for Bipolar Disorders held in Istanbul this past March, Mark A. Frye and Shigenobu Kanba chaired a symposium on antidepressant-induced mania and individualized treatment for bipolar depression.
This editor (Robert M. Post) discussed factors influencing antidepressants’ effects on patients with bipolar depression. In a recent meta-analysis, researchers Sidor and MacQueen reviewed data from studies encompassing 2373 patients with bipolar depression and found that antidepressants had no significant benefits over placebo on measures of response or remission. Pooled estimates for a thousand patients showed no increase in patients’ risk of switching into mania after treating with antidepressants. However, in a smaller sub-analysis, the risks of switching into mania following treatment with the older tricyclic antidepressants (43%) and venlafaxine (15%) was greater than the risk of switching after being treated with SSRIs (7%) or bupropion (5%).
There is a conundrum in the literature. While antidepressants don’t work very well in bipolar depression, there is a small subgroup of patients who, having responded well to antidepressants for two months, benefit more from continuing the antidepressant treatment than from discontinuing the drug. Continued treatment with adjunctive antidepressants (added to regular treatment with a mood stabilizer or an atypical antipsychotic) was associated with fewer relapses into depression over the next year when the antidepressants were continued compared to when they were discontinued. Lori Altshuler et al. have published two uncontrolled studies to this effect, Russell Joffe et al. have published one, and a more recent randomized study of this by Nassir Ghaemi replicated some of the results in patients who had non-rapid-cycling bipolar disorder. At the same time, the literature shows that there are number of risk factors for switching into hypomania during antidepressant treatment in bipolar depression.
Risk factors for switching into mania upon treatment with an antidepressant include: younger age, bipolar I compared to bipolar II, rapid cycling in the past year, mixed depression, use of older tricyclic antidepressants compared to newer second-generation antidepressants, use of noradrenergic active antidepressants compared to those that act on serotonin or dopamine, and a history of substance abuse. Read more
Among Bipolar Patients, Women Spend More Time Depressed Than Men Do
An article by Lori Altshuler et al. (including this editor Robert M. Post) published in the American Journal of Psychiatry in 2010 presents research that among bipolar patients studied over a period of 7 years, women spent more time than men depressed. Women had higher rates of rapid cycling and of anxiety disorders, both of which were associated to higher rates of depression.
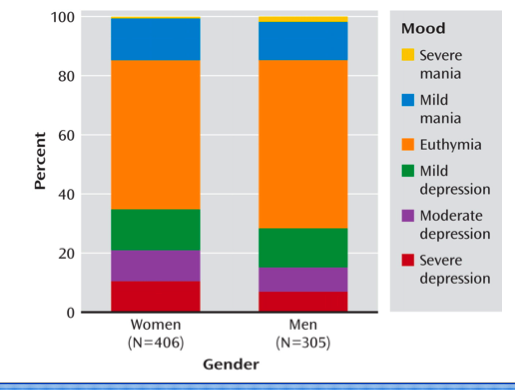
Proportion of Time Spent Ill During Clinical Visits for Women and Men With Bipolar I or II Disorder (N=711)aaWomen and men, 35.6% compared with 28.7% of visits depressed; 50.4% compared with 56.9% of visits euthymic; 14.1% compared with 14.4% of visits hypomanic or manic.
Sleep Apnea Common Among Rapid Cyclers
Kellen and colleagues presented a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, in which they reported that 21% of patients with rapid cycling bipolar disorder have confirmed sleep apnea. Since many patients who screened positive for sleep apnea on the study’s sleep questionnaire did not undergo follow-up sleep studies to confirm the diagnosis, it is estimated that up to 40% of rapid cycling patients may, in fact, have sleep apnea.
Editor’s note: Given such a high incidence of sleep apnea among rapid cycling bipolar patients, it would be prudent for patients and clinicians to be alert to the possibility of sleep apnea and follow up with appropriate sleep studies. Sleep apnea can cause daytime fatigue, cognitive dysfunction, and treatment resistance, so its identification and treatment with continuous positive airway pressure (CPAP) may be enormously beneficial to a substantial number of rapid cycling bipolar patients. A just-published article by Sukys-Claudino in Sleep Medicine presents findings that compared to placebo, the anti-Alzheimer’s drug donepezil (Aricept) started at 5mg/day for 2 weeks and then increased to 10 mg given twice a day (20 mg/day total) helped all measures of sleep apnea including daytime sleepiness.
Clinical hints that a patient may be suffering from sleep apnea include loud snoring, long pauses between breaths, and non-restorative sleep. The likelihood of sleep apnea increases with age and with overweight or obesity.
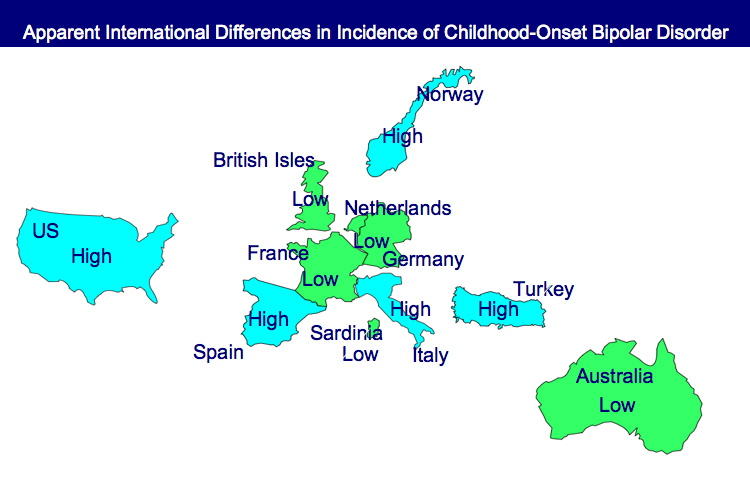
Bipolar Disorder Worse in US than Europe
New research shows that there are more early onsets of illness and more difficult courses of bipolar illness in the US than in the Netherlands or Germany.
This editor was invited to give a plenary presentation at the 4th Biennial Conference of the International Society for Bipolar Disorders in Sao Paulo, Brazil in March. The talk, titled “A greater incidence of early onset bipolar illness and poor prognosis factors in patients in the US compared with those in The Netherlands and Germany,” was based on studies in our Bipolar Collaborative Network.
We found that patients who were studied and treated at four sites in the US (Los Angeles, Dallas, Cincinnati, and Bethesda) had more poor-prognosis factors and indices of difficult courses of bipolar illness compared with patients studied in the same fashion at three sites in Utrecht, the Netherlands and Freiberg and Munich, Germany. We presented some of these data in a preliminary report in the British Journal of Psychiatry in 2008 and further analyzed these data for an article published last year in the Journal of Clinical Psychiatry. Read more