Safety of Atypical Antipsychotics in Pregnancy
A 2017 article in the Journal of Clinical Psychiatry systematically reviewed data on the risks related to schizophrenia, bipolar disorder, and treatment with atypical antipsychotic medication during pregnancy. The article by researcher Sarah Tosato and colleagues suggests that a mother’s illness may be more harmful to a fetus than treatment for that illness is.
The review analyzed 49 articles about illness-related and atypical antipsychotic–related risks in bipolar disorder and schizophrenia. Tosato and colleagues found that abrupt discontinuation of treatment led to a high risk of relapse in pregnant women with bipolar disorder or schizophrenia.
Schizophrenia was linked to a slight increase in obstetric complications for mothers, while both bipolar disorder and schizophrenia were linked to a slight increase in complications for newborns. Mothers ill with schizophrenia had the highest risk for serious complications, including stillbirth, neonatal or infant death, and intellectual disability in the child.
The researchers reported that untreated bipolar disorder and schizophrenia are risk factors for birth defects, but use of atypical antipsychotics is not. Children’s neurodevelopment also does not seem to be affected by mothers’ use of atypical antipsychotics during pregnancy.
The authors suggest that, given parents agree and understand any risks involved, the least harmful choice of action is to maintain treatment of women with bipolar disorder and schizophrenia during pregnancy at the safest minimum dosage to keep their illness at bay.
Birth Defects from Valproate Lower in Bipolar Disorder than in Epilepsy
 The anticonvulsant valproate increases the risk of serious birth defects in fetuses exposed to it. However, a 2017 report by ANSM, France’s agency for health and product safety, and its national insurance fund for employed workers shows that these risks are lower for women taking valproate for bipolar disorder than for women taking valproate for epilepsy.
The anticonvulsant valproate increases the risk of serious birth defects in fetuses exposed to it. However, a 2017 report by ANSM, France’s agency for health and product safety, and its national insurance fund for employed workers shows that these risks are lower for women taking valproate for bipolar disorder than for women taking valproate for epilepsy.
In France, the risk of a major fetal malformation was 10.2 per 1000 women in the general population, about twice that (22.2 per 1000) in women taking valproate for bipolar disorder, and about 4 times higher (46.5 per 1000) in women taking valproate for epilepsy. The authors suggest that treatment for bipolar disorder may be more likely to be interrupted during pregnancy, and this could explain the different levels of risk by diagnosis.
Among the risks of defects in the fetuses of women being treated with valproate for epilepsy, the risk of a ventricular septal defect (a hole in the wall separating the lower heart chambers) was 11.2% compared to 2.7% in fetuses not exposed to valproate, while risk of an atrial septal defect (a hole in the wall separating the upper heart chambers) was 19.1% in the fetuses of those prescribed valproate for epilepsy compared to 1.9% in unexposed fetuses. Risk of hypospadias (placement of the urethra opening on the underside of the penis rather than its end) was 22.7% compared to 4.8% in the general population.
Risks of a major malformation were dose dependent in those with epilepsy (but interestingly, not in those with bipolar disorder), meaning the more valproate patients with epilepsy took, the higher their risk of a fetus with birth defects.
The only birth defects that were more common in the fetuses of women taking valproate for bipolar disorder than in fetuses not exposed to valproate were hypospadias (17.5% risk compared to 4.8% in the general population) and craniostenosis, a deformity of the skull (4.2% risk compared to 0.4% in the general population).
The relative safety of valproate in women being treated for bipolar disorder compared to those being treated for epilepsy is good news for some. However, fetal exposure to valproate has also been linked to deficits in cognitive development.
The risk of spina bifida, which causes lifetime paralysis, in a fetus may no longer be such a catastrophic issue for women taking valproate for bipolar disorder (where the risk did not exceed that of the general population), as was once assumed based on data from women with epilepsy (where the risk is usually 2-4%, but was 8% in this French study). This may be of some comfort to women with bipolar disorder who require valproate treatment to remain stable and wish to become pregnant or in those who experience an unplanned pregnancy.
Antidepressant Use in Pregnancy Does Not Increase Autism Risk
 Two large observational studies published in the journal JAMA in 2017 find no link between antidepressant use during pregnancy and risk of an autism spectrum disorder. Previous studies had suggested a link between the two, but may not have sufficiently accounted for confounding factors. In both new studies, autism rates did not differ between siblings exposed to antidepressants in utero and those who were not exposed.
Two large observational studies published in the journal JAMA in 2017 find no link between antidepressant use during pregnancy and risk of an autism spectrum disorder. Previous studies had suggested a link between the two, but may not have sufficiently accounted for confounding factors. In both new studies, autism rates did not differ between siblings exposed to antidepressants in utero and those who were not exposed.
One of the studies, by researcher Ayesha C. Sujan and colleagues, analyzed exposure to antidepressants in the first trimester and neurodevelopmental outcomes in almost 1.6 million Swedish children. Antidepressant use did slightly increase the chance of a preterm birth, but was not linked to autism spectrum disorder, attention-deficit hyperactivity disorder (ADHD), or small size of the fetus.
The researchers suggested that doctors and patients work together to decide how depression should be treated during pregnancy, based on severity of the depression, treatment history, and access to services.
The other study, by researcher Hilary K. Brown and colleagues, analyzed 36,000 births in Ontario, Canada and found no increased risk of autism spectrum disorder based on antidepressant exposure in utero. The study controlled for 500 characteristics such as mother’s education, age, and health history.
The journal JAMA Pediatrics also published a meta-analysis and review of 10 studies on the subject, finding that a woman’s history of psychiatric disorders weakened any link between antidepressant use during pregnancy and risk of autism spectrum disorder in her children. This implies that the underlying illness, not its treatment, may be responsible if there is any link between depression and autism. The meta-analysis was carried out by researcher Antonia Mezzacappa and colleagues.
Breathing in Through the Nose Enhances Judgment and Memory
A 2016 study published in the Journal of Neuroscience reported that the rhythm of breathing changes electrical activity in the brain and can improve emotional judgments and recall. Breathing in through the nose seemed to produce benefits compared to breathing out or to breathing in through the mouth.
Participants more easily identified a fearful face if they viewed it while breathing in. They also had an easier time remembering objects they observed while breathing in. The effects were not seen if the participants breathed through their mouth.
The researchers, led by Christina Zelano, reported that there was a major difference in brain activity in the amygdala and hippocampus during inhalation versus exhalation. Breathing in, in addition to stimulating the olfactory cortex responsible for smell perception, seems to activate the entire limbic system, the emotional center of the brain.
Breathing-Focused Yoga and Meditation Improved Depression
A 2016 article in the Journal of Clinical Psychiatry reports that Sudarshan Kriya yoga, a breathing-based meditation intervention, improved depression in people who had had an inadequate response to antidepressants.
In the study by researcher Anup Sharma and colleagues, 25 participants were randomized to either receive the breathing-based meditation training right away or be put on a waitlist to receive the training later. After two months, those who received the intervention showed improvement in depression scores compared to those on the waitlist. The intervention also reduced anxiety.
Following Collisions, High School Football Players with No Signs of Concussion May Still Have Neurological Impairment
In a small 2014 study in the Journal of Neurotrauma, researcher Thomas M. Talavaga and colleagues reported that repeated head trauma that did not produce concussion symptoms was still associated with neurocognitive and neurophysiological changes to the brain in high school football players.
The longitudinal study tracked ‘collision events’ experienced by 11 teens who played football at the same high school. The young men also completed neurocognitive testing and magnetic resonance imaging (MRI) scans of their brains over time.
The researchers expected to see the participants fall into two categories: those who had no concussions and normal neurological function, and those who had at least one concussion and subsequent neurological changes. They ended up observing a third group: young men who had not exhibited concussion symptoms, but nonetheless had measurable changes to their neurological functioning, including impairments to visual working memory and altered activation of the dorsolateral prefrontal cortex. Young men in this last group had had more collisions that impacted the top front of the head, directly above the dorsolateral prefrontal cortex.
The authors suggest that the discovery of this third category mean that some neurological injuries are going undetected in high school football players. The players who are injured in this way are not likely to seek treatment, and may continue playing football, risking more neurological brain injury or brain damage with subsequent collisions.
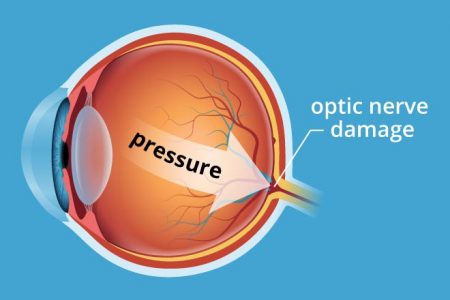
In Mice, Vitamin B3 (Niacin) Prevents Glaucoma
A study published in the journal Science in 2017 reports that adding vitamin B3 to the drinking water of mice prevented them from developing glaucoma. Glaucoma is an age-related condition in which pressure inside the eye damages retinal ganglion cells, the neuronal cells that connect the eye to the brain.
Age contributes both to the buildup of pressure within the eye and to the vulnerability of the neuronal cells to damage. Vitamin B3 seemed to correct the latter problem.
The study by Pete A. Williams and colleagues compared mice with an inherited risk of glaucoma to control mice. Williams and colleagues found that a molecule called NAD that keeps cells functioning normally declined with age, reducing the reliability of the neurons’ energy metabolism.
Vitamin B3 boosted the metabolic reliability of the aging neuronal cells. This helped the cells resist damage from mounting pressure in the eye.
Williams and colleagues also found that a single application of gene therapy with the gene NMNAT1 also prevented glaucoma in the mice. NMNAT1 is the gene for an enzyme that makes NAD from vitamin B3. Gene therapy via an injection in the eye has been approved to treat some rare human eye disorders.
The researchers hope to eventually test vitamin B3 treatment in people with glaucoma and other neurodegenerative disorders.
Editor’s Note: Vitamin B3 may be beneficial for other conditions as well. High-dose niacin (500 mg and up) is a prescription treatment for high cholesterol, and especially the combination of high cholesterol and high triglycerides (blood fats). Niacin may also prevent hardening of the arteries and second heart attacks in men with heart or circulatory problems, and improve diabetes (type 1 and 2). There is some evidence that vitamin B3 can also improve symptoms of osteoarthritis, such as joint stiffness, pain, and swelling. In addition, people who consume more niacin have a lower risk of Alzheimer’s disease, though it is not clear that taking niacin supplements can prevent the illness.
Eating Fresh Fruits and Veggies Can Improve Feelings of Well-Being
A couple weeks of consuming extra fresh fruits and vegetables can improve well-being, according to a 2017 study of 171 young adults. Those who were given two extra daily servings of carrots, kiwis, apples, or oranges reported increases in vitality and motivation after only two weeks.
Interestingly, participants who received text reminders to eat more produce or $10 vouchers to pay for fruits and vegetables did not see the same improvements as those who were given servings of produce directly. Those who got texts or vouchers were more likely to cook extra vegetable servings or mix them into other meals rather than eating additional raw produce.
The authors led by Tamlin Conner suggested that institutional settings such as schools, dormitories, childcare centers, hospitals, and workplaces could make fresh fruits and vegetables easily available to improve general well-being.
Concentrated Blueberry Juice Daily Improves Brain Function
A small study in the journal Applied Physiology, Nutrition, and Metabolism showed an improvement in cognitive function, bloodflow to the brain, and brain activation in older people who drank concentrated blueberry juice every day for 12 weeks.
The 26 participants were healthy adults between the ages of 65 and 77. People who consumed more than 5 daily servings of fruits and vegetables were excluded from the study. Twelve participants consumed 30mL (less than a quarter cup) of the concentrated juice each day, while the other 14 received a daily placebo instead.
The participants did a variety of cognitive tests before and after the study period. Magnetic resonance imaging (MRI) scans collected information about bloodflow and brain function during these tests.
Participants in the blueberry juice group showed statistically significant increases in brain activity by the end of the study compared to those in the placebo group.
The study was led by researcher Joanna Bowtell.
High-Dose Vitamin D May Improve Cognition More Than Low-Dose Vitamin D
 Vitamin D deficiency has been associated with dementia and cognitive decline, but supplements may help. In a study of 82 healthy individuals with low vitamin D levels, high-dose vitamin D supplements (4000 IU/day) improved visual/nonverbal memory more than did low-dose vitamin D supplements (400 IU/day) over 18 weeks.
Vitamin D deficiency has been associated with dementia and cognitive decline, but supplements may help. In a study of 82 healthy individuals with low vitamin D levels, high-dose vitamin D supplements (4000 IU/day) improved visual/nonverbal memory more than did low-dose vitamin D supplements (400 IU/day) over 18 weeks.
The 2017 study took place in Canada, where short winter days can make it more difficult to get sufficient levels of vitamin D from sunlight. The higher-dose supplements raised blood levels of vitamin D compared with the lower-dose supplements.
Those who received the higher doses performed better at tests of visual memory such as the Pattern Recognition Memory Task and the Paired Associates Learning Task, but their performance on tests of verbal memory was not significantly different from those in the lower-dose group. This suggests that higher vitamin D levels are particularly important to visual/nonverbal memory.
The study by Jacqueline A. Pettersen was published in the journal Experimental Gerontology.