Scopolamine Produces Larger Antidepressant and Antianxiety Effects in Women Than in Men
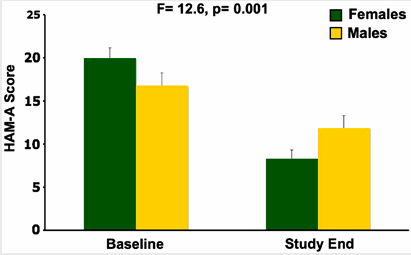
In a study published in Neuropscyhopharmacology, three sessions of intravenous scopolamine (4µg/kg over 15 minutes) led to rapid antidepressant response in both men and women, but the magnitude of response was larger in women. Women also experienced significant reduction in anxiety, as seen below:
Editor’s Note: Scopolamine is a potent blocker of acetylcholine receptors of the muscarinic type. This can cause side effects such as dry mouth and constipation. However, when given intravenously, scopolamine produces rapid onset of antidepressant effects in both bipolar and unipolar depressed patients. This study suggests that the drug may be even more effective in women.
IV Scopolamine Brings About Rapid Onset Of Antidepressant Effects
 Frankel and colleagues from the National Institute of Mental Health presented a randomized, placebo-controlled clinical trial of intravenous (IV) scopolamine for bipolar depression at the 9th International Conference on Bipolar Disorder (ICBD) in 2011. The same group of investigators previously showed that IV scopolamine was able to induce fast-acting antidepressant responses in those with unipolar major depression. This represents a new and independent study exclusively among patients with bipolar depression.
Frankel and colleagues from the National Institute of Mental Health presented a randomized, placebo-controlled clinical trial of intravenous (IV) scopolamine for bipolar depression at the 9th International Conference on Bipolar Disorder (ICBD) in 2011. The same group of investigators previously showed that IV scopolamine was able to induce fast-acting antidepressant responses in those with unipolar major depression. This represents a new and independent study exclusively among patients with bipolar depression.
In the first phase of the study, three sessions of either IV scopolamine at 4 mcg/kg or a sham treatment were scheduled three to five days apart. In the second phase of the study, the patients were switched to the other treatment for three sessions. The results showed a rapid improvement in depression following the first session with scopolamine, more than occurred with the sham treatment. Hamilton Anxiety Rating scale (HAMA) scores also improved more on scopolamine than with the sham treatment, while Young Mania Rating Scores (YMRS) did not differ.
Editor’s note: As previously discussed in the BNN, scopolamine, an antagonist of acetylcholine muscarinic receptors, appears to exert rapid onset antidepressant effects in both unipolar and bipolar depression. When administered intravenously it takes its place with other rapidly acting antidepressant treatments, including IV ketamine, IV thyrotropin releasing hormone (TRH), and one night of sleep deprivation. The new data indicate that both unipolar and bipolar depression can respond rapidly (i.e. within a matter of hours) to certain treatments, even though most conventionally acting antidepressant modalities can take weeks to achieve maximum antidepressant effects. Read more
New Atypical Antipsychotic Lurasidone Has a Good Metabolic Profile
 Andre Pikalov and colleagues from Sunovion Pharmaceuticals Inc. reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011 on the weight and metabolic effects seen in short- and long-term trials of the atypical antipsychotic lurasidone (Latuda) in schizophrenia. The studies compared lurasidone to olanzapine (Zyprexa, at 15mg), haloperidol (Haldol, at 10mg), and placebo. Doses of lurasidone ranged from 20-120mg administered once daily. Short-term treatment for six weeks was associated with changes in weight and metabolic indices similar to those of placebo, while participants taking olanzapine gained substantial amounts of weight and had increases in triglycerides and cholesterol. Changes in glucose and hemoglobin A1C were similar on lurasidone, haloperidol, and placebo, but higher on olanzapine. In the long-term sample, mean weight gain on lurasidone at 12 months was 0.71 kg and metabolic parameters remained relatively unchanged.
Andre Pikalov and colleagues from Sunovion Pharmaceuticals Inc. reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011 on the weight and metabolic effects seen in short- and long-term trials of the atypical antipsychotic lurasidone (Latuda) in schizophrenia. The studies compared lurasidone to olanzapine (Zyprexa, at 15mg), haloperidol (Haldol, at 10mg), and placebo. Doses of lurasidone ranged from 20-120mg administered once daily. Short-term treatment for six weeks was associated with changes in weight and metabolic indices similar to those of placebo, while participants taking olanzapine gained substantial amounts of weight and had increases in triglycerides and cholesterol. Changes in glucose and hemoglobin A1C were similar on lurasidone, haloperidol, and placebo, but higher on olanzapine. In the long-term sample, mean weight gain on lurasidone at 12 months was 0.71 kg and metabolic parameters remained relatively unchanged.
Editor’s note: Multiple posters at the meeting composed a substantial body of evidence concerning acute and long-term studies of lurasidone, which shows that the drug has a weight and metabolic profile relatively similar to placebo and more favorable than that of olanzapine.
Although lurasidone has not been studied acutely or in the long term in patients with bipolar disorder, the safety profile of this drug in schizophrenia indicates that it may eventually be useful for acute and long-term treatment strategies in bipolar disorder. All typical and atypical antipsychotic drugs that have been approved for treatment of schizophrenia have subsequently been shown to have efficacy in acute mania, and given lurasidone’s similar actions in blocking dopamine receptors, there is little reason to expect that this drug will be any different. The results of actual studies of this drug in mania and depression are eagerly awaited.
Aripiprazole Makes Lamotrigine More Effective
 In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Rahman and colleagues reported that in patients being treated for bipolar disorder, the addition of atypical antipsychotic aripiprazole to maintenance treatment with lamotrigine was more effective than the addition of placebo to the same maintenance treatment with lamotrigine. Improvements in Young Mania Rating Scores (YMRS) with the combination of aripiprazole plus lamotrigine were significantly greater than that of lamotrigine plus placebo.
In a poster at the 9th International Conference on Bipolar Disorder (ICBD) held in Pittsburgh in 2011, Rahman and colleagues reported that in patients being treated for bipolar disorder, the addition of atypical antipsychotic aripiprazole to maintenance treatment with lamotrigine was more effective than the addition of placebo to the same maintenance treatment with lamotrigine. Improvements in Young Mania Rating Scores (YMRS) with the combination of aripiprazole plus lamotrigine were significantly greater than that of lamotrigine plus placebo.
Editor’s note: These data add to a growing literature that shows that an atypical antipsychotic added to a mood stabilizer is associated with better prophylactic effects than use of the mood stabilizer alone. Previously, most of the studies of this type of combination used lithium or valproate as the mood stabilizer and, to our knowledge, this is the first to demonstrate that long-term prevention with lamotrigine is enhanced by the addition of an atypical antipsychotic.
Many of the atypical antipsychotics are FDA-approved as adjunctive treatments to mood stabilizers in the long-term treatment of bipolar disorder. The controlled clinical trial data that led to this FDA approval support the practice of many clinicians who prescribe combination treatment rather than monotherapy in order to achieve a more rapid onset of anti-manic stabilization and longer-term maintenance effects. The use of aripiprazole and quetiapine as adjuncts to lithium and valproate is particularly common in bipolar disorder since the same atypical antipsychotics are FDA-approved as adjunctive treatments in unipolar depression, and clinicians are familiar with prescribing them to improve ineffective acute antidepressant treatment.
The Risk-Benefit Ratio Encourages the Use of Antidepressants in Unipolar Depression
Wednesday we reviewed new data that shows that despite the FDA warning that antidepressants can increase suicidal ideation among young people in the first few months they are taken, antidepressants actually reduce acute suicidal ideation and decrease suicidal acts. As we described last year in our article on five myths about antidepressants, antidepressant treatment in recurrent unipolar depression is important to patients’ long-term wellbeing, cognitive functioning, and even life expectancy.
Untreated depression, and particularly untreated recurrent depression, carries high risks not only for lethality by suicide, but also for increases in medical mortality, particularly from cardiovascular disease. In addition to these medical risks, data from many studies suggest that a higher number of prior depressions is associated with increased cognitive dysfunction, and recent large data sets from a case registry in Denmark indicate that patients with four or more prior unipolar or bipolar depressive episodes have double the risk of receiving a diagnosis of dementia in old age. Thus, depressions are dangerous for a patient’s psychological, medical, and cognitive health.
Antidepressants Are Highly Effective in Depression Prevention
In 1992 researcher John Davis completed a meta-analysis of all antidepressant data available at the time in unipolar depression studies and not only found that antidepressant continuation was more effective than placebo in reducing the likelihood of later depressions, but also calculated that the statistical likelihood that this finding was due to chance was minuscule, i.e., p<10-34. John Geddes and colleagues in a meta-analysis in 2003 indicated that there was an approximate 70% reduction in the risk of depressive recurrences with antidepressant continuation compared with discontinuation.
Treatment of a first or second episode of unipolar depression is recommended for six to nine months following achievement of remission. After a third episode, all treatment guidelines of which this editor is aware recommend long-term preventive treatment with antidepressants, particularly if episodes have been severe or close together temporally. This long-term antidepressant continuation for prophylaxis is much like long-term treatment of high blood pressure or high cholesterol recommended for those with or at high risk for cardiovascular disease.
There is some evidence that cognitive behavior therapy reduces the risk for depressive recurrence in those discontinuing antidepressant treatment, but it appears maximally beneficial to engage both psychotherapeutic and pharmacological treatment to prevent future episodes. Read more
Antidepressants Prevent Suicide in Patients with Unipolar Depression
Researcher A. Kahn reported at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in Boca Raton in 2011 that severely depressed and suicidal patients taking citalopram (Celexa) or a combination of citalopram and low dose lithium experienced improvements in depression and suicidal thoughts. This study was unusual because most clinical trials exclude actively suicidal patients. In the group of subjects receiving citalopram plus lithium (300 mg/day and achieving 0.5 mEq/l or higher), there were several indications of better anti-suicide effects than in those on citalopram alone. The authors concluded that with appropriate doses, antidepressants plus lithium may prospectively reduce suicidal thoughts, and that it is possible to conduct clinical trials in severely depressed and suicidal patients if adequate safety measures are included.
Surprisingly, improvement in suicidal ideation preceded improvement in depressed mood per se.
Editor’s note: The study reported here suggests that in those with high suicidal ideation scores at baseline, antidepressants with or without lithium may quickly bring about anti-suicidal effects on thoughts, desires, and behaviors. Whether these effects occur reliably in studies in other groups of patients and in younger individuals remains to be established.
These data are an interesting contrast to data on antidepressant use in those with low levels of suicidality at baseline. A number of studies have suggested that in children and adolescents who were exposed to an antidepressant, a small percentage experienced increases in suicidal ideation in the first two months of treatment compared to patients taking placebo. This led to a Federal Drug Administration (FDA) warning (directed at all patients taking antidepressants) that increases in suicidal ideation and action may occur upon starting antidepressants.
It is important to note that the warning does not refer to completed suicides; the data set that led to the FDA warning included no completed suicides. More than 70% of those with suicidal ideation do not make an attempt, and the vast majority of attempts do not result in a completed suicide.
Most of the studies that found the slight increase in suicidal ideation in some patients after beginning antidepressant treatment actively excluded acutely suicidal patients. Since the study of citalopram and lithium above used a population of severely depressed and suicidal patients and found that antidepressants improved suicidality, it appears important to consider a patient’s baseline state when considering psychiatric interventions. In another example, there is an interesting difference between the way depressed patients and non-depressed normal volunteers respond to one night’s sleep deprivation: depressed patients often show dramatic improvement, while normal volunteers tend to feel worse.
More Evidence that Antidepressants Prevent Suicide in Unipolar Depression
A new study by DeLeon published in the Journal of Clinical Psychiatry in 2011 found that during periods of life when unipolar patients were taking antidepressants (compared to times when they were not taking them) the patients experienced 20% fewer suicidal acts or completed suicides. Read more
Lithium More Effective than Valproate for Bipolar Disorder
 According to two studies in 2011, lithium is more effective in treating episodes of bipolar disorder than valproate, while the drugs may be equally effective in reducing suicidality among bipolar patients.
According to two studies in 2011, lithium is more effective in treating episodes of bipolar disorder than valproate, while the drugs may be equally effective in reducing suicidality among bipolar patients.
The first study, of more than 4000 Danish patients with bipolar disorder, found that patients taking lithium had fewer hospital visits and were less likely to need new medications than those taking valproate. Patients taking lithium had fewer admissions to a hospital for any type of episode. In addition, patients taking valproate had a higher rate of switching to or adding on treatment with antidepressants, antipsychotics, or anticonvulsants than those taking lithium. The study included up to 12 years of follow-up with the patients and is the largest study with the longest period of follow-up of patients taking valproate or lithium to date. Results were published by Lars Kessing et al. in the British Journal of Psychiatry in July 2011.
In the other study, a randomized controlled trial of 100 patients with bipolar disorder who had attempted suicide at least once in the past, Maria Oquendo of Columbia University found that there were no significant differences in number of suicide attempts, hospitalizations for suicide attempts, or time to a new attempt between patients taking lithium and those taking valproate over a follow-up period of 2.5 years.
Forty-five suicide events, which included attempts, hospitalizations, and changes to medication in response to suicide plans, were experienced by 35 patients (16 who were taking lithium and 19 who were taking valproate). Eighteen suicide attempts were made by 6 patients taking lithium and 8 taking valproate. There were no suicide completions during this study, which was published in Volume 168 of the American Journal of Psychiatry in 2011.
Editor’s Note: Suicide attempts are much more common than completed suicides. It appears that the second study was not large enough or long enough to detect differences in the rate of completed suicides. Older naturalistic studies suggest that treatment results in low suicide rates and that in patients who stop treatment with lithium, the rate of suicide attempts and completion increases dramatically. This is another reason for good responders to treatment regimens that include lithium to continue taking their medications.
Exercise May Improve Cognitive Function in Depression
 Tracy L. Greer of the University of Texas Southwestern in Dallas presented an abstract at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011 that suggested that exercise improved the cognitive function of patients being treated with selective serotonin reuptake inhibitors (SSRIs) for major depressive disorder.
Tracy L. Greer of the University of Texas Southwestern in Dallas presented an abstract at the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011 that suggested that exercise improved the cognitive function of patients being treated with selective serotonin reuptake inhibitors (SSRIs) for major depressive disorder.
Thirty-nine participants reported cognitive impairment at baseline. Subjects were randomized to receive antidepressant treatment in the form of an SSRI augmented by either an exercise regimen designed to burn 16 kilocalorie/kg per week (kkw) or one designed to burn 4 kkw. Both exercise regimens resulted in improved response time on a measure of attention, and for the higher intensity (16 kkw) exercise group, there were improvements in response time for visual memory tasks as well as decreased errors on an executive function task.
Editor’s note: There is a somewhat mixed literature on the efficacy of exercise in potentiating antidepressant effects of other treatments. Recent data by Fred Gage and colleagues showed that in animals, exercise increased not only brain-derived neurotrophic factor (BDNF), which seems to be necessary for long-term learning and memory, but also the formation of new neurons (neurogenesis). Gage found that new neurons that migrated to the dentate gyrus of the hippocampus were more excitable than older neurons and were important in a variety of cognitive tasks.
The newer neurons could more precisely distinguish between different stimuli, while the older neurons were sufficient only for discriminating stimuli that were widely and obviously different from each other.
Thus, the increase in new neurons and BDNF that may follow exercise and antidepressant use may be associated with some cognitive improvement in depression, particularly in the realm of response speed and perhaps also in making relatively fine discriminations among relatively similar objects.
While not much evidence for the effect of exercise on cognition has been collected in humans, exercise has many other benefits. Since it is good for cardiovascular fitness and wellbeing, as well as potentially generating new neurons that could play an important role in fine cognitive discriminations, encouraging exercise in depressed patients (especially as their depression improves and they have renewed motivation to engage in exercise regimens) could be of value, even if exercise is not a guaranteed enhancer of antidepressant effects per se.
BDNF Related to Cognition and Fitness in Men with Coronary Artery Disease
 At the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011, Walter Swardfager and colleagues from Toronto, Ontario presented a study indicating that brain-derived neurotrophic factor (BDNF) concentrations in blood are associated with cognitive performance and cardiopulmonary fitness in people with coronary artery disease.
At the 51st Annual Meeting of the National Institute of Mental Health’s New Clinical Drug Evaluation Unit (NCDEU) in 2011, Walter Swardfager and colleagues from Toronto, Ontario presented a study indicating that brain-derived neurotrophic factor (BDNF) concentrations in blood are associated with cognitive performance and cardiopulmonary fitness in people with coronary artery disease.
In 88 mostly male subjects with a mean age of 63 years, cardiopulmonary fitness was directly correlated with BDNF in blood as well as higher scores of cognition on two tests, the mini mental status exam and the digit symbol coding task. The investigators concluded that better fitness, psychomotor processing speed, and overall cognition were consistent with a hypothesis that BDNF protects midbrain dopaminergic neurons against inflammatory neurodegenerative processes.
Blood levels of interleukin 6, a measure of inflammatory cytokines, were associated with lower mini mental status scores in a multivariate analysis that controlled for BDNF levels.
Editor’s note: BDNF appears to be necessary for long-term learning and memory. Meta-analyses indicate that BDNF levels are low in depression and improve with euthymia. Many mood stabilizers including lithium, valproate, carbamazepine, and lamotrigine and most types of antidepressants are able to increase BDNF. The current findings linking BDNF with better cardiopulmonary fitness and cognition continue to emphasize the potential importance of BDNF beyond its role as a marker for depression.
In BNN Volume 12, Issue 3 from 2008, we reported on the data of Schmidt and Duman, which indicated that BDNF administered in a subcutaneous minipump is able to reverse many depressive-like behaviors in an animal model of depression, suggesting that even peripheral BDNF may have a role in the central nervous system.
Low Doses of Levetiracetam Acutely Improve Mild Cognitive Impairment
 Levetiracetam, an anticonvulsant often used to prevent seizures in epilepsy, may improve memory by decreasing hippocampal hyperactivity. Hippocampal hyperactivity in amnestic mild cognitive impairment (aMCI) was once thought to be beneficial, but results from a recent study suggest that increased activity in this structure may contribute to memory impairment. Levetiracetam was effective for memory when given in much lower doses than those used to treat epilepsy.
Levetiracetam, an anticonvulsant often used to prevent seizures in epilepsy, may improve memory by decreasing hippocampal hyperactivity. Hippocampal hyperactivity in amnestic mild cognitive impairment (aMCI) was once thought to be beneficial, but results from a recent study suggest that increased activity in this structure may contribute to memory impairment. Levetiracetam was effective for memory when given in much lower doses than those used to treat epilepsy.
In a study by Michela Gallagher and colleagues presented at the Alzheimer’s Association International Conference in 2011, a placebo-controlled, randomized crossover design was used to collect data from 17 aMCI patients and a similar number of healthy controls. Both groups went through two distinct treatment periods. People in the control group received placebos in both periods, while patients with aMCI received placebo during one period and low-dose levetiracetam (125mg twice daily) in the other period. After 2 weeks of taking the drug, hippocampal hyperactivity among aMCI patients decreased into the normal range, and memory was improved to the level of the healthy controls.
Editor’s Note: The findings from this small study are preliminary and need to be replicated in larger and longer studies before they are applied clinically. As we noted Friday, very low doses of lithium (150mg/day) prevented the progression of mild cognitive impairment compared to placebo in a one-year study. Whether these effects of levetiracetam or lithium are reliable, are of large effect, and occur by similar or different mechanisms remains to be determined.