Newest Meta-Analysis Shows Lithium Is Better than Placebo at Preventing Both Mania and Depression
 A 2004 meta-analysis of previous research showed that lithium was better than placebo at preventing affective episodes and preventing manic episodes. The evidence for the drug’s efficacy in preventing depression was less clear. A new meta-analysis by E. Severus et al. (not yet published) confirms the previous findings and provides new evidence that lithium is also better than placebo at preventing depressions.
A 2004 meta-analysis of previous research showed that lithium was better than placebo at preventing affective episodes and preventing manic episodes. The evidence for the drug’s efficacy in preventing depression was less clear. A new meta-analysis by E. Severus et al. (not yet published) confirms the previous findings and provides new evidence that lithium is also better than placebo at preventing depressions.
The study also suggested that lithium is better than anticonvulsant mood stabilizers at preventing relapse and recurrence, but this finding only reached statistical significance in the prevention of new manic and hypomanic episodes.
Editor’s Note: These findings highlight the desirability of greater lithium use. The drug is currently prescribed less often in the US than it is in Europe. In addition to lithium’s efficacy in the long-term preventative treatment of bipolar disorder, there is evidence that lithium is also the best agent for suicide prevention and for neuroprotective effects.
Jules Angst on the Long-Term Progressive Course of Mood Disorders
At a symposium celebrating the retirement of Willem Nolen, a researcher who spent 40 years studying unipolar and bipolar disorder, from his position at Groningen Hospital in the Netherlands, his colleague Jules Angst discussed some recent findings. Angst is perhaps the world’s leading authority on the long-term course of unipolar and bipolar disorders based on his multiple prospective follow-up studies, some lasting 20-30 years.
The Sensitization-Kindling Model
Angst described evidence that supports the sensitization-kindling model of recurrent mood disorders, which this editor (Robert Post) described in 1992. Episodes tend to recur faster over time, i.e. the well interval between episodes becomes progressively shorter. While stressors often precipitate initial episodes, after multiple occurrences, episodes also begin to occur spontaneously (in the absence of apparent stressors).
This type of progressive increase in response to repetition of the same stimulus was most clearly seen in animal studies, where repeated daily electrical stimulation of the amygdala eventually produced major motor seizures (i.e. amygdala kindling). Daily electrical stimulation of rodents’ amygdala for one second initially produced no behavioral change, but eventually, minor and then full-blown seizures emerged. Once enough of the stimulated full-blown amygdala-kindled seizures had occurred, seizures began to occur spontaneously (i.e. in the absence of the triggering stimulation).
The analogy to human mood disorders is indirect, but kindling provides a model not only for how repeated triggers eventually result in full-blown depressive episodes, but also for how these triggered depressive episodes may eventually occur spontaneously as well.
Long-Term Treatment of Mood Disorders
Angst also discussed long-term treatment of mood disorders. He has found that long-term lithium treatment not only reduces suicides in patients with bipolar disorder, but also reduces the medical mortality that accompanies bipolar disorder.
Angst noted his previous surprising observations that in unipolar disorder, long-term maintenance treatment, even with low doses of tricyclic antidepressants, prevents suicide. Previously, researchers Ellen Frank and David Kupfer of Western Psychiatric Institute and Clinic at the University of Pittsburgh Medical Center had found that when patients with recurrent unipolar depression who had been stable for 5 years on the tricyclic antidepressant nortriptyline were blindly switched to half their original dose, about 90% rapidly relapsed into a new episode of depression. Their data helped establish the prevailing view that maintenance treatment with the full-dose regimen required to achieve a good initial acute response is also the optimal approach to long-term continuation and prophylactic treatment.
Angst found good results even at low doses, but his data may not be in conflict with Frank and Kupfer’s, as a person who responds well acutely to low doses may also be able to maintain good enough response to them to prevent recurrences in the long term.
Incidence of Bipolar Disorder in Adolescents Similar to Incidence in Adults
Angst also presented data from the Adolescent Supplement to the National Comorbidity Study (NCS-A), which analyzed interviews with approximately 10,000 adolescents (aged 13-17) in the US. He found a 7.6% incidence of major depression, a 2.5% incidence of bipolar I or II disorder, and a 1.7% incidence of mania. There was an even higher incidence of sub-threshold bipolar disorder, when there are not enough symptoms or a long enough duration of symptomatology to meet diagnostic criteria for bipolar I or II disorder. These data published by Merikangas et al. in 2009 provide clear epidemiological data that there is a substantial incidence of bipolar disorder in adolescents in the US, roughly similar to that seen in adults.
Long-term Treatment Response in Bipolar Illness
Willem Nolen, a researcher who has spent 40 years studying unipolar and bipolar disorder, recently retired from his position at Groningen Hospital in the Netherlands. In February, his retirement was celebrated with a symposium where he and other researchers discussed some of their important findings from the last several decades.
Nolen recently published a double-blind randomized study showing that in patients who were initially responsive to monotherapy with quetiapine (Seroquel), continuing the drug (at doses of 300-800mg/night) or switching to lithium were both more effective than switching to placebo over 72 weeks of long-term follow-up.
This study shows that quetiapine, which is only FDA-approved for long-term preventative treatment when used in combination with lithium or valproate (Depakote), also has efficacy when used as monotherapy.
Lithium is Highly Effective in Long-term Prevention
Nolen’s work also adds to an impressive amount of literature showing that lithium is highly effective in long-term prevention. This case is especially noteworthy because lithium was effective even in patients who had initially been selected for their response to quetiapine. (Studies that use this kind of “enriched sample” can only claim that quetiapine has long-term efficacy in those patients who initially respond well to the drug.) The data on lithium are even more impressive since the patients in this study were not enriched for lithium response.
Nolen has also conducted multiple studies of lithium, but optimal doses and target blood levels of the drug remain controversial. The therapeutic range of lithium is usually considered to be 0.6 to 1.2 meq/L, but some have argued that lower levels may still be effective. In a new analysis of those patients in the quetiapine study who were switched to lithium treatment, Nolen found that only lithium levels above 0.6 meq/L produced better results than placebo in long-term prophylaxis. Read more
The Risk-Benefit Ratio Encourages the Use of Antidepressants in Unipolar Depression
Wednesday we reviewed new data that shows that despite the FDA warning that antidepressants can increase suicidal ideation among young people in the first few months they are taken, antidepressants actually reduce acute suicidal ideation and decrease suicidal acts. As we described last year in our article on five myths about antidepressants, antidepressant treatment in recurrent unipolar depression is important to patients’ long-term wellbeing, cognitive functioning, and even life expectancy.
Untreated depression, and particularly untreated recurrent depression, carries high risks not only for lethality by suicide, but also for increases in medical mortality, particularly from cardiovascular disease. In addition to these medical risks, data from many studies suggest that a higher number of prior depressions is associated with increased cognitive dysfunction, and recent large data sets from a case registry in Denmark indicate that patients with four or more prior unipolar or bipolar depressive episodes have double the risk of receiving a diagnosis of dementia in old age. Thus, depressions are dangerous for a patient’s psychological, medical, and cognitive health.
Antidepressants Are Highly Effective in Depression Prevention
In 1992 researcher John Davis completed a meta-analysis of all antidepressant data available at the time in unipolar depression studies and not only found that antidepressant continuation was more effective than placebo in reducing the likelihood of later depressions, but also calculated that the statistical likelihood that this finding was due to chance was minuscule, i.e., p<10-34. John Geddes and colleagues in a meta-analysis in 2003 indicated that there was an approximate 70% reduction in the risk of depressive recurrences with antidepressant continuation compared with discontinuation.
Treatment of a first or second episode of unipolar depression is recommended for six to nine months following achievement of remission. After a third episode, all treatment guidelines of which this editor is aware recommend long-term preventive treatment with antidepressants, particularly if episodes have been severe or close together temporally. This long-term antidepressant continuation for prophylaxis is much like long-term treatment of high blood pressure or high cholesterol recommended for those with or at high risk for cardiovascular disease.
There is some evidence that cognitive behavior therapy reduces the risk for depressive recurrence in those discontinuing antidepressant treatment, but it appears maximally beneficial to engage both psychotherapeutic and pharmacological treatment to prevent future episodes. Read more
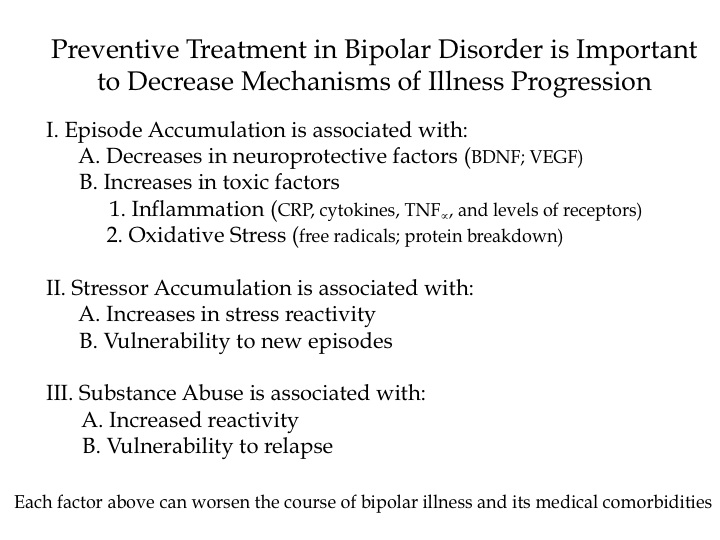
Why Preventive Treatment Is Important
RTMS Versus ECT
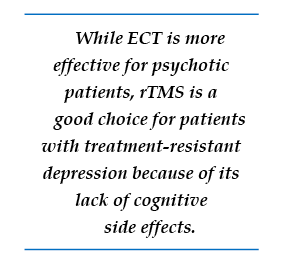 We’ve been posting about repeated transcranial magnetic stimulation (rTMS), a treatment in which a magnetic field is applied to a patient’s head, where it is able to affect tissue 2-3 centimeters into the brain.
We’ve been posting about repeated transcranial magnetic stimulation (rTMS), a treatment in which a magnetic field is applied to a patient’s head, where it is able to affect tissue 2-3 centimeters into the brain.
In randomized, controlled, head to head comparisons of electroconvulsive therapy (ECT) and repeated transcranial magnetic stimulation (rTMS), ECT often proves superior, particularly for a more severe psychotic or medically compromised patient. Nonetheless, for a more routine patient with non-psychotic depression, multiple studies have shown approximate equivalence of rTMS and ECT, while rTMS may have a superior benefit-to-risk ratio because it brings less risk of cognitive dysfunction. Thus, given almost equivalent efficacy for some subgroups of depressed patients, and a clear advantage for rTMS in terms of lack of cognitive side effects, this editor/clinician would recommend a course of rTMS prior to a series of ECT for the subgroup of non-emergency treatment-resistant depressed patients.
However, for highly treatment-refractory, severe, and particularly psychotic depression, few treatments appear to approach the efficacy and rapid response onset of electroconvulsive therapy (ECT). ECT as given in the modern era involves anesthesia and muscle paralysis while the patient is mechanically ventilated in order to prevent any damage from muscle contractions during the seizure. Read more
Long-Term Treatment with Lithium, Valproate, or Carbamazepine: Lithium Best for Most Patients
 Shannon Stepan, Eric Peselow and Nunzio Pomara from Maimonides Medical Center in Brooklyn, NY, have analyzed naturalistic observations of long-term maintenance treatment of bipolar disorder with valproic acid, lithium, and carbamazepine and found that patients on lithium went much longer before experiencing an episode of mania or depression than patients taking carbamazepine or valproate.
Shannon Stepan, Eric Peselow and Nunzio Pomara from Maimonides Medical Center in Brooklyn, NY, have analyzed naturalistic observations of long-term maintenance treatment of bipolar disorder with valproic acid, lithium, and carbamazepine and found that patients on lithium went much longer before experiencing an episode of mania or depression than patients taking carbamazepine or valproate.
The team followed 225 outpatients for up to 124 months, or until they had a manic or depressive episode or dropped out of the study during a well phase. Ninety-eight patients took lithium, 78 took valproate, and 50 took carbamazepine. Fifty-two percent of the participants dropped out of the study during a well phase.
One hundred three patients (45.8%) had either a manic or depressive episode during the study. This included 36.7% of the patients taking lithium, 55% of patients taking valproate, and 50% of patients taking carbamazepine. Median time until a first episode was 45 months for the entire sample, 36 months for those patients on valproate, 42 months for those on carbamazepine, and 81 months for those on lithium. A statistical analysis known as a Cox regression model indicated that patients taking valproate had a significantly higher risk of having a manic or depressive episode than those taking lithium.
Editor’s note: These naturalistic data are highly consistent with a number of more controlled clinical studies. In particular, the BALANCE study by Geddes et al. (2010) reported that lithium was superior to valproate on most outcome measures in a two-year randomized study, and that the combination of lithium and valproate was significantly better than valproate alone. Read more
Inflammation and Oxidative Stress in Bipolar Disorder
A number of studies presented at the 4th Biennial Conference of the International Society for Bipolar Disorders conference in Sao Paulo, Brazil in March reported new data relevant to inflammation and oxidative stress. Both inflammation and oxidative stress increase risk of cardiovascular disorders, and patients with inadequately treated mood disorders lose 10 or more years of life expectancy from cardiovascular disorders compared to the general population. Inflammation and oxidative stress may also contribute to the symptoms, evolution, and progression of the mood disorders themselves.
It is possible that these two processes could become new targets for therapeutic intervention in addition to more traditional psychopharmacological drugs that primarily target the neurotransmitters dopamine, norepinephrine, serotonin, and the neurotrophic factor BDNF. Read more