Hyperinsulinemia Associated Depression
Haider Sarwar writes in Clinical Medicine Insights (2022) that “Hyperinsulinemia promotes fat accumulation, causing obesity. Being an inflammatory state, obesity can induce further inflammation and is a risk factor for HPA (hypothalamic pituitary axis) dysregulation through hypercortisolism-related hyperglycemia….A disruption on SNS (sympathetic nervous system) activity increases insulin levels, and induces glycogenolysis in the liver and lipolysis in adipose tissue during hypoglycemia. Hyperglycemia-hyperinsulinemia exacerbates inflammation and increases the oxidative stress along with regulating the levels of norepinephrine in the brain sympathetic system. Increased inflammatory cytokines have also been shown to disrupt neurotransmitter metabolism and synaptic plasticity which play a role in the development of depression via inhibiting serotonin, dopamine, melatonin, and glutamate signaling. An increased level of plasma insulin over time in the absence of exercising causes …an increase in insulin resistance due to obesity and further culminates into depression….. Triple therapy with SSRI, bupropion, and cognitive behavioral therapy aids in improving glycemic control, lowering fasting blood glucose, decreasing the chances of relapse, as well as decreasing cortisol levels to improve cognition and the underlying depression.”
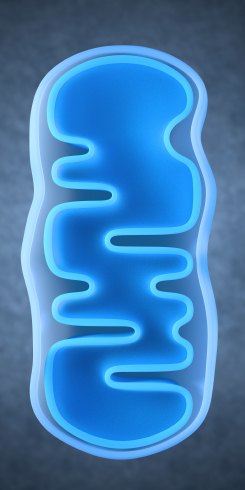
Lithium Reverses Effects of Oxidative Stress on Mitochondrial Function
Oxidative stress has been implicated in a wide range of illnesses, but what is it exactly? Our bodies use the oxygen we breathe to burn the fuel we get from food, and while this is a natural process, it produces byproducts known as free radicals, which are unstable molecules that can strip electrons from other molecules in a process called oxidation. Antioxidants (such as vitamin C) act as a source of electrons, helping keep other cells stable and healthy. Oxidative stress refers to the stress on our bodies from the normal effects of free radicals combined with environmental stressors like tobacco smoke or radiation.
In work presented at the 2013 meeting of the Society of Biological Psychiatry, Anna Andreason showed that over-activity of neurons increases oxidative stress through the production of reactive oxygen species (ROS). These are a type of free radicals that can damage cells in two ways: nitrosylation of proteins (adding nitric oxide to a thiol molecule), and oxidation, which results in more lasting effects on synaptic structures. The chemical compound rotenone damages mitochondria by producing ROS, and Andreason found that lithium was able to reverse this production and reverse the adverse effects of oxidative stress.
Lithium Has an Amazing Array of Positive Effects
Editor’s Note: The ability of lithium to protect mitochondria (the energy storehouse of a cell) adds to an increasingly long list of lithium’s neurotropic and neuroprotective benefits. Lithium increases cell survival factors BDNF and Bcl-2, increases markers of neuronal integrity such as N-Acetylaspartic acid (NAA), increases the volume of the hippocampus and cortex, and now helps protect mitochondria from oxidative stress. Lithium also increases the length of telomeres, which cap the ends of chromosome and protect them from damage during the DNA replication that occurs each time a cell divides. Short telomeres are associated with many kinds of medical and psychiatric diseases, as well as shorter life spans. No wonder that in addition to preventing mania and depression it has other clinical benefits, such as preventing memory deterioration, medical mortality, and suicide.
How Illness Progresses In The Recurrent Affective Disorders
This editor (RM Post) in collaboration with Jacqueline Fleming and Flavio Kapczinski published the article “Neurobiological mechanisms of illness progression in the recurrent affective disorders” in the Journal of Psychiatric Research this year. The article built on several themes about the progression of bipolar illness that had been explored in previous research.
These themes include:
- The likely acceleration of repeated episodes as a function of the number of prior episodes (episode sensitization)
- The increased responsivity of the illness to repeated stressors (stress sensitization)
- The increased behavioral reactivity to repeated use of psychomotor stimulants such as cocaine (stimulant-induced behavioral sensitization)
Not only are these observations well documented in the scientific literature, but recent observations also suggest that each type of sensitization can show cross-sensitization to the other two types. That is, individuals exposed to repeated stressors are more likely both to experience affective illness episodes and to adopt comorbid substance abuse. In a similar way, episodes of an affective disorder and stressors may also be associated with the relapse into drug administration in those who have been abstinent.
In addition to these mechanisms of illness progression in the recurrent affective disorders, the new article reviews the literature showing that the number of affective episodes or the duration of the illness appear to be associated with a variety of other clinical and neurobiological variables.
The number of affective episodes a patient experiences is associated with the degree of cognitive dysfunction present in their bipolar illness, and experiencing more than 4 episodes of unipolar or bipolar depression is a risk factor for dementia in late life. A relative lack of response to most treatments is also correlated with the number of prior episodes, and this holds true for response to naturalistic treatment in general. While most of these data are correlational and the direction of causality cannot be ascertained for certain, it is likely that the number of affective episodes and/or their duration could account for and drive difficulties with treatment and with cognitive function.
If this were the case, one would expect to see a variety of neurobiological correlates with the number of prior episodes or duration of illness, and in the article we summarize those that have been found in unipolar and bipolar disorder. Considerable data indicate that cortical volume and degrees of prefrontal cortical dysfunction can vary as a function of number of prior episodes. There is evidence that increased activity of the amygdala and the nucleus accumbens are also related to episodes or duration of illness. In those with unipolar depression, the volume of the hippocampus is decreased with longer duration of illness. Read more
Inflammation and Oxidative Stress in Bipolar Disorder
A number of studies presented at the 4th Biennial Conference of the International Society for Bipolar Disorders conference in Sao Paulo, Brazil in March reported new data relevant to inflammation and oxidative stress. Both inflammation and oxidative stress increase risk of cardiovascular disorders, and patients with inadequately treated mood disorders lose 10 or more years of life expectancy from cardiovascular disorders compared to the general population. Inflammation and oxidative stress may also contribute to the symptoms, evolution, and progression of the mood disorders themselves.
It is possible that these two processes could become new targets for therapeutic intervention in addition to more traditional psychopharmacological drugs that primarily target the neurotransmitters dopamine, norepinephrine, serotonin, and the neurotrophic factor BDNF. Read more