Early Precursors of Mood Disorders in Young Children of Parents with Bipolar or Unipolar Disorder

At the 2020 meeting of the International Society for Bipolar Disorders, researcher Caroline Vandeleur presented findings from a 13-year study of children in Switzerland who have a parent with bipolar disorder or major depressive disorder. In contrast to findings from the US presented by Danella Hafeman, Vandeleur and colleagues found no evidence of psychopathology in 4 year-olds. They did find that in 7-year-olds, children of a parent with major depressive disorder were four times more likely to have a separation anxiety disorder. In an overall sample of 449 children with a mean age of 10 who were followed up for 13 years, major depression tended to be preceded by anxiety disorders. Participants who went on to be diagnosed with bipolar disorder had earlier symptoms of depression, subthreshold hypomania, conduct disorders, and drug abuse. These were especially common in those who had a parent with bipolar disorder.
Editor’s Note: These data indirectly confirm other observations in which children at high risk for mood disorders in the US showed earlier signs of psychopathology than those in other countries including the Netherlands and Canada.
Meta-Analysis Finds Antidepressants More Effective Than Placebo
In a 2018 article in the journal The Lancet, researchers led by Andrea Cipriani compared the efficacy of 21 different antidepressants and established that antidepressants are more effective than placebo at reducing unipolar depression. To date, this is the largest meta-analysis of double-blind, randomized controlled studies of antidepressant efficacy, including 522 trials and a total of 116,477 participants. All 21 of the antidepressants were found to be more effective than placebo.
Looking at head to head studies, Cipriani and colleagues found that the most effective antidepressants were agomelatine, amitriptyline, escitalopram, mirtazapine, paroxetine, venlafaxine, and vortioxetine. The least effective antidepressants were fluoxetine, fluvoxamine, reboxetine, and trazodone.
In terms of tolerability, agomelatine, citalopram, escitalopram, fluoxetine, sertraline, and vortioxetine were most tolerable to patients, while amitriptyline, clomipramine, duloxetine, fluvoxamine, reboxetine, trazodone, and venlafaxine caused the most study dropouts due to side effects. Only agomelatine and fluoxetine had better dropout rates than placebo.
Interestingly, agomelatine, the medication found to be most effective and most tolerable, is unavailable in the US. Pharmaceutical company Novartis, which owns the rights to the drug, was disappointed by some lackluster studies of the drug and never applied for Food and Drug Administration approval to sell it in the US. The studies found potential problems regarding drug interactions related to the metabolic enzyme CYP1A2 and a risk of liver damage with longer-term use.
Editor’s Note: This meta-analysis should end any remaining controversy about the efficacy of antidepressants in the acute treatment of unipolar depression.
This study did not address maintenance treatment for the prevention of depressive episodes. Researcher John R. Geddes and colleagues have found robust, statistically significant data that continuation treatment with antidepressants can prevent depressive relapse, suggesting that if patients continue taking effective antidepressants, rather than switching to placebo, the antidepressants can reduce depressive occurrences by about 70%.
It is now recommended in most guidelines that patients with two or three prior episodes of depression consider staying on antidepressants indefinitely over their lifetime in order to prevent recurrence. Antidepressants increase the creation of new neurons and brain-derived neurotrophic factor (BDNF), which protects neurons and is important for learning and memory. Antidepressants can also prevent loss of hippocampal volume.
Longer Periods of Untreated Depression Linked to More Brain Inflammation
 A 2018 study by researchers Elaine Setiawan, Sophia Attwells and colleagues reports that inflammation seems to increase with duration of untreated unipolar depression. This implies that depression may be a progressive illness, and later stage depression may require different treatments than early stage depression, such as those that directly target inflammation.
A 2018 study by researchers Elaine Setiawan, Sophia Attwells and colleagues reports that inflammation seems to increase with duration of untreated unipolar depression. This implies that depression may be a progressive illness, and later stage depression may require different treatments than early stage depression, such as those that directly target inflammation.
The study published in the journal The Lancet Psychiatry used positron emission tomography (PET scan) to examines levels of translocator protein in the brain. Higher levels of translocator protein indicate activation of microglia, the brain’s immune cells, which can respond to trauma or injury.
The study included 80 participants between the ages of 18 and 75. Ten had a history of more than 10 years of depression, ten had experienced fewer than 10 years of depression, and 30 comprised a healthy comparison group.
The best predictors of high levels of translocator protein were duration of untreated major depressive disorder, total illness duration, and duration of antidepressant exposure. These three factors explained about half of the variation in translocator protein levels. Those participants whose depression went untreated for 10 years or longer had inflammation levels 29–33% higher than those whose depression was untreated for 9 years or less.
Participants who had received antidepressant treatment appeared to avoid an average yearly increase in the extent of their microglial activation.
The study took place at Canada’s Centre for Addiction and Mental Health.
Editor’s Note: Since inflammation is a predictor of poorer response to antidepressants, these data add a further neurochemical rationale to the already strong clinical rationale for earlier and more sustained antidepressant treatment and prevention. Virtually all treatment guidelines suggest that after two or three prior unipolar depressions, patients should receive long-term (lifelong) antidepressant treatment.
There is now a large body of data, including a 2012 article by this editor Robert M. Post and colleagues in the Journal of Psychiatric Research that too many episodes can hurt the brain, and the current study adds to this perspective. Avoiding preventive treatment for too long may actually foster the development of more episodes and more treatment resistance. A good mantra is “prevent episodes, protect the brain.”
Consensus is now also building that comprehensive long-term treatment is indicated after a first manic episode. A 2013 article by Lars Kessing and colleagues in the British Journal of Psychiatry suggested that high quality initial treatment can improve the long-term course of illness. Moreover, a 2016 article by Jan-Marie Kozicky and colleagues and a 2017 article by Christine Demmo and colleagues, both in the journal Bipolar Disorders, suggest that after a first mania, cognition recovers over the next year only if no further episodes occur in that time.
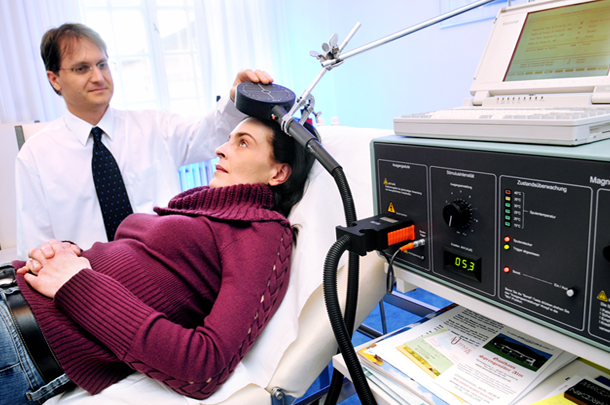
Three-Minute ‘Theta Burst’ Treatment as Effective as 37-Minute RTMS
A variation on repeated transcranial magnetic stimulation (rTMS) called intermittent theta burst stimulation (iTBS) may be able to deliver the same benefits in a tenth of the time. RTMS is a non-invasive treatment in which a magnetic coil placed near the skull transmits electrical signals to the brain. It is effective in depression and has been shown to improve aspects of schizophrenia, autism, and addictions as well.
A typical rTMS session lasts for 37.5 minutes and consists of high frequency (10 Hz) stimulation. Access to the treatment remains somewhat limited, so the newer form of iTBS treatment may help more people access treatment by allowing clinicians to treat more patients in a day.
The 2018 study, published by Daniel Blumberger and colleagues in the journal The Lancet, compared iTBS to standard rTMS and evaluated the effectiveness, safety, and tolerability of the new treatment compared to the old. 414 patients aged 18–65 with major depression that had persisted despite treatment with several antidepressant options were randomized to receive either iTBS or rTMS delivered to their left dorsolateral prefrontal cortex. They received the given treatment five days/week for four to six weeks.
Patients who received iTBS showed a nearly identical level of improvement in depression to those who received rTMS. Self-reports of pain intensity were worse among those who received iTBS, but the dropout rate was not higher for that group. Headaches were the most common side effect reported, and rates were similar across both groups. The authors judged iTBS to be a comparable, non-inferior alternative to rTMS for people with major depression.
Among participants who received iTBS, depression improved significantly, with 32 percent reporting a remission of depression symptoms. Those who received standard rTMS had a remission rate of 27 percent.
Using Antidepressants During Pregnancy Likely Does Not Increase Autism Risk
In the past year or so, several meta-analyses have analyzed data from numerous studies of a possible link between antidepressant use in pregnancy and autism in the offspring. In a 2017 article in the Journal of Clinical Psychiatry, researcher Chittaranjan Andrade offers a meta-analysis of these previous meta-analyses, and determines that while there is a small link between antidepressant use in pregnancy and autism in the offspring, it is most likely the mother’s depressive illness rather than the medications that is responsible for this link.
Andrade found that antidepressant exposure was linked to an increased risk of autism spectrum disorders in the offspring even when the antidepressant use occurred only before conception occurred, when it could not possibly have affected the future fetus’ physiology. This implies that it is the mother’s illness rather than the antidepressant treatment that is a determinant of autism risk.
Depression and Suicidal Thoughts Linked to Brain Inflammation
A 2017 article by Sophie E. Holmes and colleagues in the journal Biological Psychiatry reports that people with major unipolar depression, especially those with suicidal thoughts, have higher levels of the inflammatory marker translocator protein than do healthy individuals.
The participants with depression and suicidal thinking had high levels of translocator protein in the anterior cingulate cortex, which suggests that inflammation is affecting microglia.
Many studies have found links between different indicators of inflammation and mood disorders, leading researchers to speculate whether targeting the immune system could be an effective way to treat mood disorders. Patients with high levels of inflammation often fail to respond to typical treatments for depression.
Some previous research has found evidence of microglial activation in the brains of people who died from suicide.
The small study by Holmes and colleagues used positron-emission tomography, or PET scans, to observe evidence of translocator protein levels in the brain in 14 medication-free participants in a major depressive episode and 13 healthy volunteers. Those with depression, and particularly those with suicidal thoughts, showed more evidence of neuroinflammation.
Combo of Memantine and Sertraline Effective for Unipolar Depression
A 2016 study in the Journal of Clinical Pharmacy and Therapeutics finds that the combination of memantine (Namenda), a drug used to treat Alzheimer’s disease, and the antidepressant sertraline (Zoloft) improved unipolar depression more than sertraline plus placebo.
The study by Meysam Amidfar and colleagues included 66 patients with moderate to severe unipolar depression. They were divided into two groups—one received sertraline plus memantine for six weeks, while the other received sertraline and a placebo.
The memantine group showed significantly greater improvement at 2 weeks, 4 weeks, and 6 weeks, and significantly greater response at 4 and 6 weeks. There were also more early improvers in the mematine group, and more rapid response to treatment. Both groups improved significantly over the six weeks of treatment.
Larger studies are needed to learn more about the safety and efficacy of memantine combined with sertraline for the treatment of unipolar depression, but this initial study is promising. In 2012, researcher Amit Anand and colleagues reported that in bipolar depression, memantine potentiates the effects of lamotrigine. Memantine also helped rapid cyclers when added to ongoing treatment in an open study of the drug treatment by Athanasios Koukopoulus and colleagues in 2012.
Meta-Analysis Shows Effectiveness of Ketamine for Bipolar and Unipolar Depression
Ketamine, an anesthetic sometimes used intravenously in the treatment of depression, can bring about rapid onset of antidepressant effects. A new meta-analysis by researcher Michael Bloch and colleagues presented at a recent conference showed that ketamine’s maximum antidepressant effects occur within one day of administration, and its effects remain significant (compared to control conditions) one week following infusion. Ketamine’s effects were diminished in patients taking other medications. There was a trend for better response in patients with bipolar disorder than with unipolar disorder.
Bloch and colleagues analyzed eight earlier studies including a total of 180 participants. In each study, ketamine had been compared to a control condition, either an infusion of saline solution or of midazolam, which mimics ketamine’s sensory effects but does not have antidepressant effects. The researchers are calling for more meta-analyses of ketamine studies to determine which patients respond best to ketamine and how to sustain ketamine’s effects.
Editor’s Note: In another poster presented at the same conference, James Murrough reported that patients with slower processing speed responded best to ketamine. Other findings have shown that those with a history of alcohol abuse and a common genetic variant of brain-derived neurotrophic factor (BDNF), the val-66-val allele of proBDNF, are more likely to respond to ketamine.
Ziprasidone Added to Escitalopram Improved Unipolar Depression
In a new study of patients with major depressive disorder who did not improve after eight weeks of the selective serotonin reuptake inhibitor (SSRI) antidepressant escitalopram, the addition of the atypical antipsychotic ziprasidone improved their depression more than did placebo. Patients took the combination of escitalopram (20mg/day on average) and ziprasidone twice a day at doses of 20–80 mg.
This was the first randomized, double-blind placebo controlled trial of ziprasidone as an adjunct treatment for unipolar depression. While ziprasidone was more efficacious than placebo, discontinuation of the study due to intolerance was higher among the patients who received ziprasidone.
Editor’s Note: Two atypical antipsychotics (quetiapine and aripiprazole) have been approved by the Federal Drug Administration for augmentation of antidepressants in unipolar depression. Now there have also been placebo-controlled positive trials of two others (ziprasidone and cariprazine).
These findings are of particular interest as the studies of ziprasidone monotherapy in bipolar depression not only failed, but response to ziprasidone and placebo was virtually identical (and negligible).
Brain Activity Differentiates Youth with Bipolar Disorder from Youth with Unipolar Depression
Both bipolar disorder and unipolar depression often begin in childhood or adolescence, but it can be difficult to distinguish the two using symptoms only. People with bipolar illness may go a decade without receiving a correct diagnosis. Researcher Jorge Almeida and colleagues recently performed a meta-analysis of previous studies to determine what neural activity is typical of children with bipolar disorder versus children with unipolar depression while processing images of facial emotion. They found that youth with bipolar disorder were more likely to show limbic hyperactivity and cortical hypoactivity during emotional face processing than youth with unipolar depression. Almeida and colleagues hope that this type of data may eventually be used to diagnose these disorders or to measure whether treatment has been successful.