Early Precursors of Mood Disorders in Young Children of Parents with Bipolar or Unipolar Disorder

At the 2020 meeting of the International Society for Bipolar Disorders, researcher Caroline Vandeleur presented findings from a 13-year study of children in Switzerland who have a parent with bipolar disorder or major depressive disorder. In contrast to findings from the US presented by Danella Hafeman, Vandeleur and colleagues found no evidence of psychopathology in 4 year-olds. They did find that in 7-year-olds, children of a parent with major depressive disorder were four times more likely to have a separation anxiety disorder. In an overall sample of 449 children with a mean age of 10 who were followed up for 13 years, major depression tended to be preceded by anxiety disorders. Participants who went on to be diagnosed with bipolar disorder had earlier symptoms of depression, subthreshold hypomania, conduct disorders, and drug abuse. These were especially common in those who had a parent with bipolar disorder.
Editor’s Note: These data indirectly confirm other observations in which children at high risk for mood disorders in the US showed earlier signs of psychopathology than those in other countries including the Netherlands and Canada.
Parents’ History of Mood and Anxiety Disorders Increases Risk of These Disorders in Offspring
A 2016 article by researcher Petra J. Havinga and colleagues in the Journal of Clinical Psychiatry suggests that offspring of a parent with a mood or anxiety disorder are at higher risk for these disorders than offspring from non-ill parents. Havinga and colleagues studied 523 offspring of parents with one of these disorders. Among these offspring, 38.0% had had a mood or anxiety disorder by age 20, and 64.7% had had such a disorder by age 35. (Rates of these disorders in the general population are closer to 10%.)
The risk of offspring developing one of these disorders was even higher when both parents had a history of a mood or anxiety disorder, when a parent had an early onset of one of these illnesses, and when the offspring was female. The good news is that balanced family functioning had a protective effect, reducing the likelihood that the offspring would develop a mood or anxiety disorder.
Researcher David Axelson reported in a 2015 study published in the American Journal of Psychiatry that approximately 74% of the offspring of a parent with bipolar disorder went on to have a major psychiatric diagnosis over 6.7 years of followup. Similarly, researcher Myrna Weissman and colleagues reported in 2006 that the same high incidence of psychiatric diagnoses was true of the offspring of a parent with unipolar depression over 20 years of followup.
Editor’s Note: It is important to be vigilant for mood or behavioral disorders that may emerge in the offspring of a parent with a mood or anxiety disorder. Children at high risk should maintain a healthy diet and good sleep hygiene, exercise regularly, and perhaps try practicing mindfulness and meditation, as recommended by researcher Jim Hudziak. Family-focused therapy (developed by researcher David Miklowitz) can help when early symptoms appear in the offspring of a parent with bipolar disorder.
Another option is joining our Child Network, a secure online program that allows parents to track their children’s symptoms of anxiety, depression, attention-deficit hyperactivity disorder (ADHD), oppositional behavior, and mania. This may facilitate earlier recognition and treatment of dysfunctional symptoms, which can be treated with psychotherapy and medication.
In Rats, Mother’s Exercise Habits Affect Those of Offspring
 A recent study suggests that when a mother rat exercises during pregnancy, her offspring will exercise more too.
A recent study suggests that when a mother rat exercises during pregnancy, her offspring will exercise more too.
In the study, published by Jesse D. Eclarinel and colleagues in The FASEB Journal, pregnant mother rats were placed in cages that each contained an exercise wheel. One group had access to a working wheel on which they could run. The other group had the same wheel, but it was locked so that they couldn’t use it for running. Daughters of the rats who ran during pregnancy ran more in adulthood (both at 60 days and 300 days after birth) than daughters of the rats who couldn’t run during pregnancy.
While it is a mystery why this occurs, it is consistent with other data about the ways that a parent’s experiences can influence the next generation, even when the offspring don’t grow up with the parents.
For example, father rats conditioned to associate a specific smell with fear of an electric shock have offspring that also fear that smell (but not other smells).
Drug use is another example. Father rats given access to cocaine have offspring that are less interested in cocaine. Interestingly, father rats exposed to marijuana have offspring that are more interested in opiates.
Experiences with drugs or stress are thought to affect the next generation via ‘epigenetic’ marks on ova or sperm. These marks change the way DNA is packaged, with long-lasting effects on behavior and chemistry. Most marks from a mother’s or father’s experiences are erased at the time of conception, but some persist and affect the next generation.
The nature versus nurture debate is getting more and more complicated. Parents can influence offspring in a number of ways: 1) genetics; 2) epigenetics in the absence of contact between parent and offspring after birth; 3) epigenetic effects of behavioral contact—that is, parents’ caring and warmth versus abuse and neglect can affect offspring’s DNA expression too. All these are in addition to any purely behavioral influence a parent may have on their offspring via discipline, teaching, being a role model, etc.
Editor’s Note: The moral of the story is, choose your parents wisely, or behave wisely if you yourself become a parent.
Father’s Age, Behavior Linked to Birth Defects
For decades, researchers have known that a pregnant mother’s diet, hormone levels, and psychological state can affect her offspring’s development, altering organ structure, cellular response, and gene expression. It is now becoming clear that a father’s age and lifestyle at the time of conception can also shape health outcomes for his offspring.
Older fathers have offspring with more psychiatric disorders, possibly because of increased incidence of mutations in sperm.
A 2016 article by Joanna Kitlinska and colleagues in the American Journal of Stem Cells reviewed findings from human and animal studies about the links between fathers’ behaviors and their offspring’s development.
Father’s behavior can shape gene expression through a phenomenon described as epigenetics. Epigenetics refers to environmental influences on the way genes are transcribed. While a father’s behavior is not registered in his DNA sequences, it can influence the structure of his DNA or the way in which it is packaged.
Kitlinska suggests that these types of findings should eventually be organized into recommendations for prospective parents. More research is also needed into how maternal and paternal influences interact with each other.
Some findings from the article:
- A newborn can have fetal alcohol spectrum disorder even if the mother doesn’t drink. “Up to 75% of children with [the disorder] have biological fathers who are alcoholics,” says Kitlinska.
- Father’s alcohol use is linked to low birth weight, reduced brain size, and impaired cognition.
- Dad’s obesity is linked to enlarged fat cells, diabetes, obesity, and brain cancer in offspring.
- A limited diet in a father’s early life may reduce his children and grandchildren’s risk of death from cardiovascular causes.
- Dad’s advanced age is correlated with higher rates of schizophrenia, autism, and birth defects in his children.
- Psychosocial stress on dads can affect their children’s behavioral traits.
Anxiety, Depression, Unstable Mood, and Low-Level Mania Best Predictors of Bipolar Disorder
Researchers are looking for better ways of predicting whether children at risk for bipolar disorder will go on to develop the illness. A 2015 study by David Axelson and colleagues in the American Journal of Psychiatry reported that in the offspring of parents with bipolar disorder, diagnoses of sub-threshold mania, depression, and disruptive behavior disorders were associated with subsequent diagnosis of full-blown Bipolar I or Bipolar II disorders six to seven years later.
More recently, in an article by Danella M. Hafeman and colleagues in the American Journal of Psychiatry, the same group of investigators has examined how symptoms (rather than categorical diagnoses, as in the earlier study) predict the development of bipolar disorder. In children and adolescents at high risk for bipolar disorder (because they have a parent with the disorder) three types of symptoms were the best predictors of later bipolar disorder: anxiety/depression at the time participants entered the study, unstable mood or irritability both when entering the study and shortly before a bipolar diagnosis, and low-level manic symptoms observed shortly before diagnosis.
The earlier the age at which a parent was diagnosed with a mood disorder, the greater the risk that the offspring would also be diagnosed with bipolar disorder. Youth with all four risk factors (anxiety or depression, mood changes, low-level mania, and a parent who was diagnosed with a mood disorder at an early age) had a 49 percent chance of developing bipolar disorder, compared to a 2 percent chance among those without those risk factors.
Childhood onset of bipolar disorder and long delays until first treatment for depression or mania are both significant predictors of a poor outcome in adulthood compared to adult onsets and shorter delays to treatment. Read more
Stimulants Linked to Psychotic Symptoms in Offspring of Parents with Psychiatric Illness
Stimulants are one of the most common medications prescribed to children and adolescents, typically for attention deficit hyperactivity disorder (ADHD). In children of parents with major depression, bipolar disorder, or schizophrenia, stimulant use may come with a risk of psychotic symptoms. A 2016 study by L.E. MacKenzie and colleagues in the journal Pediatrics reported that among children and youth whose parents had one of these psychiatric illnesses, 62.5% of those who had taken stimulants had current psychotic symptoms, compared to only 27.4% of those who had not taken stimulants. The participants with psychotic symptoms tended to have hallucinations that occurred while they were taking stimulants. Doctors may want to consider whether parents have a history of psychiatric illness when deciding whether to prescribe stimulants to children and adolescents with ADHD. Activation is a common side effect of antidepressants in children who have a parent with bipolar disorder. Young people taking stimulants for ADHD should be monitored for psychotic symptoms, particularly if they have a parent with a history of depression, bipolar disorder, or schizophrenia.
Offspring of Bipolar Parents at High Risk for Psychiatric Disorders
Researcher Juan David Palacio reported at the 2015 meeting of the American Academy of Child and Adolescent Psychiatry that compared to offspring of non-ill parents, children of parents with bipolar I disorder are at high risk for psychiatric disorders, particularly bipolar spectrum disorders and substance use disorders. They were also at risk for symptoms of anxiety disorders and conduct disorder. Palacio’s findings from Colombia mirror those from other studies of familial risk and suggest the importance of vigilance to detect these disorders early and provide appropriate treatment. Our Child Network may help.
Diagnosing Childhood Bipolar Disorder: Mom Knows Best
In a talk at the 2015 meeting of the International Society for Bipolar Disorders, researcher Eric Youngstrom showed that mothers’ evaluation of their children’s psychiatric symptoms was more valid than both teacher ratings and the children’s own evaluations. Parents were better at detecting irritability, while children were better at assessing their energy levels and the quality of their sleep.
Youngstrom reported that about 2% of children worldwide are diagnosed with bipolar disorder. However, when bipolar disorder not otherwise specified (BP NOS), a diagnosis given when symptoms do not meet the diagnostic criteria for Bipolar I or II, is included in the statistics, rates of bipolar disorder among children in the US reach about 6%.
Youngstrom mentioned that an epidemiological study by Kathleen Merikangas found that among children in the US with a bipolar spectrum diagnosis, only 22% were in treatment, compared to 38% of those with depression and 60% of those with ADHD.
Parents of children (aged 2–12) with mood, anxiety, and behavioral disorders are invited to join the Child Network, our program for tracking weekly symptoms which can then be printed out longitudinally to share with the child’s doctor.
Offspring of Parents with Psychiatric Disorders At Increased Risk for Disorders of Their Own
At a symposium at the 2015 meeting of the International Society for Bipolar Disorder, researcher Rudolph Uher discussed FORBOW, his study of families at high risk for mood disorders. Offspring of parents with bipolar disorder and severe depression are at higher risk for a variety of illnesses than offspring of healthy parents.
Uher’s data came from a 2014 meta-analysis by Daniel Rasic and colleagues (including Uher) that was published in the journal Schizophrenia Bulletin. The article described the risks of developing mental illnesses for 3,863 offspring of parents with schizophrenia, bipolar disorder, or major depression compared to offspring of parents without such disorders.
Previous literature had indicated that offspring of parents with severe mental illness had a 1-in-10 likelihood of developing a severe mental illness of their own by adulthood. Rasic and colleagues suggested that the risk may actually be higher—1-in-3 for the risk of developing a psychotic or major mood disorder, and 1-in-2 for the risk of developing any mental disorder. An adult child may end up being diagnosed with a different illness than his or her parents.
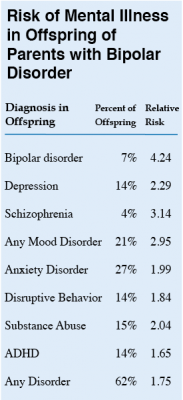 At the symposium, Uher focused on families in which a parent had bipolar disorder. These families made up 1,492 of the offspring in the Rasic study. The table at right shows the risk of an illness among the offspring of bipolar parents compared to that risk among offspring of healthy parents, otherwise known as relative risk. (For example, offspring of parents with bipolar disorder are 4.24 times more likely to be diagnosed with bipolar disorder themselves than are offspring of non-bipolar parents.) The table also shows the percentage of offspring of parents with bipolar disorder who have each type of disorder.
At the symposium, Uher focused on families in which a parent had bipolar disorder. These families made up 1,492 of the offspring in the Rasic study. The table at right shows the risk of an illness among the offspring of bipolar parents compared to that risk among offspring of healthy parents, otherwise known as relative risk. (For example, offspring of parents with bipolar disorder are 4.24 times more likely to be diagnosed with bipolar disorder themselves than are offspring of non-bipolar parents.) The table also shows the percentage of offspring of parents with bipolar disorder who have each type of disorder.
Editor’s Note: These data emphasize the importance of vigilance for problems in children who are at increased risk for mental disorders because they have a family history of mental disorders. One way for parents to better track mood and behavioral symptoms is to join our Child Network.
Predictors of Bipolar Disorder in At-Risk Youth
A new longitudinal study of 391 youth at risk for bipolar disorder revealed some predictors of the disorder. The study by Danella M. Hafeman and colleagues was presented at the 2015 meeting of the Society of Biological Psychiatry. The participants were aged 6–18 and each had a parent with bipolar disorder. Over the course of the study, 40 developed an illness on the bipolar spectrum, including 21 who developed bipolar I or II. The participants were assessed for various descriptive characteristics and those who developed bipolar disorder were compared to those who developed major depressive disorder.
The most important predictors of bipolar disorder were parental assessment of internalizing symptoms of anxiety or depression, self-assessment of mood changeability, and self-assessment of hostility. A diagnosis of bipolar disorder not otherwise specified (BP-NOS) was the only predictor of a later diagnosis of bipolar I or II.
Editors Note: These data resemble findings from a 2015 study by David Axelson and colleagues in the American Journal of Psychiatry that used the same cohort of participants. The Axelson study indicated that a categorical diagnosis of a major psychiatric disorder occurred in 74% of the offspring of a bipolar parent compared to about 50% in a control group from the community. Depression, anxiety, attention deficit hyperactivity disorder (ADHD), and oppositional disorders were even more common than bipolar disorder in the at-risk population.
The presence of a major psychiatric diagnosis in about three-quarters of the offspring of a parent with bipolar disorder suggests the importance of early vigilance. One way to track symptoms of depression, anxiety, ADHD, oppositional behavior, and bipolar disorder is to join the Child Network, a secure online platform for rating children’s moods, medications, and side effects. These weekly ratings can be collected longitudinally and printed out to help parents and clinicians assess mood difficulties in their children.









