Adolescent Delta-9-tetrahydrocannabinol induces long-term neuronal disturbances in dorsal vs. ventral hippocampus
De Felice et al reported in Neuropsychopharmacology (2022) how adolescent THC exposure in a rodent model can induce significant morphological disturbances and glutamatergic signaling abnormalities in the hippocampus. The dorsal hippocampus is critical for cognitive and contextual processing, whereas the ventral region is critical for affective and emotional processing. Adolescent THC exposure induces long-lasting memory deficits and anxiety like-behaviors concomitant with a wide range of differential molecular and neuronal abnormalities in dorsal vs. ventral hippocampal regions.
Editors Note: While these data are in rodents, they provide insights into how THC use in adolescents exerts memory deficits and anxiety-like behavior in adulthood by dysregulation of glutamate signaling in the hippocampus. These data converge with data in humans. The bottom line is: use of marijuana in adolescence is not good for brain function, cognition, and behavior in adulthood.
Successful Trial of N-Acetylcysteine for Veterans with PTSD and Substance Abuse
 The antioxidant N-acetylcysteine (NAC) can improve a number of habit-related conditions, such as substance use disorders, gambling, and compulsive hair-pulling. It also aids in the treatment of depression and obsessive-compulsive disorder (OCD). A 2016 study by Susie E. Back and colleagues in the Journal of Clinical Psychiatry found that NAC can also improve symptoms of post-traumatic stress disorder (PTSD) in veterans who also had substance use disorders.
The antioxidant N-acetylcysteine (NAC) can improve a number of habit-related conditions, such as substance use disorders, gambling, and compulsive hair-pulling. It also aids in the treatment of depression and obsessive-compulsive disorder (OCD). A 2016 study by Susie E. Back and colleagues in the Journal of Clinical Psychiatry found that NAC can also improve symptoms of post-traumatic stress disorder (PTSD) in veterans who also had substance use disorders.
In the pilot study of 35 veterans, participants were randomized to receive an 8-week course of NAC (2,400 mg/day) or placebo, plus cognitive-behavioral therapy targeting their substance use disorder. PTSD and substance use disorders have some overlapping neurobiological features, such as impaired prefrontal cortex regulation of basal ganglia circuitry.
At the end of the 8-week trial, those veterans who received NAC showed improvement in PTSD symptoms, substance cravings, and depression compared to those who received placebo. Substance use was similar and low among both groups. Side effects were minimal.
While these results were preliminary, they suggest that NAC could treat both PTSD and substance use disorders, which often occur together. Larger studies are expected to follow.
Editor’s Note: These preliminary data add to the evidence that NAC has remarkably wide utility in addictions (cocaine, alcohol, nicotine, and marijuana), habits (including OCD, trichotillomania/hair-pulling, nail biting, skin-picking, and cutting), depression and anxiety in bipolar disorder and negative symptoms in schizophrenia.
Offspring of Bipolar Parents at High Risk for Psychiatric Disorders
Researcher Juan David Palacio reported at the 2015 meeting of the American Academy of Child and Adolescent Psychiatry that compared to offspring of non-ill parents, children of parents with bipolar I disorder are at high risk for psychiatric disorders, particularly bipolar spectrum disorders and substance use disorders. They were also at risk for symptoms of anxiety disorders and conduct disorder. Palacio’s findings from Colombia mirror those from other studies of familial risk and suggest the importance of vigilance to detect these disorders early and provide appropriate treatment. Our Child Network may help.
Substance Abuse Is a Treatable Brain Disorder
Depression and bipolar disorder come with a high incidence of substance abuse. It is important to realize that there are now good medicines to treat the addictions as well as the primary mood disorders they accompany. At the 2015 meeting of the American Psychiatric Association, Nora Volkow, director of the National Institute of Drug Abuse, encouraged psychiatrists to think of addiction as a “disease of the brain that disrupts the systems that allow people to exert self-control,” saying that this would help reduce stigma both for insurance companies and for the wider public.
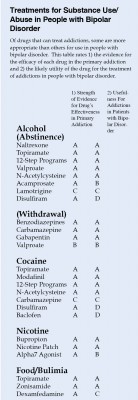
Most treatment of substance abuse in bipolar disorder is off-label. Doctors must infer indirect evidence of the possible efficacy of each drug in bipolar disorder from studies in those with only the primary addiction, for example, cocaine abuse without bipolar disorder.
The table at right is a preliminary rating of 1) the strength of the evidence for the efficacy of each drug in the primary addiction and 2) the likely utility of the drug for the treatment of addictions in people with bipolar disorder. For example, the drug baclofen has excellent evidence of efficacy in cocaine addiction, but gets a D for utility in bipolar disorder because baclofen can exacerbate depression.
This list is provisional, and the subjective grades for each drug are likely to change as more research is collected on these treatments. Consult a doctor if you are seeking treatment for bipolar disorder and/or substance abuse.
Connections Between Stress and Substance Use May Be Mediated By Corticotropin-Releasing Factor
 Researchers hope to map out the neurocircuitry by which stress leads to compulsive drug taking. A recent study by Klaus Miczek and colleagues examined different rodents’ responses to the stress of being repeatedly placed in the cage of a larger, more aggressive rodent, developing what is known as defeat stress, a set of behaviors that mimic human depression. Mice and rats showed increases in the stress hormone corticosterone that did not diminish over repeated run-ins with a larger animal. Rodents who were exposed to this stress became sensitized to cocaine or amphetamine, showing hyperactivity that increased each time they accessed the drug (the opposite of a tolerance response). Some also “binged” on cocaine, which they were able to self-administrate by pushing a lever to receive infusions. The mice and rats that went through the social defeat showed elevated levels of dopamine in the nucleus accumbens, the brain’s reward center. Levels were related to the severity of their stressful experience.
Researchers hope to map out the neurocircuitry by which stress leads to compulsive drug taking. A recent study by Klaus Miczek and colleagues examined different rodents’ responses to the stress of being repeatedly placed in the cage of a larger, more aggressive rodent, developing what is known as defeat stress, a set of behaviors that mimic human depression. Mice and rats showed increases in the stress hormone corticosterone that did not diminish over repeated run-ins with a larger animal. Rodents who were exposed to this stress became sensitized to cocaine or amphetamine, showing hyperactivity that increased each time they accessed the drug (the opposite of a tolerance response). Some also “binged” on cocaine, which they were able to self-administrate by pushing a lever to receive infusions. The mice and rats that went through the social defeat showed elevated levels of dopamine in the nucleus accumbens, the brain’s reward center. Levels were related to the severity of their stressful experience.
Later the rodents had a choice between water and a 20% alcohol solution. The researchers determined what type of stress led the rodents to consume the alcohol solution instead of the water. The maximal effect was seen in two types of mice that suffered an attack of less than five minutes that resulted in a moderate number of attack bites (30); this resulted in the mice consuming large amounts (15–30 g/kg/day) of the alcohol solution. Earlier sensitization to cocaine or amphetamine did not predict later alcohol or cocaine self-administration.
When the researchers injected the rodents with antagonists of the receptors for corticotropin-releasing factor, a hormone and neurotransmitter important in stress response, prior to each episode of social defeat, the rodents did not escalate their cocaine or alcohol self-administration, indicating that CRF plays an essential role in the process by which stress makes animals prone to using substances.
In related research by Camilla Karlsson and colleagues, IL-1R1 and TNF-1R, the receptors for two inflammatory cytokines, mediated the effects of social stress on escalated alcohol use in mice.