Positive Effects of a Brief Session of Aerobic Exercise for Sedentary Children
At a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Benjamin I. Goldstein reported that a single 20-minute session of aerobic exercise (achieving 70% of maximal heart rate) was associated with improvement in cognition and in abnormalities seen on brain imaging in young people. Goldstein urged clinicians to do motivational interviews with sedentary children in their care, emphasizing the positive cardiovascular and cognitive effects of exercise. He indicated this would be more effective than a focus only on weight loss, which is much more difficult to achieve.
Family Focused Therapy Effective in Youth at Risk for Bipolar Disorder Who Have Early Symptoms
 Researcher David Miklowitz developed Family Focused Therapy (FFT), in which families of young people at risk for bipolar disorder take part in therapy, learning about the illness and practicing strategies for communication and coping.
Researcher David Miklowitz developed Family Focused Therapy (FFT), in which families of young people at risk for bipolar disorder take part in therapy, learning about the illness and practicing strategies for communication and coping.
At a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, Miklowitz reported findings from recent studies of youth who were at high risk for bipolar disorder because of a family history of the illness and the presence of early symptoms such as depression or cyclothymia or bipolar not otherwise specified (BP-NOS). Family focused therapy reduced symptoms. It also slowed onset of a first episode of mania and slowed the conversion to a diagnosis of bipolar I or bipolar II. These results converge with a total of 10 other positive studies of family focused therapy in different populations in children and adults. FFT or its equivalent should be made available to all symptomatic children who are at risk for bipolar disorder because of a family history of the disorder.
Potential Problems when Youth at Risk for Bipolar Disorder Take SSRIs
 At a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Manpreet Singh reported that in youth at high risk for bipolar disorder, 53% had an adverse event while taking a selective serotonin reuptake inhibitor antidepressant (SSRI), and 26% had a new onset of suicidality while taking an SSRI. These adverse events were associated with reduced size and increased activation of the amygdala, the brain region responsible for emotion processing. Singh concluded that dysfunction in the prefrontal-limbic network may predict adverse events in children at risk for bipolar disorder when they are given SSRI antidepressants. She urged caution in the use of antidepressants in this population. Researcher Joseph Biederman echoed this caution later in the meeting.
At a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Manpreet Singh reported that in youth at high risk for bipolar disorder, 53% had an adverse event while taking a selective serotonin reuptake inhibitor antidepressant (SSRI), and 26% had a new onset of suicidality while taking an SSRI. These adverse events were associated with reduced size and increased activation of the amygdala, the brain region responsible for emotion processing. Singh concluded that dysfunction in the prefrontal-limbic network may predict adverse events in children at risk for bipolar disorder when they are given SSRI antidepressants. She urged caution in the use of antidepressants in this population. Researcher Joseph Biederman echoed this caution later in the meeting.
Quetiapine Reduced Childhood Mania, Especially in Those with Thicker Frontal Temporal Regions
 In a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Melissa P. Delbello reported that six weeks of treatment with either lithium or quetiapine was effective in childhood mania, but quetiapine had a higher response rate of 71% versus 46% for lithium. Delbello found two types of structural changes on functional magnetic resonance imaging (fMRI). Some children had thicker frontal temporal regions, while others had thinning in these areas. The first group of patients had a 100% response to quetiapine, but only 53% of the second group responded to quetiapine.
In a symposium at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry, researcher Melissa P. Delbello reported that six weeks of treatment with either lithium or quetiapine was effective in childhood mania, but quetiapine had a higher response rate of 71% versus 46% for lithium. Delbello found two types of structural changes on functional magnetic resonance imaging (fMRI). Some children had thicker frontal temporal regions, while others had thinning in these areas. The first group of patients had a 100% response to quetiapine, but only 53% of the second group responded to quetiapine.
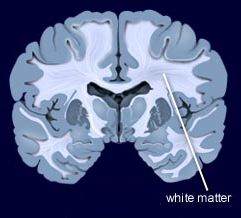
In contrast, other researchers have found lithium superior to quetiapine. Vivian Kafantaris showed that patients who respond well to lithium show improvements in white matter abnormalities. Michael Berk and colleagues found that a year on lithium was superior to quetiapine on all measures including cognition and brain imaging in patients having their first episode of mania.
7-Year-Olds At Risk for Schizophrenia, But Not Bipolar Disorder, Show Specific Types of Cognitive Dysfunction
 A large Danish study investigated whether children at risk for schizophrenia and bipolar disorder would show signs of cognitive problems. The study by researcher Nicoline Hemager and colleagues was published in the journal JAMA Psychiatry in 2018.
A large Danish study investigated whether children at risk for schizophrenia and bipolar disorder would show signs of cognitive problems. The study by researcher Nicoline Hemager and colleagues was published in the journal JAMA Psychiatry in 2018.
The researchers identified 7-year-olds,197 who had family members with schizophrenia, 118 who had family members with bipolar disorder, and 199 control 7-year-olds with no family history of these illnesses. Those children at risk for schizophrenia had significantly more cognitive deficits and behavioral disorders than the controls, while those children at risk for bipolar disorder did not differ significantly from the controls. The deficits among the children at risk for schizophrenia were in the areas of processing speed and working memory, executive and visuospatial functions, and declarative memory and attention.
The researchers indicated that the neurocognitive profile seen in the children at risk for schizophrenia could help clinicians identify these children for early intervention.
Lithium Effective for Maintenance Treatment of Childhood-Onset Bipolar Disorder
Evidence has been accumulating that lithium is effective in the treatment of young people with bipolar disorder. In a study by Robert Findling and colleagues published in the Journal of the American Academy of Child and Adolescent Psychiatry in 2018, participants aged 7–17 who responded well to lithium during a 24-week study were then randomized to receive either lithium continuation (17 participants) or placebo (14 participants) for 28 more weeks.
Those who continued lithium treatment were more likely to stay in the study. Participants who discontinued the study mostly reported that they did so due to re-emergence of their mood symptoms (mostly in the placebo group).
Lithium was well-tolerated and was not associated with any more weight gain than placebo. This study adds to the growing literature on the effectiveness and tolerability of lithium both acutely and in maintenance treatment in childhood bipolar disorder.
Lithium Better than Other Mood Stabilizers for Youth with Bipolar Disorder
A new study by Danella M. Hafeman and colleagues finds that lithium is superior to other mood stabilizers in young people. The data in this case come from 340 youth aged 7–17 who participated in a study known as Course and Outcome of Bipolar Youth (COBY).
At each visit over an average of 10 years, participants reported medications taken, symptoms they had experienced, etc. during the preceding six-month period. During times that participants had taken lithium (compared to other mood stabilizers) they were older, on fewer antidepressants, and they were less likely to have an anxiety disorder.
Those participants who took lithium had half as many suicide attempts, fewer depressive symptoms, less psychosocial impairment, and less aggression than those who took other mood stabilizers.
The researchers concluded, “Findings are consistent with adult studies, showing that lithium is associated with decreased suicidality, less depression, and better psychosocial functioning. Given the paucity of evidence regarding lithium in children and adolescents, these findings have important clinical implications for the pharmacological management of youth with bipolar disorder.”
Editor’s Note: Lithium should especially be considered in those with a family history of mood disorders, and in particular in those with a family history of good response to lithium. Lithium is under-prescribed in both adults and children and should be given much higher consideration in light of the multiple benefits it provides in addition to mood stabilization. These include maintenance of memory, increases in longevity (perhaps based in its ability to increase the length of telomeres, the bits of protective material at the end of DNA strands that deteriorate with age and illness), and neuroprotection against loss of gray and white matter volume in the brain, which often occurs in mood disorders.
Prazosin Effective and Well-Tolerated for PTSD in Young People
In a poster session at the 2019 meeting of the American Academy of Child and Adolescent Psychiatry (AACAP), three posters highlighted the efficacy and tolerability of prazosin, a drug typically used to treat high blood pressure, for the treatment of childhood-onset post-traumatic stress disorder (PTSD).
Researchers Samira Khan and Taniya Pradhan of West Virginia University reviewed cases in which 39 patients aged 8–19 received 1–5 mg of prazosin at bedtime. The mean dose was 1.72 mg. Sleep (including nightmares) improved in 92.3% of the youths, and mood improved in 33.3%. Sleep improved more in patients who received lower doses (1–2 mg) than those who received higher doses. About 70% of the patients whose data were included in the case series were also receiving psychotherapy while being treated with prazosin.
In another poster, researcher Vladimir Ferrafiat and colleagues from University Hospital of Rouen in France reported on a prospective study of 18 participants under age 15 with severe PTSD who were unresponsive to other medications. The participants were given 1 mg of prazosin at bedtime, which was increased to 3 mg in 20% of the participants. The youth were assessed weekly over a one-month period. Improvement was seen in all domains, including sleep, nightmares and daytime intrusive symptoms. Prazosin was well tolerated, with only one patient experiencing low blood pressure, which did not necessitate withdrawal from the study.
In the final poster, researcher Fatima Motiwala and colleagues reviewed the literature on the treatment of PTSD in children. Motiwala indicated that among the options, prazosin was widely used in her hospital, at doses starting at 1 mg given at bedtime and increasing to a mean of 4 mg at bedtime with excellent results and tolerability.
Editor’s Note: Although these were not double-blind controlled studies, the findings are noteworthy in that they provide consistent data on the effectiveness and tolerability of prazosin in low doses in children with PTSD, essentially mirroring controlled data in adults, where higher doses are typically required.





