Methamphetamine Kills Dopamine Neurons in the Midbrain of Mice
Epidemiological studies have linked methamphetamine use to risk of Parkinson’s disease, and animal studies of the illicit drug have shown that it harms dopamine neurons. A 2014 study by Sara Ares-Santos et al. in the journal Neuropsychopharmacology compared the effects of repeated low or medium doses to those of a single high dose on mice. Loss of dopaminergic terminals, where dopamine is released, was greatest after three injections of 10mg/kg given at three-hour intervals, followed by three injections of 5 mg/kg at three-hour intervals, and a one-time dose of 30mg/kg. All of the dosages produced similar rates of degeneration of dopamine neurons via necrosis (cell destruction) and apoptosis (cell suicide) in the substantia nigra pars compacta (the part of the brain that degenerates in Parkinson’s disease) and the striata.
Resilience Important for Mental Health
A symposium at the 2014 meeting of the American Psychiatric Association suggested that resilience may hold the key to healthy aging, and overcoming trauma and stress.
Resilience in Aging
Former APA president Dilip Jeste began the symposium with a discussion of successful aging. He noted the importance of optimism, social engagement, and wisdom (or healthy social attitudes) in aging. In a group of 83-year-olds, those with an optimistic attitude had fewer cardiovascular illnesses, less cancer, fewer pain syndromes, and lived longer. Those with high degrees of social engagement had a 50% increase in survival rate. Wisdom comprises skills such as seeing aging in a positive light, and having a memory that is biased toward the positive (the opposite of what happens in depression, where negatives are selectively recalled and remembered). Jeste encouraged psychiatrists to focus not just on the treatment of mental illness, but on behavioral change and the enhancement of wellbeing. He suggested asking patients not just, “How do you feel?” but instead, “How do you want to feel?”
Resilience in the Military
Researcher Dennis Charney gave a talk on resilience based on his work with people in the military, some of whom experienced post-traumatic stress disorder (PTSD). He cited a series of important principles that could enhance resilience. The first principle was to reframe adversity—assimilating, accepting and recovering from it. The second principle was that failure is essential to growth. The third principle was that altruism helps, as does a mission for the survivor of trauma. Charney suggested that a personal moral compass is also critical, whether this is based on religion or general moral principles. Other factors that are important for resilience include having a role model, facing one’s fears, developing coping skills, having a support network, increasing physical well-being, and training regularly and rigorously in multiple areas.
Charney and colleagues studied Navy SEALS who went through SERE (Survival, Evasion, Resistance, Escape) training. Those SEALS who had the highest resilience during this severe training exercise had the highest levels of the neurotransmitter norepinephrine and NPY (an antianxiety neuropeptide). NPY levels are low in people with PTSD. Charney and colleagues reasoned that giving a peptide that acted on the NPY-1 receptors intranasally (so that it could cross the blood brain barrier) might be therapeutic. In a rodent model of PTSD, the peptide prevented and reversed PTSD-like behaviors. Further clinical development of the peptide is now planned.
The Effects of Stress
Researcher Owen Wolkowitz described how stress accelerates the mental and physical aspects of aging. Telomeres are strands of DNA at the end of each chromosome that protect the DNA during each cell replication. Telomere length decreases with stress and aging. Read more
Lithium and Quetiapine Have Similar Efficacy in Bipolar Disorder
In a recent study comparing the efficacy of lithium and the second-generation antipsychotic quetiapine, the drugs had remarkably similar results. Researcher Andrew Nierenberg et al. presented the results at the 2014 meeting of the American Society of Clinical Psychopharmacology. In the 6-month study called CHOICE (Clinical Health Outcome Initiative Comparative Effectiveness), 482 patients received either lithium or quetiapine in addition to other medications in a manner consistent with clinical practice. For the purposes of the study, those receiving lithium could not receive quetiapine or another antipsychotic, and those receiving quetiapine could not receive lithium or another antipsychotic, but both groups could receive other types of adjunctive medications.
By the end of the 6-month study period, most patients had improved substantially, but only about a quarter of each group became truly well. The researchers suggest that patients may need a longer period of treatment or other interventions such as psychotherapy or combination treatment. Clinicians were told to use the maximum dose of lithium or quetiapine that each patient could tolerate. Mean maximum doses were 1007.5mg of lithium and 344.9mg of quetiapine.
One surprise for the researchers was that 24% of lithium patients and 27% of quetiapine patients required no other medications and improved on monotherapy.
While results were very similar for two drugs, lithium produced slightly greater side effects and produced slightly better results in patients with anxiety. This may have been due to those patients also receiving benzodiazepines, and the researchers are analyzing data to see whether the patients with anxiety did indeed receive this kind of adjunctive treatment. Quetiapine was slightly better in patients who had more manic symptoms.
In another surprise finding, patients with bipolar II disorder fared better overall than patients with bipolar I disorder. Patients with higher suicide risk did worse than those with lower suicide risk.
Traditional Antidepressants Are Not Effective in Bipolar Depression
 Bipolar illness affects 4.5% of the US population. According to researcher Kathleen Merikangas, 1.0% have bipolar I disorder, 1.1% have bipolar II disorder, and the remainder have subthreshold symptoms. Mark Frye, Chairman of the Department of Psychiatry at the Mayo Clinic, gave a lecture on antidepressants in bipolar illness at the 2014 meeting of the American Psychiatric Association.
Bipolar illness affects 4.5% of the US population. According to researcher Kathleen Merikangas, 1.0% have bipolar I disorder, 1.1% have bipolar II disorder, and the remainder have subthreshold symptoms. Mark Frye, Chairman of the Department of Psychiatry at the Mayo Clinic, gave a lecture on antidepressants in bipolar illness at the 2014 meeting of the American Psychiatric Association.
The newest data from meta-analyses indicate that traditional antidepressants that are effective in unipolar depression are not effective in bipolar depression. Some patient groups, especially those with very early onset depression and mixed depression, are at increased risk of switching into mania and making a suicide attempt while taking antidepressants.
Unipolar depressed patients with a genetic variation that produces a short form of the serotonin transporter (5HT-LPRs/s) are at increased risk for depression in adulthood following a history of childhood adversity, and tend to respond less well to antidepressants. Frye found that 5HT-LPRs/s is weakly associated with switching into mania when antidepressants are given to patients with bipolar depression.
At the same symposium, researcher Mike Gitlin reviewed data on combination therapy, which is rapidly becoming the norm, indicating that in most circumstances, it is superior to monotherapy.
Researcher David Miklowitz reviewed the impressive data on the superiority of most forms of targeted psychotherapy or psychoeducation compared to treatment as usual for bipolar depression. He noted his own finding that Family Focused Therapy (FFT) not only is effective in adolescents and adults with bipolar disorder, but also in reducing illness and dysfunction in those with prodromal disorders (such as depression, cyclothymia, and bipolar not otherwise specified) in situations where there is a family history of bipolar disorder.
Eight components of FFT are:
- Recognition of prodromal symptoms and development of treatment strategies for them.
- Recognition and management of stress and triggers using cognitive restructuring.
- Development of a relapse prevention plan and rehearsal of what to do.
- Regularization of sleep.
- Encouragement of treatment adherence with an eye to a good future.
- Enhancement of emotional self-regulation skills, including cognitive restructuring.
- Improvement of family relationships and communication.
- Education about substance abuse avoidance and treatment for that and other comorbidities.
Many of these are also key components of group psychoeducation, cognitive-behavioral therapy, and interpersonal and social rhythms therapy, and all of these are effective in treating and preventing bipolar depression compared to treatment as usual. It is noteworthy that in the research of Francesc Colom, 90% of patients randomized to treatment as usual relapsed within 24 months, while psychoeducation was highly effective in preventing relapses over the next five years.
This editor (Robert M. Post), the discussant for the symposium, emphasized that the main take-away messages of the speakers were: use more lithium, use more caution and fewer antidepressants in treating bipolar depression, use more combination therapy for acute illness and for maintenance, and definitely use more psychotherapy. Read more
Theta-burst RTMS Improved Depression
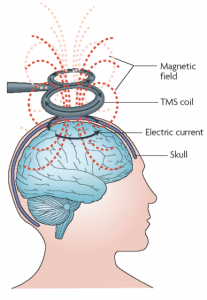 Theta-burst stimulation is a type of repeated transcranial magnetic stimulation (rTMS) currently being investigated for the treatment of severe depression. In rTMS a magnetic pulse applied to the scalp causes neurons to fire. A recent study of 60 patients by Cheng-Ta Li et al. published in the journal Brain compared continuous, intermittent, and combined theta-burst treatment with a sham treatment. While all four groups of patients with treatment-resistant depression improved, indicating some placebo effect, patients in the group who received intermittent stimulation over the left prefrontal cortex and those who received a combination of intermittent left prefrontal cortex stimulation and continuous right prefrontal stimulation showed the greatest improvement in their depression. Those patients with greater prior treatment resistance responded less well across all of the treatments.
Theta-burst stimulation is a type of repeated transcranial magnetic stimulation (rTMS) currently being investigated for the treatment of severe depression. In rTMS a magnetic pulse applied to the scalp causes neurons to fire. A recent study of 60 patients by Cheng-Ta Li et al. published in the journal Brain compared continuous, intermittent, and combined theta-burst treatment with a sham treatment. While all four groups of patients with treatment-resistant depression improved, indicating some placebo effect, patients in the group who received intermittent stimulation over the left prefrontal cortex and those who received a combination of intermittent left prefrontal cortex stimulation and continuous right prefrontal stimulation showed the greatest improvement in their depression. Those patients with greater prior treatment resistance responded less well across all of the treatments.
Editor’s Note: Studies continue to explore the optimum parameters for rTMS, but large studies and meta-analyses continue to show that the treatment has positive effects in depression.
A Re-Kindling Process Produces Late-Onset PTSD
Not everyone who experiences trauma develops post-traumatic stress disorder (PTSD) immediately. Researchers are discovering that some people go on to develop symptoms like flashbacks or intrusive thoughts, anxiety, and withdrawal, sometimes after long periods of being asymptomatic. Two studies provide hints about the mechanism of this late-onset (or delayed-type) PTSD.
In an article by Danny Horesh et al. published in the journal Psychiatry Research in 2013, a reported 16.5% of 675 Israeli veterans of the 1982 conflict with Lebanon developed late-onset PTSD after a completely non-symptomatic period. The number of deployments soldiers were sent on and the number of terror incidents they experienced within Israel after the war were correlates of the late-onset PTSD, while continuous post-war employment was a protective factor reducing late-onset PTSD.
In a study of 260 older adults (above age 60) who survived the destruction around Galveston Bay, Texas by Hurricane Ike in 2008, Robert H. Pietrzak et al. reported in the Journal of Psychiatry Research in 2013 that 5.3% developed late-onset PTSD. In this case as well, a greater number of subsequent traumatic and stressful life events (and in particular financial difficulties) was associated with late onset of PTSD. The majority of participants in Pietrzak’s study (78.7 %) had no to few PTSD symptoms, while 16.0% had chronic PTSD symptoms from the outset persisting through assessments at three months and 15 months.
Editor’s Note: These two studies reveal that upon prospective follow-up, a small but substantial group of patients (5–16%) develop a late-onset type of PTSD. Acute onset PTSD has been closely linked to new trauma in adulthood, especially following the occurrence of previous (childhood) traumas. The late-occurring variety of PTSD seems to appear after an incubation period, and appears to be closely associated with the occurrence of new traumatic events during the well interval. These new events may result in a kindling-like effect, where repetition of subthreshold stimuli come to evoke a full-blown episode. PTSD appearing after repeated traumatic experiences may operate in a similar fashion to seizures that gradually emerge following repeated electrical stimulation of the amygdala (i.e. amygdala kindling). Read more
Ketamine for Chronic PTSD
We reported in BNN Volume 17, Issue 6 in 2013 on researchers’ efforts to treat symptoms of post-traumatic stress disorder using the drug ketamine. This research by Adriana Feder et al. has now been published in the journal JAMA Psychiatry.
In the study of 41 patients with post-traumatic stress disorder, patients showed a greater reduction in symptoms 24 hours after receiving intravenous (IV) ketamine than after taking IV midazolam, a benzodiazepine used as an active placebo control because it produces anti-anxiety and sedating effects similar to ketamine’s. The patients ranged in age from 18 to 55 years of age and were free of other medication for two weeks before the study. Ketamine was also associated with reduction in depressive symptoms and with general clinical improvement, and side effects were minimal.