Psychiatric Symptoms in Childhood Linked to Struggles in Adulthood
Psychiatric illness is one of the most common health problems among children. A study by William E. Copeland and colleagues in the journal JAMA Psychiatry indicates that psychiatric symptoms and diagnoses in childhood can lead to struggles with health, the legal system, personal finances, and social functioning in early adulthood, even if the psychiatric symptoms themselves do not last.
The study included 1420 participants from 11 mostly rural counties in North Carolina, who participated in structured interviews up to six times between the ages of 9 and 16 to determine the existence of psychiatric symptoms and diagnoses. Of these, 1273 were assessed three times during young adulthood, at the ages of 19, 21, and 24–26, for any evidence of social, legal, financial, or health problems.
Participants who had had a childhood psychiatric disorder were six times more likely to have at least one adverse outcome in adulthood compared to participants with no history of psychiatric problems, and nine times more likely to have two or more adverse outcomes in adulthood. Those participants who had psychiatric symptoms that were not sufficient for a particular diagnosis were still three times more likely to have at least one adverse outcome in adulthood, and five times more likely to have at least 2 adverse outcomes. The cumulative number of psychiatric disorders to which a participant was exposed was the best predictor of adverse outcomes in adulthood.
Even moderate psychiatric problems in childhood can disrupt a person’s transition to adulthood. However, early treatment and prevention can help reduce the long-term impact of psychiatric illness. Parents of children (aged 2–12) with mood and behavioral symptoms are welcome to join the Child Network, a system for collecting weekly ratings of their children’s symptoms and displaying them longitudinally for the child’s doctor.
Childhood Maltreatment Associated with Suicide Attempts
A history of childhood maltreatment increases the risk that a person will attempt suicide. Different types of maltreatment, such as physical abuse, emotional abuse, sexual abuse, and neglect, often overlap. In a 2015 study in the Journal of Clinical Psychiatry, researcher Nicolas Hoertel and colleagues used data from an epidemiological survey of 34,653 Americans to clarify the mechanism by which maltreatment is linked to suicide risk.
Hoertel and colleagues found that childhood maltreatment in general was associated with an increased risk of attempting suicide and an earlier age at first suicide attempt. The analysis controlled for demographic characteristics and psychiatric diagnoses. Most of the risk came from effects that were shared across all the types of maltreatment. However, sexual abuse directly conferred an additional risk of suicide attempt.
In an earlier study of 648 outpatients with bipolar disorder by this editor Robert Post and colleagues (led by Gabriele Leverich), 34% had a history of suicide attempts, and these participants had a higher incidence of traumatic stressors in childhood and more stresses at illness onset than those without a history of suicide attempts. A history of sexual abuse in childhood was also linked to an increased risk of a serious suicide attempt in the earlier study, which appeared in the Journal of Clinical Psychiatry in 2003.
Treating Women During Pregnancy and Breastfeeding
A Danish working group has released guidelines for prescribing psychotropic drugs to women who are pregnant or breastfeeding. After a comprehensive review of the literature, researchers from several different Danish medical societies reported that sertraline and citalopram are the first choice among selective serotonin reuptake inhibitors (SSRIs) for depression in women who are pregnant or breastfeeding. The working group suggested that women with bipolar disorder who need a mood stabilizer because of frequent relapses could be prescribed lithium, though lithium use is associated with a small risk of cardiac abnormalities in the child. Lamotrigine may also be used, and has not been associated with any congenital abnormalities.
Valproate and carbamazepine are not recommended for use during pregnancy and breastfeeding. Use of valproate among women of child-bearing age should particularly be avoided due to several risks for the potential child. These include spina bifida and other serious congenital problems, but also severe developmental delay and loss of about 9 IQ points. Other possible treatments for bipolar disorder and schizophrenia in pregnant and breastfeeding women include olanzapine, risperidone, quetiapine, and clozapine. The data about the safety of these medications are not extensive.
The working group included members of the Danish Psychiatric Society, the Danish Society of Obstetrics and Gynecology, the Danish Paediatric Society, and the Danish Society of Clinical Pharmacology. The recommendations may be found in an article by E.R. Larsen and colleagues in a 2015 supplement to the journal Acta Psychiatrica Scandinavica.
Obesity Linked to Illness Severity
In a talk at the 2015 meeting of the International Society for Bipolar Disorder, researcher David Bond reported that 75% of patients in a study of first episode mania had unhealthy body mass indices (BMIs). Forty percent were overweight while thirty-five percent were obese. Higher weight was associated with greater illness severity. Bond said that in other studies obesity has been associated with less time well and a greater risk of relapse into depression.
Obese patients also had lower brain volume, worse memory, and a greater risk of developing early onset dementia compared to other patients. Those who were overweight or obese had a 35% higher risk of developing Alzheimer’s disease.
In a different talk at the same meeting, researcher Roger McIntyre reported that among patients with bipolar disorder, those who were obese have greater cognitive problems and more evidence of inflammation than those who were not obese. He has seen indirect antidepressant effects and other health benefits following weight loss from bariatric surgery.
Lori Altshuler, Leading Figure in American Psychiatry, 1957–2015
 We are sad to report the death of Dr. Lori Altshuler, one of the leading figures in American psychiatry. She passed away last month after a 10-year battle with cancer. She was the director of the Mood Disorders Research Program at UCLA and a founding member of the Bipolar Collaborative Network, which included US sites in Los Angeles, Dallas, Cinncinatti, and Bethesda and European sites in Utrecht, Freiberg, and Munich, and spawned the BNN newsletter.
We are sad to report the death of Dr. Lori Altshuler, one of the leading figures in American psychiatry. She passed away last month after a 10-year battle with cancer. She was the director of the Mood Disorders Research Program at UCLA and a founding member of the Bipolar Collaborative Network, which included US sites in Los Angeles, Dallas, Cinncinatti, and Bethesda and European sites in Utrecht, Freiberg, and Munich, and spawned the BNN newsletter.
Dr. Altshuler made important contributions to the understanding of bipolar disorder, particularly with her work on brain imaging. She also conducted countless treatment studies so that patients could be treated based on the best available evidence.
After funding for the Bipolar Collaborative Network ended in 2002, she organized all of the researchers to continue working together, and this resulted in more than 90 publications from the group. Her tireless and heroic efforts to improve the lives of people with bipolar disorder will be sorely missed.
Low Vitamin D Linked to Cognitive Decline
Low levels of vitamin D levels are common, particularly in older adults and in African Americans and Hispanics. Unfortunately, low vitamin D is associated with decline in two types of cognitive functioning: episodic memory (memories of autobiographical events) and executive function (reasoning, problem-solving, planning, etc.).
A recent study with a particularly diverse group of participants, over half of whom were African American or Hispanic, found that over a period of about 5 years, episodic memory and executive function declined faster in older adults with low levels of vitamin D.
Average vitamin D levels for the entire group of 382 adults were below national standards. Levels of 25-hydroxy vitamin D should be between 20 and 50 nanograms per milliliter of blood. The average fell just below this, at 19.2 ng/mL. Over a quarter of participants had vitamin D deficiency, with levels below 12 ng/mL, and another 35.1% had vitamin D insufficiency, with levels between 12 and 20 ng/mL.
African Americans and Hispanics had lower levels of vitamin D (17.9 ng/mL and 17.2 ng/mL, respectively) than whites (21.7 ng/mL). Average vitamin D levels were lower in participants with dementia compared with those who had mild cognitive impairment or normal cognitive function.
Vitamin D levels can depend on factors such as dairy intake, sun exposure, and exercise. It has not been determined whether taking vitamin D supplements could slow down cognitive decline, but vitamin D supplementation has several benefits. Compared to placebo, supplementation with vitamin D increases response to antidepressants. A high percentage of children with major psychiatric disorders are vitamin D deficient, and it is also estimated that about 40% of adults in the US have a vitamin D deficiency.
The study by researcher Joshua W. Miller and colleagues was published in the journal JAMA Neurology in September.
Benefits of a Healthy Lifestyle
 In a talk at the 2015 meeting of the International Society for Bipolar Disorder, researcher Michael Berk suggested that a healthy lifestyle may improve mood disorder symptoms.
In a talk at the 2015 meeting of the International Society for Bipolar Disorder, researcher Michael Berk suggested that a healthy lifestyle may improve mood disorder symptoms.
Diet is important. A study of more than 20,000 mothers revealed that those with unhealthy diets had children with more externalizing disorders, such as attention deficit hyperactivity disorder (ADHD), oppositional defiant disorder, and mania. Diets high in fat and sugar were linked to depression. The Nurses’ Health Study, a long-term epidemiological study of 50,000 women, showed that people who exercised more were less likely to be depressed, while lower muscle mass was associated with greater depression. Exercise also has anti-inflammatory effects.
Avoiding smoking has benefits, too. A study by Pasco and colleagues showed that people who smoke are at increased risk for a new onset of a mood disorder. Smoking is associated with onset of a more severe mood disorder earlier in life, suicide attempts, alcohol and substance abuse, and decreased response to treatment. Fortunately, quitting smoking can reverse some of these risks.
Ultrabrief Right Unilateral ECT Similar in Efficacy to Brief ECT with Fewer Side Effects
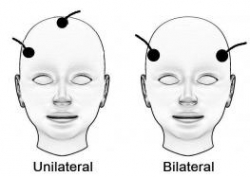 A new meta-analysis suggests that right unilateral ultrabrief electroconvulsive therapy (ECT) may be a better choice than standard brief pulse ECT for the treatment of severe depression. Researchers at the University of New South Wales in Australia led by Colleen Loo say that while standard ECT (with a pulsewidth of 1.0 ms) is recommended when urgency is paramount, ultrabrief ECT (with a pulsewidth of 0.3 ms) is better for patients at risk for cognitive side effects or those who do not require an urgent response. The researchers’ findings were reported in the Journal of Clinical Psychiatry in July.
A new meta-analysis suggests that right unilateral ultrabrief electroconvulsive therapy (ECT) may be a better choice than standard brief pulse ECT for the treatment of severe depression. Researchers at the University of New South Wales in Australia led by Colleen Loo say that while standard ECT (with a pulsewidth of 1.0 ms) is recommended when urgency is paramount, ultrabrief ECT (with a pulsewidth of 0.3 ms) is better for patients at risk for cognitive side effects or those who do not require an urgent response. The researchers’ findings were reported in the Journal of Clinical Psychiatry in July.
Loo and colleagues analyzed the findings of six different studies that compared right unilateral standard brief pulse ECT with ultrabrief pulse ECT and included a total of 689 patients. Standard ECT was more effective, producing more improvement in mood and more remissions, and working faster than ultrabrief ECT. However, standard ECT also produced greater cognitive side effects in every area tested, including thinking, learning and recall, and memory.
(When bilateral ECT is used, the cognitive effects are even worse, and researcher Harold Sacheim and colleagues have reported that the severity of the impairment in autobiographic memory is directly proportional to the number of bilateral ECT treatments a patient received, even when measured one year after the last session of bilateral ECT. This editor (Robert Post) believes bilateral ECT should be avoided if at all possible, as cognitive side effects can occasionally be severe.)
When Loo and colleagues removed nonrandomized trials from the analysis, the differences in efficacy between ultrabrief and standard right unilateral ECT were not statistically significant. Loo told Medscape Medical News that while the differences in efficacy between brief and ultrabrief ECT are minimal, the differences in side effects are greater. Right unilateral ultrabrief ECT works about as well as standard right unilateral brief pulse ECT, but preserves patients’ cognitive function better.
New TMS System Approved for Depression
In August the US Food and Drug Administration (FDA) approved the marketing of the MagVita TMS Therapy system from the company MagVenture. This machine can be used to provide transcranial magnetic stimulation (TMS) to patients with major depression that has not responded to antidepressant drugs. A TMS system uses magnets placed close to the head to stimulate the brain.
There are several existing systems that can provide TMS. The Neuronetics Neurostar TMS machine was the first one to be approved, in 2008. Then came Brainway’s Deep TMS machine. Now MagVenture says that the benefits of their new system include a simple design, low operating costs, no disposable components, and safety and efficacy rates comparable to those of other FDA-approved TMS devices.
Treatment with the MagVita system is typically provided five times per week for a duration of six weeks.
As TMS treatment becomes available to more patients, coverage by insurance companies is also increasing, but is still not guaranteed for patients in the US.
Treating Bipolar Disorder in Children and Adolescents
Bipolar disorder in childhood or adolescence can destroy academic, family, and peer relationships and increase vulnerability to drug use, unsafe sexual encounters, disability, and suicide. Treatment is critical to avoid cognitive decline. Given the potential tragic outcomes of undertreating bipolar illness, it is concerning that 40–60% of children and adolescents with bipolar disorder are not in treatment.
In a talk at the 2015 meeting of the International Society for Bipolar Disorder, researcher Cristian Zeni reviewed the existing research on the treatment of bipolar disorder in children and adolescents. A 2012 study by Geller reported response rates of 68% for the atypical antipsychotic risperidone, 35% for lithium and 24% for valproate. Risperidone was linked to weight gain and increases in prolactin, a protein secreted by the pituitary gland, while lithium was linked to more discontinuations and valproate to sedation.
For children or adolescents with aggression, researcher Robert Kowatch recommends quetiapine, aripiprazole, and risperidone. For those with a family history of bipolar disorder, he recommends lithium or alternatively, valproate plus an atypical antipsychotic.
Reseacher Robert Findling has found that lamotrigine has positive effects in childhood mania, and Duffy et al. found in a study of 21 children with mania that 13 remained stable on monotherapy with quetiapine for 40 weeks without relapse, while 5 others required combination treatment with more than one drug. In studies by Karen Wagner, oxcarbazepine was significantly better than placebo at reducing mania in younger children (ages 7–12), but not older children (13–18).
Studies by Duffy and colleagues in 2007 and 2009 recommend lithium for those with a family history of bipolar disorder, atypical antipsychotics for children with no family history of bipolar disorder, and lamotrigine for those with a family history of anxiety disorders.
In children with bipolar disorder and comorbid attention deficit hyperactivity disorder, there is universal agreement that mood should be stabilized first, and then small amounts of stimulants may be added for residual ADHD symptoms. Too often, the opposite occurs, with stimulants given prior to mood stabilization with lithium, anticonvulsants (valproate, lamotrigine, carbamazepine/oxcarbazepine) and/or an atypical antipsychotic. Read more








